 |
 |
- Search
| Ann Geriatr Med Res > Volume 27(2); 2023 > Article |
|
Abstract
Background
Falls are a major concern among hospitalized adults, and it is essential to identify high-risk patients to prevent falls. This retrospective cohort study conducted at the Asan Medical Center, Korea, compared the screening abilities of the at-point Clinical Frailty Scale (CFS) and Morse Fall Scale (MFS) to identify patients at high risk for falls among hospitalized adults.
Methods
We assessed the records of at-point CFS, MFS, and fall incidence during hospitalization of 2,028 patients aged 18 or older included in this study. We calculated the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and area under the curve (AUC) for each tool.
Results
Twenty-five patients (1.23%) experienced falls during hospitalization. The mean at-point CFS score was significantly higher in those with falls than in those without falls. The mean MFS score did not differ significantly between the two groups. The optimal cutoff points for the at-point CFS and MFS scores were 5 and 45, respectively. At these cutoffs, the at-point CFS demonstrated a sensitivity of 76.0%, specificity of 54.0%, PPV of 2.0%, and NPV of 99.4%, whereas the MFS demonstrated a sensitivity of 60.0%, specificity of 68.1%, PPV of 2.2%, and NPV of 99.4%. The AUC values for the at-point CFS and MFS were 0.68 and 0.63, respectively, with no significant difference (p=0.31).
Falls are a major concern in hospitalized patients, particularly in older adults and those with frailty.1) Falls can result in a range of negative outcomes, including fractures and head injuries, leading to longer hospital stays and significant morbidity and mortality.2) Moreover, falls can cause psychological distress, fear of falling, and a loss of confidence in oneŌĆÖs ability to move safely.2) Falls also create a significant burden on healthcare systems by increasing healthcare costs and diverting resources from other areas of care.3,4) Therefore, it is crucial to screen patients who are at high risk of falling and implement preventive measures in a hospital setting.
The Morse Fall Scale (MFS), developed in 1986, is a widely used tool in healthcare settings to assess a patientŌĆÖs risk of falling.5) It considers six factors: history of falling, current medications, mobility, mental status, presence of equipment (such as intravenous lines or catheters), and age. Each factor is assigned a score, and the total scores determine a patientŌĆÖs overall fall risk. The MFS is one of the most commonly used screening tools for high fall risk in hospitalized patients; however, the optimal cutoff value remains controversial.6,7) Furthermore, studies have shown that the screening value of MFS might be insufficient.8,9)
Falls are considered a geriatric syndrome, a condition closely related to frailty,10) which is a state of increased vulnerability and reduced physiological reserves due to the accumulation of aging processes in older adults.11,12) Numerous studies have demonstrated a higher risk of falls among hospitalized patients with frailty.13,14) Consequently, it may be logical to screen patients for frailty to more effectively predict and prevent falls. Indeed, the MFS itself includes items reflecting the spectrum of frailty, such as a history of falls, mobility, mental status, and age.
Among the tools to assess frailty, the Clinical Frailty Scale (CFS), with scores ranging from 1 (very fit) to 9 (terminally ill), has been widely used in various clinical settings.15) In acute medical conditions, the CFS is generally applied to assess a patientŌĆÖs baseline functional status 2 weeks before they fall ill.16) Meanwhile, the at-point CFS, which incorporates the baseline functional status and severity of an acute illness, can assess the health status of patients at the time of evaluation.16,17) A previous study showed that at-point CFS predicted various adverse health outcomes, such as falls, in hospitalized patients aged >65 years.17) However, despite the general applicability of frailty in younger and middle-aged adults,18,19) no study has established the efficacy of the CFS as a screening tool for falls in this population. Hence, we aimed to assess the screening ability of the at-point CFS and MFS in identifying hospitalized adults aged >18 years at high risk for falls.
This retrospective cohort study was conducted at the Asan Medical Center, a tertiary hospital in Seoul, Korea. The study included a total of 2,028 patients, consisting of 1,016 patients aged Ōēź65 years who were admitted to the general ward between May 1 and September 30, 2021 and 1,012 patients aged Ōēź18 years who were admitted to the emergency room between February and March 2022. Although the at-point CFS was measured for all patients who visited the emergency room since August 2021, the most recent data from February and March 2022 were used to increase the accuracy of the study, considering the proficiency of the emergency medical staff in CFS measurements. Patients who did not undergo at-point CFS measurements were excluded. The study protocol was approved by the Institutional Review Board of Asan Medical Center (No. 2022-0722). Written informed consent was waived as the evaluation of the general health status of patients at admission is a routine practice and no harm was expected.
This study complied the ethical guidelines for authorship and publishing in the Annals of Geriatric Medicine and Research.20)
The MFS is used to assess a patientŌĆÖs risk of falling by evaluating the presence or absence of various risk factors.5) It comprises six items: fall history, secondary diagnosis, use of ambulatory aids, intravenous therapy or heparin cap use, gait, and cognitive status related to gait. Each item was scored, with a maximum total score of 125 points. Patients with a score <45 points were considered to have a low risk of falling, whereas those with a score Ōēź45 were considered to be at high risk. The fall risk assessment using the MFS was performed at the time of admission, once daily during hospitalization, and when the patientŌĆÖs condition changed. The results of the fall risk assessments were included in electronic medical records.
The at-point CFS measurement for inpatients was performed by experienced geriatric nurses on the day after admission to the geriatric department. In the emergency room, the at-point CFS was measured by emergency room nurses. We used the Korean-translated version of the CFS 2.0 and a classification tree with established construct validity in the Korean geriatric outpatients21) and accuracy for predicting adverse outcomes in hospitalized older patients.22) The Korean-translated version of the CFS 2.0 and classification tree are described in Supplementary Figs. S1 and S2, respectively.
The fall incidence was obtained from mandatory fall reports for all falls that occurred in the hospital. This comprehensive data collection approach aimed to accurately capture and analyze the frequency and causes of falls in a hospital setting as a standard patient safety measure. Each report contained pertinent details, such as the patientŌĆÖs demographics, fall location, circumstances leading to the incident, and sustained injuries.
The data in this study were analyzed using the SPSS version 21.0 and R software version 3.6.3. The baseline characteristics of the fall and non-fall groups, including frequency, percentage, mean, and standard deviation, were described using descriptive statistics. The t-tests and chi-square tests were used to compare the two groups. The score distributions of the at-point CFS and MFS among the patients were described. We compared and analyzed the predictive ability of each tool in terms of sensitivity, specificity, and positive and negative predictive values (PPV and NPV, respectively). The area under the receiver operating characteristic (ROC) curve (AUC) was analyzed to compare the diagnostic accuracy of predicting falls and non-falls based on each toolŌĆÖs evaluation score. We determined the cutoff score for distinguishing between the fall and non-fall groups by adding the sensitivity and specificity scores in each score range and selecting the maximum value. The significance of the AUC difference between the fall risk assessment tools was analyzed using the DeLong test.
Table 1 presents the baseline characteristics of the study participants categorized according to fall events. Of the 2,028 total patients, 25 (1.23%) experienced falls during hospitalization, whereas 2,003 (99.75%) did not. Participants in the non-fall group were younger than those in the fall group; however, the difference was not statistically significant. The average length of hospitalization was significantly longer in participants with falls than in those without falls (21.12┬▒15.13 vs. 9.30┬▒10.32 days; p<0.001). The mean at-point CFS score was significantly higher in participants with falls than in those without falls (5.56┬▒1.56 vs. 4.52┬▒1.59; p<0.001). The mean MFS score did not differ significantly between the two groups (45.00┬▒19.26 vs. 38.55┬▒16.76 for those with and without falls, respectively; p=0.056).
Tables 2 and 3 show the distributions of the at-point CFS and MFS scores. The at-point CFS scores with the highest frequency of falls were 6 points with six falls (24.0%), followed by 7 points with six falls (24.0%), and 5 points with five falls (20.0%). In the fall group, the MFS scores with the highest frequency of falls were 41ŌĆō50 points with 10 falls (40.0%), followed by 31ŌĆō40 points with six falls (24.0%), and Ōēż20 points with three falls (12.0%). Using a cutoff score of 45 points, 17 patients (68.0% of the total subjects with fall events) had a score of Ōēż45 points.
For the at-point CFS, the sensitivity, specificity, PPV, and NPV were 84.0%, 35.4%, 1.6%, and 99.4% at a cutoff score of 4 and 76.0%, 54.0%, 2.0%, and 99.4% at a cutoff score of 5, respectively. Based on the optimal cutoff score determined by the sum of sensitivity and specificity presented in the ROC analysis, the optimal cutoff score for the at-point CFS was 5. For the MFS, the cutoff score of 45 points proposed by the original author during tool development showed a sensitivity of 60.0%, specificity of 68.1%, PPV of 2.2%, and NPV of 99.4%; thus, the optimal cutoff score in this study was retained at 45 points (Table 4).
The optimal cutoff points, which were determined by the maximal points of the sums of sensitivity and specificity, for the at-point CFS and MFS were 5 and 45, respectively. The AUC value of at-point CFS was higher than that of MFS (0.68 and 0.63, respectively), although not statistically significant (p=0.31) (Fig. 1). After excluding participants aged <60 years, the AUC value of the at-point CFS was still higher than that of the MFS (0.65 and 0.61, respectively), although also without statistical significance (p=0.52) (Supplementary Fig. S3). Considering the potential impact of measurement reliability on the results, we conducted subgroup analyses based on the groups measured by emergency room nurses and experienced geriatric nurses. The AUC values for at-point CFS and MFS in the group measured by emergency room nurses, were 0.62 and 0.54, respectively, whereas in the group measured by experienced geriatric nurses, the AUC values were 0.76 and 0.77, respectively. Supplementary Fig. S4 shows the corresponding ROC curves for reference.
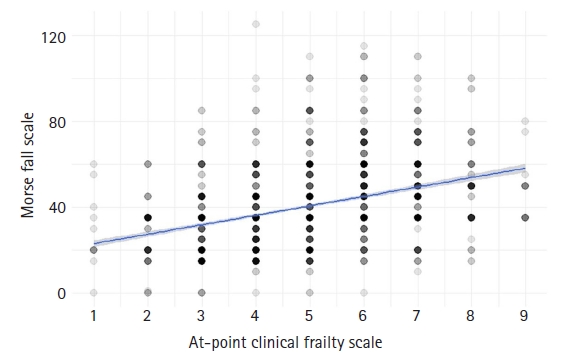
We observed a significant association between the at-point CFS and MFS. The standardized beta coefficient was 2.76, indicating a strong positive relationship between the two variables (p<0.001). Additionally, the R2 value was 0.17. Fig. 2 presents a point plot and linear regression depicting this association.
In this comparative study, we aimed to assess the screening ability of the at-point CFS and MFS to identify hospitalized adults with high risk of falls. We found optimal cutoff points of 5 and 45 for the at-point CFS and MFS, respectively. Although the at-point CFS had higher explanatory power than the MFS, the AUC values did not differ significantly between the two tools. To our knowledge, this is the first study to compare the screening values of the at-point CFS and MFS in an acute-care hospital.
In this study, we used the at-point CFS, which is different from the original CFS that reflect baseline health status. However, our findings are consistent with those of previous studies that reported the optimal cutoff point for CFS in determining frailty status.23) Our current observations are also concordant with our previous report showing that a cutoff point of 5 for the at-point CFS can predict various geriatric adverse events such as pressure ulcers, delirium, longer duration of hospitalization, unexpected emergency department visits after discharge, and institutionalization after discharge in hospitalized patients aged Ōēź65 years.17) This consistency lends further credibility to our results and suggests that the at-point CFS may serve as a useful tool for predicting fall risk among hospitalized adults.
Falls are the result of a complex system failure rather than a single cause, making them a component of geriatric syndromes, which are multifactorial health conditions that arise from accumulated impairments in multiple systems.10,24) Frailty is a common and important geriatric syndrome that is closely associated with falls.25) Physical frailty, characterized by a decline in physical function and muscle strength, can lead to a loss of balance and increased risk of falls.26) Furthermore, falls are often a consequence of the inability to perform multiple tasks due to cognitive decline and inability to integrate sensory inputs.24) Polypharmacy, another phenotype that reflects deficits in systemic integrity, is also an important risk factor for falls.27) Various studies have demonstrated that frailty is an important risk factor for falls among different populations.26,28,29) Hence, falls result from a systemic failure, a concept that may be applicable not only to older adults but also to younger populations.
The CFS is a simple and rapid tool for assessing frailty and has shown promising results in predicting falls. Church et al.23) showed the predictive ability of CFS in 71% of fall cases in a scoping review. Hatcher et al.30) demonstrated that the CFS score at admission predicted readmission for falls after trauma-related injuries. The Center for Effective Practice recommends the CFS as a screening tool to evaluate the risk of falls in community-dwelling adults.31) Jung et al.17) showed that an at-point CFS Ōēź5 was associated with an increased risk of falls, with an odds ratio of 1.74 in older hospitalized patients. However, none of the studies utilized the at-point CFS in acute medical conditions in populations including young adults.
The MFS is a tool commonly used to assess fall risk among hospitalized patients; however, it has several limitations compared to those of the CFS. One major advantage of the CFS is because it was initially developed to evaluate frailty, it can predict a wide range of geriatric syndromes other than falls, including outcomes such as delirium and pressure ulcers.17,23,32) In contrast, the MFS measures only the risk of falls, although some of its components include a range of frailties, such as a history of falls and cognitive function. Another limitation of the MFS is the burden to ask six questions to every individual, whereas the CFS requires only one question. Furthermore, the accuracy and cutoff score of the MFS are controversial, as previous studies have shown mixed results.8,9)
One of the key strengths of this study was its comparative approach, which allowed for a more comprehensive assessment of the at-point CFS and MFS to identify hospitalized adults with a high risk of falls. To our knowledge, this is the first study to compare the screening values of the two assessment tools in an acute-care hospital setting, making the result an important contribution to the existing literature. Furthermore, our findings are consistent with previous research on the optimal CFS cutoff points for determining frailty status, providing further support for the at-point CFS as a valuable screening tool for fall risk. Additionally, our study builds on prior research by demonstrating the ability of the at-point CFS to predict various geriatric adverse events, further highlighting its potential clinical utility.
Despite its strengths, our study had several limitations. First, this study was conducted in a single acute-care hospital, which might limit the generalizability of our results to other healthcare settings and patient populations. Second, although we found no significant differences in AUC values between the assessment tools, the sample size might not have been sufficient to detect subtle differences in their predictive abilities. Third, our study did not evaluate other potentially relevant risk factors of fall such as clinical, environmental, or situational factors, which could have provided additional insights into the most effective strategies for fall prevention and intervention. Fourth, only two participants aged <60 years experienced falls, which might appear insufficient. However, as younger patients are less prone to falls, this situation was unavoidable. As shown in Supplementary Fig. S3, the exclusion of younger participants from the analysis did not affect the overall results. Finally, the inclusion of two distinct groups assessed by emergency room nurses and experienced geriatric nurses could potentially affect the reliability of the at-point CFS measurement. However, the results of the subgroup analysis comparing these two groups showed that this factor did not significantly affect the main results. Nonetheless, further investigations are needed in future studies.
In conclusion, the results of our study demonstrated that the at-point CFS is an effective tool for identifying fall risk among hospitalized adults, with a performance comparable to that of the MFS. Therefore, the at-point CFS may be a valid screening tool for fall risk in hospitalized adults.
ACKNOWLEDGMENTS
FUNDING
We thank the Asan Multidisciplinary Committee for Seniors (AMCS) and Ministry of Health and Welfare (Research-driven Hospitals, HR20C0026) for their support and funding throughout this research project. The members of the AMCS are listed in Supplementary Table S1.
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via https://doi.org/10.4235/agmr.23.0057.
Table┬ĀS1.
List of the members of the Asan Multidisciplinary Committee for Seniors
Fig.┬ĀS1.
The Korean-translated version of the Clinical Frailty Scale 2.0.
Fig.┬ĀS2.
The Clinical Frailty Scale classification tree. Adapted from Jung et al. Operationalization of the Clinical Frailty Scale in Korean community-dwelling older people. Front Med 2022;9:880511. https://doi.org/10.3389/fmed.2022.880511.
Fig.┬ĀS3.
Receiver operating characteristic curve for the fall risk assessment tool among participants aged 60 or more. CFS, Clinical Frailty Scale; MFS, Morse Fall Scale; AUC, area under the curve.
Fig.┬ĀS4.
Receiver operating characteristic curve for the fall risk assessment tool according to the evaluator. (A) Participants whose CFS was measured by emergency room nurses. (B) Participants whose MFS was measured by experienced geriatric nurses. CFS, Clinical Frailty Scale; MFS, Morse Fall Scale; AUC, area under the curve.
Fig.┬Ā1.
Receiver operating characteristic curve for the fall risk assessment tool. CFS, Clinical Frailty Scale; MFS, Morse Fall Scale; AUC, area under the curve.
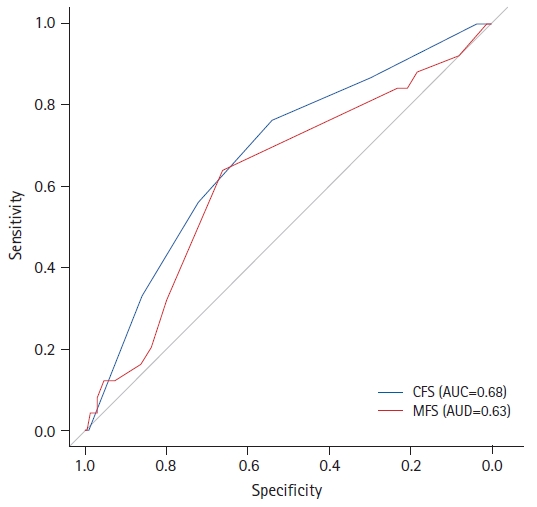
Fig.┬Ā2.
Point plot and linear regression between the at-point Clinical Frailty Scale and Morse Fall Scale.
Table┬Ā1.
Baseline characteristics of the participants
Table┬Ā2.
At-point CFS score distribution of the participants
Table┬Ā3.
MFS score distribution of the participants
Table┬Ā4.
Comparison of sensitivity, specificity, PPV, NPV, and AUC for the fall risk assessment tool
REFERENCES
2. Sato N, Hase N, Osaka A, Sairyo K, Katoh S. Falls among hospitalized patients in an acute care hospital: analyses of incident reports. J Med Invest 2018;65:81ŌĆō4.


3. Kang YO, Song R. Effects of fall prevention education program on attitudes, prevention behaviors, and satisfaction among elderly inpatients. Korean J Adult Nurs 2018;30:49ŌĆō59.


4. Gulwadi GB, Calkins MP. The impact of healthcare environmental design on patient falls. Concord, CA: The Center for Health Design; 2008.
5. Morse JM, Black C, Oberle K, Donahue P. A prospective study to identify the fall-prone patient. Soc Sci Med 1989;28:81ŌĆō6.


6. Bagui S, Long T, Bagui S. Selecting the optimal Morse Falls Scale cut-off point for patient fall risk. Health 2019;11:924ŌĆō31.


7. Schwendimann R, De Geest S, Milisen K. Evaluation of the Morse Fall Scale in hospitalised patients. Age Ageing 2006;35:311ŌĆō3.


8. Kim YS, Choi-Kwon S. Fall risk factors and fall risk assessment of inpatients. Korean J Adult Nurs 2013;25:74ŌĆō82.


9. Lee YS, Choi EJ, Kim YH, Park HA. Factors influencing falls in high- and low-risk patients in a tertiary hospital in Korea. J Patient Saf 2020;16:e376ŌĆō82.



10. Nowak A, Hubbard RE. Falls and frailty: lessons from complex systems. J R Soc Med 2009;102:98ŌĆō102.




11. Fried LP, Cohen AA, Xue QL, Walston J, Bandeen-Roche K, Varadhan R. The physical frailty syndrome as a transition from homeostatic symphony to cacophony. Nat Aging 2021;1:36ŌĆō46.




12. Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet 2013;381:752ŌĆō62.



13. Lan X, Li H, Wang Z, Chen Y. Frailty as a predictor of future falls in hospitalized patients: a systematic review and meta-analysis. Geriatr Nurs 2020;41:69ŌĆō74.


14. Liu Z, Wang Q, Zhi T, Zhu Y, Wang Y, Wang Z, et al. Frailty index and its relation to falls and overnight hospitalizations in elderly Chinese people: a population-based study. J Nutr Health Aging 2016;20:561ŌĆō8.



15. Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005;173:489ŌĆō95.



16. Rockwood K, Theou O. Using the Clinical Frailty Scale in allocating scarce health care resources. Can Geriatr J 2020;23:210ŌĆō5.




17. Jung HW, Baek JY, Kwon YH, Jang IY, Kim DY, Kwon HS, et al. At-point Clinical Frailty Scale as a universal risk tool for older inpatients in acute hospital: a cohort study. Front Med (Lausanne) 2022;9:929555.



18. Loecker C, Schmaderer M, Zimmerman L. Frailty in young and middle-aged adults: an integrative review. J Frailty Aging 2021;10:327ŌĆō33.


19. Jang AR, Sagong H, Yoon JY. Frailty trajectory among community-dwelling middle-aged and older adults in Korea: evidence from the Korean Longitudinal Study of Aging. BMC Geriatr 2022;22:524.




20. Noh JH, Jung HW, Ga H, Lim JY. Ethical guidelines for publishing in the Annals of Geriatric Medicine and Research. Ann Geriatr Med Res 2022;26:1ŌĆō3.




21. Jung HW, Jang IY, Back JY, Park S, Park CM, Han SJ, et al. Validity of the Clinical Frailty Scale in Korean older patients at a geriatric clinic. Korean J Intern Med 2021;36:1242ŌĆō50.




22. Han SJ, Jung HW, Lee JH, Lim J, Moon SD, Yoon SW, et al. Clinical Frailty Scale, K-FRAIL questionnaire, and clinical outcomes in an acute hospitalist unit in Korea. Korean J Intern Med 2021;36:1233ŌĆō41.




23. Church S, Rogers E, Rockwood K, Theou O. A scoping review of the Clinical Frailty Scale. BMC Geriatr 2020;20:393.




24. Tinetti ME, Inouye SK, Gill TM, Doucette JT. Shared risk factors for falls, incontinence, and functional dependence: unifying the approach to geriatric syndromes. JAMA 1995;273:1348ŌĆō53.


26. Chittrakul J, Siviroj P, Sungkarat S, Sapbamrer R. Physical frailty and fall risk in community-dwelling older adults: a cross-sectional study. J Aging Res 2020;2020:3964973.




27. Ming Y, Zecevic A. Medications & polypharmacy influence on recurrent fallers in community: a systematic review. Can Geriatr J 2018;21:14ŌĆō25.




28. Ensrud KE, Ewing SK, Taylor BC, Fink HA, Stone KL, Cauley JA, et al. Frailty and risk of falls, fracture, and mortality in older women: the study of osteoporotic fractures. J Gerontol A Biol Sci Med Sci 2007;62:744ŌĆō51.


29. Speciale S, Turco R, Magnifico F, Bellelli G, Trabucchi M. Frailty is the main predictor of falls in elderly patients undergoing rehabilitation training. Age Ageing 2004;33:84ŌĆō5.

30. Hatcher VH, Galet C, Lilienthal M, Skeete DA, Romanowski KS. Association of clinical frailty scores with hospital readmission for falls after index admission for trauma-related injury. JAMA Netw Open 2019;2:e1912409.



31. Center for Effective Practice. Falls prevention and management [Internet]. Toronto, Canada: Center for Effective Practice; 2021 [cited 2023 Jun 10]. Available from: https://tools.cep.health/tool/falls-prevention-and-management/.







