 |
 |
- Search
| Ann Geriatr Med Res > Volume 27(4); 2023 > Article |
|
Abstract
In the face of an ever-increasing wave of an aging population, this paper provides an update on the current status of geriatric medicine in Korea, comparing it with global initiatives and suggesting future directions. Older adults require a multifaceted approach, addressing not only comorbidity management but also unmet complex medical needs, nutrition, and exercise to prevent functional decline. In this regard, the World Health Organization's Integrated Care for Older People guidelines underscore the importance of patient-centered primary care in preventing a decline in intrinsic capacity. Despite these societal needs and the ongoing aging process, the healthcare system in Korea has yet to show significant movement or a shift toward geriatric medicine, further complicated by the absence of a primary care system. We further explore global efforts in establishing age-integrative patient-centered medical systems in Singapore, Australia, Canada, the United Kingdom, and Japan. Additionally, we review the unmet needs and social issues that Korean society is currently facing, and local efforts by both government and a private tertiary hospital in Korea. In conclusion, considering the current situation, we propose that the framework of geriatric medicine should form the foundation of the future healthcare system.
Despite the relentless march of time and the ever-increasing wave of an aging population, South Korea's commitment to geriatric medicine remains disappointingly static. As we step into 2024, a sobering reflection on the past 5 years reveals a concerning paradox: while the number of older adults in need of specialized or complex care has grown, the systemic support for geriatric medicine has not kept pace. In this article, we update the widening unfilled gap in establishing geriatric medicine in Korea, from the 2018 article calling the Korean healthcare system to urgently adopt the concept of geriatrics.1)
Over the last half-decade, the promise of institutional support for geriatric medicine in Korea has largely remained unfulfilled. The healthcare system continues to grapple with the same challenges it faced in 2018, with no significant policy advancements or shifts in funding to bolster this critical area.2) This stagnation is not just a missed opportunity but a growing liability as the older population burgeons, bringing with it complex health needs that demand specialized attention. Currently, while there is discussion about the lack of essential healthcare services such as pediatrics, obstetrics, and emergency care, paradoxically, the need for primary care and geriatric medicine, which are considered fundamental in healthcare systems worldwide, is conspicuously absent from policy discussions in Korea. This perspective by policymakers fails to recognize the critical importance of these areas, particularly in the context of an aging society that requires dedicated attention to the unique health challenges faced by older adults.
Geriatric medicine fundamentally recognizes the diversity and complexity in the health status of older adults, acknowledging the significant variability in disease burden and physical capabilities within this demographic. This field draws parallels with pediatrics by emphasizing the unique physiological differences in its patient group, understanding that older individuals are not merely adults of an advanced age.3) Geriatricians consider the often limited applicability of clinical trial results, which are typically based on younger populations,4) to their multifaceted patient base suffering from multiple chronic conditions and physical impairments. This approach necessitates a comprehensive, patient-centered strategy that encompasses a variety of healthcare settings, from acute hospital care to long-term community-based assistance.5) In managing these diverse health needs, geriatric care often involves collaboration across medical specialties and diverse healthcare professionals. Through a holistic and individualized geriatric approach, tailored treatment plans can be developed that cater to the specific requirements of each patient, ultimately providing optimal, proactive, and multifaceted interventions that enhance and preserve intrinsic capacity.
The World Health Organization's Integrated Care for Older People (ICOPE) guidelines urge primary healthcare systems to uptake the basic geriatric concepts, proactively identify and manage geriatric syndromes and frailty, emphasizing the need to prevent the decline of intrinsic capacity in older adults. The guidelines also recognize primary entrance points for community-based interventions and support. These guidelines represent a global consensus on the importance of primary care in the holistic management of aging populations, focusing on prevention and early intervention.5)
However, in stark contrast to these international standards, South Korea's primary care system remains in a nascent and unsettled state. Despite the urgency highlighted by the World Health Organization, the Korean healthcare framework has not yet established a robust primary care system that can effectively address the nuances of geriatric health. The underdevelopment of primary care in Korea has far-reaching consequences. Without a strong primary care foundation, the early detection and management of geriatric conditions are significantly hampered. Due to the lack of basic geriatric medicine services, even fundamental geriatric syndromes in the community are often addressed through fragmented care across multiple specialized departments. This fragmentation often leads to a prescribing cascade, where the accumulation of various medications can inadvertently result in further functional decline among the older populations.6) This situation not only undermines the health and wellbeing of older adults but also leads to increased healthcare costs and resource utilization. The current gap is particularly alarming given the rapid aging of the Korean population and the increasing prevalence of geriatric syndromes and frailty among older adults.
In stark contrast to Korea's static approach, other nations have made strides in geriatric care, adapting to the needs of their aging populations with innovative policies and practices.
Singapore, in response to its rapidly aging population and the accompanying healthcare challenges, has undertaken systemic reforms to create a more integrated, patient-centric, and health-centered healthcare system.7-9) Recognizing the limitations of traditional, fragmented healthcare models, Singapore reorganized its healthcare into Regional Health Systems (RHSs), incorporating acute general hospitals, community hospitals, nursing homes, and other care providers. This reorganization aims to provide seamless, holistic care across different stages of a patient's healthcare journey, from diagnosis to post-discharge follow-up. Special emphasis is placed on community initiatives, such as Wellness Kampungs and Dementia-Friendly Communities, to support aging-in-place and enhance the quality of life for older adults and their caregivers. Initiatives like Project Care and Geriatric Surgical Services focus on reducing unnecessary hospital admissions and improving care for older patients. Transitional care services and Ageing-in-Place Community Care Teams ensure continuous support post-discharge, optimizing the use of hospital resources and reducing readmissions. Overall, these efforts exemplify a shift towards a sustainable, evidence-based approach in healthcare delivery, prioritizing function and intrinsic capacity over disease-focused care.7)
In Australia, the aged care system had faced challenges due to fragmentation and the impact of government policies promoting deregulation and market forces in aged care. This approach came under scrutiny in the Royal Commission into Aged Care Quality and Safety, which documented widespread substandard care across various levels.10) Despite these policy challenges, there has been a positive development in the field of geriatric medicine in Australia. Geriatricians have been instrumental in expanding medical services and interventions targeting specific issues such as dementia, falls, polypharmacy, and orthogeriatrics. The number of academic geriatricians and other aged care health professionals is on the rise. The training for specialist geriatricians now includes a significant research component, reflecting a commitment to advancing the field through both practical application and academic inquiry.10)
Since its accreditation by the Royal College in 1977, Geriatric Medicine in Canada has evolved, encompassing a range of clinical, educational, and research activities.11) This growth has spurred public and governmental awareness about the need for specialized geriatric services. Canadian geriatricians have become influential in healthcare leadership, contributing to the development of age-friendly hospitals and the implementation of Acute Care for the Elders (ACE) units. These units focus on providing patient-centered care and addressing the unique needs of a vulnerable older population.11)
In the United Kingdom, geriatrics is recognized as a distinct medical specialty, akin to pediatrics, with approximately 12% of physicians specializing in geriatric care. Geriatricians address both acute and chronic health issues, as well as manage geriatric syndromes and disabilities. The foundation of geriatric clinics is a patient-centered, holistic approach, and geriatricians provide continuous, personalized care not only in clinics but also in settings such as the emergency department, in-hospitals, and hospice care.12)
In Japan, starting in 2005, the Community-based Integrated Care System was established.13-15) It consists of five key components: housing, medical care, long-term care, preventive care, and daily living support. In this system, the framework of geriatric medicine is embedded to provide person-centered healthcare and welfare service. At the center of this system are patients and their families, with coordination facilitated by a manager. These five elements work together in harmony. In terms of medical care, there is a comprehensive range from acute care hospitals to chronic hospitals, including rehabilitation facilities and primary care services. A primary goal of this system is to prevent long-term care needs and functional decline.
Each country possesses its own age-integrated patient-centered system that encompasses not only medical care but also social support and nursing care. These global examples offer valuable lessons that Korea could draw from, ranging from integrated care models to improved training and support for geriatric specialists. The reluctance to embrace such strategies in Korea is not just a lack of innovation but a disregard for global best practices that could reshape the landscape of geriatric care. There are several needs and issues that Korean society is currently facing.
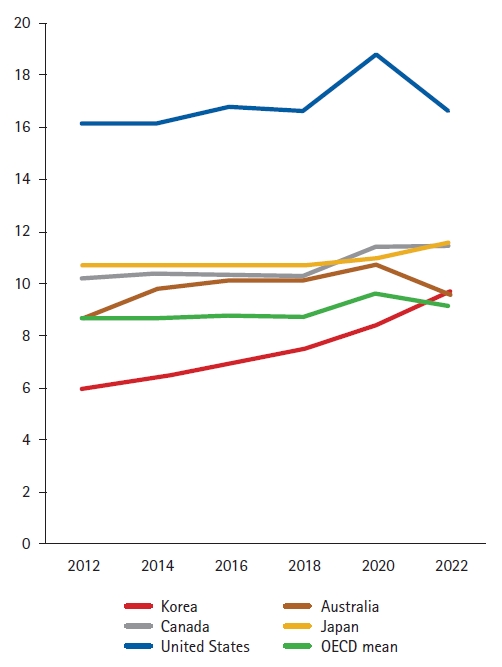
First, healthcare expenses are escalating rapidly. According to Health Statistics 2023 from the Organization for Economic Co-operation and Development (OECD), the expenditure on health compared as a percentage of gross domestic product (GDP) in 2022 was 9.7%, which turns higher than OECD mean (9.2%), and the increasing rate is notably faster compared with other OECD countries (Fig. 1). Analyzing Fig. 1, with the current Korean medical system and the changing population structure, the surge in the social burden of medical expenses is inevitable and necessitating radical changes in the medical system.
Second, there is lack of a care transition system encompassing transitions within tertiary medical institutions, local healthcare facilities, and long-term care institutions.16) In such a system, while the treatment of diseases may be possible, preventing functional decline and promoting functional recovery may not be achievable. Care transitions encompass all shifts within healthcare settings, involving not only the shifting location of care but also patient-centered, multidisciplinary medical services such as communication, home visits, primary care, and follow-up.16) In Korea, many services are absent, and if they exist, the systems are fragmented. For example, Korean Long-Term Care Insurance (LTCI) only covers existing care needs without emphasizing prevention and medical coordination. Even though frail older adults are prone to hospitalization-associated disability,17-19) LTCI does not address caregiving issues in post-acute care. Consequently, Korean systems fail to prevent the progression from frailty to disability, leading to a continuous increase in caregiving costs in Korea.20)
Third, with increasing number of older adults and disease-oriented healthcare system, multimorbidity and polypharmacy are inevitable.21) Moreover, disease-specific medical practices are prone to prescription cascade.22) Research based on 2018 National Health Insurance Data indicates that 35.9% of older adults aged 65 years or older are taking five or more medications. Among them, 44.7% have potential inappropriate medications, and 30.6% have duplicate prescriptions of the same ingredient on the same date from different institutions.23) Furthermore, older adults with more prescription had worse outcomes including mortality, adverse medication effects, increased medical expenses, and lower quality of life.23-25) Addressing these issues requires a patient-centered comprehensive geriatric approach that considers the all medical histories and unmet medical needs and provides appropriate medical interventions. However, in the Korean medical system, lacking an appropriate reimbursement system, such practices are challenging to implement. Unless there is fundamental shift from diagnostic test or procedure focused reimbursement system, it appears challenging the so-called “3-minute medical consultations” to improve in the future.
One of the local efforts may include the example of a tertiary hospital, which achieved committed to care excellence designation of the age-friendly health system in Korea, as demonstrated in a recent studies.26,27) This example highlighted the effectiveness of the Clinical Frailty Scale (CFS), which evaluates the functional status of patients within 24 hours of acute hospital admission, in predicting geriatric outcomes like falls, pressure ulcers, and delirium, as well as general hospital outcomes including death, emergency visits, and readmissions. The tertiary has been integrating the at-point CFS into its electronic health records.27) This integration is part of their initiative to adopt the 4M framework (matter, mentation, medication, and mobility) in developing an acute care pathway for older adults. This approach is aimed at providing efficient, person-centered geriatric interventions within their large-scale hospital environment. However, this system operates without any government support or payment structure. In Korea, there is a pressing need to integrate an age-friendly healthcare system that spans downstream service provision, striving to harmonize the integration of disease management, functional considerations, and caregiving demands.
The polypharmacy management project in Korea, initiated in 2018 by the National Health Insurance Service, is designed to manage the use of multiple medications, particularly in the aging population. The purpose is to review and organize these medications to prevent side effects associated with polypharmacy. Its hospital mode, initiated in 2020, has seen substantial growth. Initially starting with just seven hospitals, the initiative has grown about sevenfold in four years, with 36 hospitals participating last year and increasing to 48 this year. The project targets inpatients and outpatients for multiple drug management services. The rapid expansion of participating institutions is attributed to both online and offline regional meetings aimed at promoting the project and encouraging participation from local medical institutions. The project is organized into two models: the inpatient/outpatient model and the outpatient model, with each participating hospital potentially operating different models. The core service constitutes a multidisciplinary team of pharmacists, doctors, and nurses managing polypharmacy in chronic disease patients.
Korea’s Primary Healthcare Home Visit Fee Pilot Project, launched in December 2019, has been extended ever since, as 526 medical institutions and 696 doctors have registered for the project, with actual claims made by 142 institutions and 185 doctors in 2023. Despite the project's growth, the participation rate among all medical institutions remains low at 0.4%, and the patient utilization rate is only 1.9% when calculated to the estimated adult population who have difficulty moving and could benefit from such services.28) Despite these individual initiatives, there remains a fundamental lack in the foundation of primary healthcare providing geriatric medical services. This gap highlights the need for a more systemic approach to address the healthcare requirements of the aging population.
Several potential solutions can contribute to the integration of a geriatric perspective into our society. First, the establishment of geriatric specialists and the implementation of a comprehensive training system are imperative. This training should extend not only to physicians but also to paramedics, social workers, and policymakers, fostering an understanding of geriatric concepts. The need for manpower extends beyond geriatric clinics, encompassing policymaking and evidence generation. An initial step towards a robust geriatric training system would be the official recognition of geriatrics as a subspecialty or specialty. Second, there is a necessity to reform the medical delivery system and reimbursement structures to effectively deliver ICOPE. The current system, which often lacks a primary care focus, falls short in preventing the functional decline of older adults. Third, an organized care transition system from tertiary hospitals to local clinics or long-term care facilities should be promoted and incentivized through appropriate reimbursement. Lastly, a paradigm shift is needed where frailty and intrinsic capacity take center stage in the care system, superseding the reliance on chronological age and specific diseases. This holistic approach ensures that the care system addresses the unique needs of older adults, fostering a healthier and more resilient aging population.
This update serves as a clarion call for immediate action. Policymakers must recognize the importance of geriatric medicine, aligning it with the country's demographic reality. This call extends to increased funding, policy reform, and a public awareness campaign to elevate the importance of geriatric care in the national consciousness. In light of the systemic inertia, exploring alternative solutions becomes imperative. Community-driven initiatives, private sector innovations, and technology-driven approaches could offer some respite. However, without substantial changes, the future of geriatric care in Korea appears grim. The increasing older population, coupled with inadequate healthcare support, forecasts a crisis that could strain the healthcare system to its breaking point. The need for urgent reform is clear: Korea must embrace the concept of geriatric medicine not just as a specialty but as a foundational pillar of its healthcare system, adapting to the realities of its aging society.
ACKNOWLEDGMENTS
Fig. 1.
Expenditure on health compared to gross domestic product (GDP) of OECD countries (percentage). Source: OECD Stats (December 2023), Health Expenditure and Financing, https://stats.oecd.org/Index.aspx?DataSetCode=SHA.
REFERENCES
1. Jung HW, Lim JY. Geriatric medicine, an underrecognized solution of precision medicine for older adults in Korea. Ann Geriatr Med Res 2018;22:157–8.



2. Lee Y, Kim S, Hwang N, Im J, Joo B, Namgung E, et al. Examining the status of the older adults in 2020. Sejong, Korea: Korea Institute for Health and Social Affairs; 2020.
5. Cesari M, Sumi Y, Han ZA, Perracini M, Jang H, Briggs A, et al. Implementing care for healthy ageing. BMJ Glob Health 2022;7:e007778.



6. Sternberg SA, Guy-Alfandary S, Rochon PA. Prescribing cascades in older adults. CMAJ 2021;193:E215.



7. Lim WS, Wong SF, Leong I, Choo P, Pang WS. Forging a frailty-ready healthcare system to meet population ageing. Int J Environ Res Public Health 2017;14:1448.



8. Tan CC, Lam CS, Matchar DB, Zee YK, Wong JE. Singapore's health-care system: key features, challenges, and shifts. Lancet 2021;398:1091–104.


9. Lim WS, Wong CH, Ding YY, Rockwood K, Lien C. Translating the science of frailty in Singapore: results from the national frailty consensus discussion. Ann Acad Med Singap 2019;48:25–31.


10. Le Couteur DG, Flicker L, Hilmer SN. Geriatric medicine and health care for older people in Australia. Age Ageing 2022;51:afac001.


11. Madden KM, Wong RY. The health of geriatrics in Canada: more than meets the eye. Can Geriatr J 2013;16:1–2.




12. Oliver D, Burns E. Geriatric medicine and geriatricians in the UK: how they relate to acute and general internal medicine and what the future might hold? Future Hosp J 2016;3:49–54.



13. Song P, Tang W. The community-based integrated care system in Japan: health care and nursing care challenges posed by super-aged society. Biosci Trends 2019;13:279–81.


14. Hatano Y, Matsumoto M, Okita M, Inoue K, Takeuchi K, Tsutsui T, et al. The vanguard of community-based Integrated Care in Japan: the effect of a rural town on national policy. Int J Integr Care 2017;17:2.



15. Tsutsui T. Implementation process and challenges for the community-based integrated care system in Japan. Int J Integr Care 2014;14:e002.



16. Mansukhani RP, Bridgeman MB, Candelario D, Eckert LJ. Exploring transitional care: evidence-based strategies for improving provider communication and reducing readmissions. P T 2015;40:690–4.


17. Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated disability: "She was probably able to ambulate, but I'm not sure". JAMA 2011;306:1782–93.


18. Chodos AH, Kushel MB, Greysen SR, Guzman D, Kessell ER, Sarkar U, et al. Hospitalization-associated disability in adults admitted to a safety-net hospital. J Gen Intern Med 2015;30:1765–72.




19. Park CM, Kim W, Rhim HC, Lee ES, Kim JH, Cho KH, et al. Frailty and hospitalization-associated disability after pneumonia: a prospective cohort study. BMC Geriatr 2021;21:111.




20. Joo H. Recognition of 1 million long-term care insurance beneficiaries for the elderly [Internet]. Seoul, Korea: akomnews.com; 2023 [cited 2023 Dec 27]. Available from: https://www.akomnews.com/bbs/board.php?bo_table=news&wr_id=54335.
21. Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 2012;380:37–43.


22. Tinetti ME, Bogardus ST, Agostini JV. Potential pitfalls of disease-specific guidelines for patients with multiple conditions. N Engl J Med 2004;351:2870–4.


23. Jang T, Kim D, Park H, Lee C, Jeon E, Park Y, et al. A study on the medication prescribing patterns, underlying conditions, and prognosis of polypharmacy users using national health insurance data [Internet]. Goyang, Korea: National Health Insurance Service Ilsan Hospital; 2019.
24. Kim D, Yoon S, Jo H, Chae J, Lee J, Jeon G. Strategies for handling polypharmacy in the older adults. Wonju, Korea: Health Insurance Review & Assessment Service; 2022.
25. Yoon S, Kim D, Chae J, Choi Y, Jo H. Guidelines for the management of inappropriate polypharmacy in the older adults. Wonju, Korea: Health Insurance Review & Assessment Service; 2023.
26. Yi Y, Lee Y, Kang S, Kwon YH, Seo YM, Baek JY, et al. Unmet needs and barriers in providing hospital care for older adults: a qualitative study using the age-friendly health system framework. Clin Interv Aging 2023;18:1321–32.




27. Jung HW, Baek JY, Kwon YH, Jang IY, Kim DY, Kwon HS, et al. At-point clinical frailty scale as a universal risk tool for older inpatients in acute hospital: a cohort study. Front Med (Lausanne) 2022;9:929555.



28. Hong W. Extension of the pilot project for primary healthcare visits by another 3 years [Internet]. Seoul, Korea: doctorsnews.co.kr; 2022 [cited 2023 Dec 27]. Available from: https://www.doctorsnews.co.kr/news/articleView.html?idxno=147694.
- TOOLS







