|
 |
- Search
| Ann Geriatr Med Res > Volume 28(1); 2024 > Article |
|
Abstract
Background
Challenges of polypharmacy and the impact of coronavirus disease 2019 (COVID-19) pandemic in older patients require further investigation. This retrospective study analyzed the progression of polypharmacy and anticholinergic burden in older patients in a primary care setting before, during, and after the COVID-19 pandemic.
Methods
This 3-year cross-sectional study (2019, 2020, and 2021) comprised a dynamic cohort of individuals aged ≥75 years, who attended the Arrabal Primary Care Center in Zaragoza, Spain. Older patients with polypharmacy (≥5 medications) were identified according to their electronic health records. We collected demographic and clinical data, including medication prescriptions, diagnoses, and anticholinergic risks, and performed descriptive and statistical analyses.
Results
This study included a total of 1,928 patients with a mean age of 83.52±0.30 years. Over the 3-year study period, the mean number of medications prescribed increased, from 9.4 in 2019 to 10.4 in 2021. The prevalence of excessive polypharmacy (≥10 medications) increased from 39% in 2019 to 45% in 2021. The most commonly prescribed drugs were anilides, proton pump inhibitors, benzodiazepine derivatives, and platelet aggregation inhibitors. Women had a higher prevalence of illnesses and anticholinergic drug prescriptions than men.
Conclusion
The results of this study highlighted an upward trend in polypharmacy and excessive polypharmacy among older patients in primary care settings. Future research should focus on optimizing medication management and deprescribing strategies and minimizing the adverse effects of polypharmacy in this population.
Population aging has significant implications for public health and healthcare systems.1) The proportion of the world's population aged ≥65 years is projected to increase from 10% in 2022 to 16% in 2050.2) An increasing population with progressive aging has led to an increase in the number of individuals with chronic diseases. In Europe, these conditions are among the leading causes of illness, disability, and healthcare costs.3)
Consequently, older individuals often receive multiple medications for comorbidities including geriatric syndromes such as dysphagia, delirium, depression, pressure ulcers, frailty, and dependence.4,5) This situation poses a major challenge as it often leads to polypharmacy in this population.
Polypharmacy and excessive polypharmacy are commonly defined as the concurrent use of ≥5 and ≥10 medications, respectively.6-9) Polypharmacy by itself is a geriatric syndrome, and its prevalence varies widely due to differences in study inclusion criteria (age group, definition, health care setting, location), and can range from 4% to >80%.10,11) For instance, in a cross-sectional study conducted across 17 European countries and Israel, researchers analyzed data from the sixth wave of the Survey of Health, Aging, and Retirement in Europe (SHARE) database. This study including participants aged ≥65 years (mean age 75.1±7.2 years), revealed that the prevalence of polypharmacy (simultaneous use of ≥5 medications), ranged from 26.3% to 39.9%.12) In addition, a cross-sectional study analyzing the electronic medical records of adults in Scotland reported a polypharmacy (4–9 medications) prevalence of 28.6% in adults aged 60–69 years and 51.8% in those >80 years.13) In this regard, a study based on data from the National Health Survey 2017 in Spain, which included participants aged ≥65 years (mean age 76±7.6 years), reported a polypharmacy and excessive polypharmacy prevalence of 27.3% and 0.9%, respectively.14)
The frequent occurrence of polypharmacy in the older adult population is concerning as it is associated with an increased risk of drug interactions, adverse drug effects, poor treatment adherence, and potentially inappropriate medication.15-18) These factors increase the susceptibility of older adults to cognitive and functional impairments, episodes of delirium, falls, hospital admissions, increased healthcare costs, and even mortality.19-22) Furthermore, certain drugs with anticholinergic activity may have adverse effects in this population, including confusion, dizziness, delirium, mild cognitive impairment, falls, compromised physical function, increased hospitalization rates, and elevated risk of mortality.23-25)
The increased vulnerability of older adults to complications and higher mortality rates, as evidenced during the coronavirus disease 2019 (COVID-19) pandemic, is attributable to factors including immunosenescence, frailty, underlying diseases, and the concurrent use of multiple medications.22,26) Additionally, the social isolation, fear of contagion, and loneliness experienced during the pandemic further exacerbated the susceptibility of older patients to adverse outcomes.27) In their meta-analysis, Pimentel-Tormon et al.28) reported the effects of the COVID-19 pandemic on the older adult population, including outcomes such as weight loss, increased prevalence of respiratory and heart diseases, and higher rates of depression and anxiety. In response to these new health problems, physicians may have prescribed additional medications to treat these pathologies.27) Consequently, studies have investigated the relationship between polypharmacy and COVID-19. Poblador-Plou et al.29) reported that a higher number of medications was associated with worse outcomes, including death, in men with COVID-19. Moreover, a meta-analysis of 14 studies involving 189,870 patients with COVID-19 reported the prevalence of polypharmacy as 34.6%.30)
Given its impact on the general population, especially older individuals, investigating the effects of the COVID-19 pandemic on polypharmacy and anticholinergic risks within this age group is essential. The pandemic has caused complications and adverse clinical, functional, psychosocial, and mental health outcomes. Unfortunately, current scientific literature offers limited insights into this topic. Therefore, the present study analyzed the evolution of polypharmacy and anticholinergic burden in older patients in a primary care setting before, during, and after the pandemic.
The study was designed in three cross-sectional periods—2019, 2020, and 2021—within a dynamic cohort composed of individuals aged ≥75 years who attended the Arrabal Primary Care Center in Zaragoza, Spain, between January 1, 2019, and December 31, 2021. We collected demographic and clinical variables from electronic primary care records from all patients using an Aragon health card at the time of their medical consultation and analyzed these variables of the older patients with polypharmacy (≥5 prescribed medications).
This study was reviewed and approved by the Aragon Clinical Research Ethics Committee (Protocol Code PI22/456; approval date on November 2nd, 2022). All procedures contributing to this work complied with the ethical standards of the Aragon Clinical Research Ethics Committee (part of the Government of Aragon’s Department of Health) and the principles of the 1975 Declaration of Helsinki, revised in 2008. Data were obtained from the clinical records provided in a non-identifiable format by the Aragonese Health Service. Written informed consent from the participants or their legal guardian/next of kin was not required for this study, in accordance with national legislation and institutional requirements (Law 14/2007, of July 3, on Spanish Biomedical Research). The processing, notification, and transfer of personal data was conducted in accordance with the European Parliament’s 2016/679 Regulation (EU) and the 3/2018 Spanish Organic Law on the Protection of Personal Data and the Guarantee of Digital Rights. This study complied the ethical guidelines for authorship and publishing in the Annals of Geriatric Medicine and Research.31)
The present study included all patients ≥75 years of age who were prescribed ≥5 medications based on the electronic health records of Arrabal Primary Care Center, a center of the Spanish public health system. Inclusion criteria are individuals aged ≥75 years with polypharmacy (≥5 prescribed medications).7-9)
The following variables were collected.
1) The total number of drugs prescribed at consultation was recorded to assess whether the patient had polypharmacy (≥5 medications) or excessive polypharmacy (≥10 medications).
2) The Anatomical Therapeutic Chemical Classification (ATC) system proposed by the World Health Organization was used to identify the drugs prescribed in the study. This system classifies drugs based on their therapeutic effects and characteristics. The system is organized into five levels and includes multiple categories at each level.
3) Diagnoses during consultation were made according to the International Classification of Primary Care 2 (CIAP-2),32) developed and updated by the World Organization of Family Doctors. The conditions are classified into 17 chapters based on the body systems that represent the problem's location and disease.
4) Comorbidity was measured using the CIAP-2.32)
5) We assessed anticholinergic risk using the anticholinergic cognitive burden (ACB) scale. This scale includes 88 medications with known anticholinergic activity. The assigned scores ranged from 0 to 3, with 0 indicating no activity and 3 indicating the maximum anticholinergic activity. We categorized ACB in the present study as 0, 1, 2, or 3+.
We analyzed the evolution in terms of diagnosis, anticholinergic risk, and drugs of low therapeutic usefulness in older patients who were prescribed >5 medications at the Arrabal Primary Care Center between 2019 and 2021.
We used descriptive analysis, with continuous variables expressed as means±standard deviation, and categorical (nominal) variables reported as percentages of the total sample. Owing to the large sample size, parametric tests were deemed appropriate because in large samples, even if the data distribution is not normal, the statistics tended to be normal.33) Welch two-sample t-tests were conducted to compare two numerical variables and assess significant differences in the means between the groups. We applied one-factor analysis of variance to examine substantial standard variations across groups for comparisons among more than two numerical variables after log-transformation to ensure that the data conformed sufficiently to normality. Heteroscedasticity in the data was not considered a problem because the designs were well-balanced. We used Fisher exact test to explore the associations between categorical variables. All statistical analyses were performed using R version 4.3 (https://cran.r-project.org/), with significance set at p<0.05. The R packages nortest and PMCMRplus were also used to analyze the data.
We included 1,928 patients aged ≥75 years who were prescribed >5 medications during the study period (2019–2021). The mean age of these individuals was 83.5±0.3 years, and 1,222 patients (63.4%) were females (Table 1). Evaluation of the distribution of patients according to age revealed that 37.3% of the patients were 75–79 years of age (Table 2).
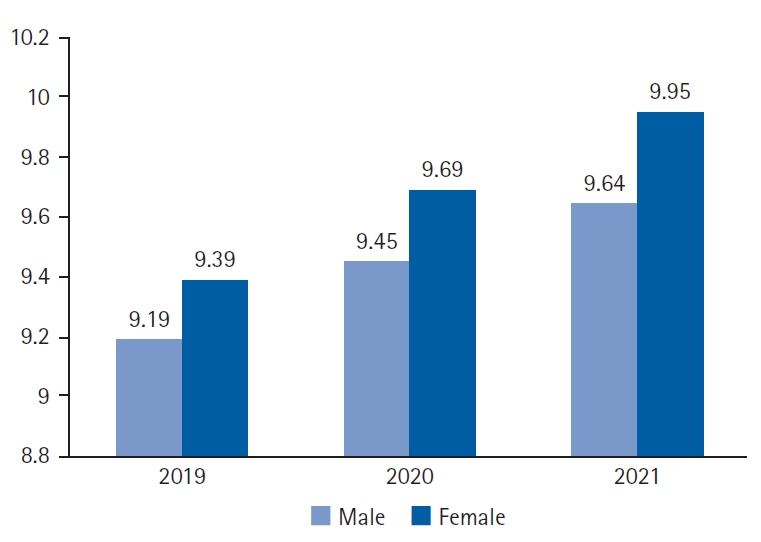
A mean of 9.3±0.15 medications were prescribed during the study period. The mean number of medicines per year among the enrolled patients showed a significant upward trend, with values of 9.4, 9.9, and 10.4 in 2019, 2020, and 2021, respectively (p=0.009). Regarding the number of drugs prescribed by sex per year, although we observed an increasing tendency to prescribe more drugs to women than men; however, the variation between sexes was not statistically significant (p=0.12). Specifically, we observed that the number of women taking multiple medications per year remained stable, with rates ranging from 761 to 870, while the figures for men were lower, at around 460 to 497 during the same period (2019–2021). In addition, the analysis of the average number of prescribed drugs according to sex revealed averages of 9.2 and 9.4 medications in men and women, respectively, in 2019, and 9.6 and 9.9 medications in 2021, respectively. The medication use did not differ significantly between the sexes for any of the 3 years (p=0.22, 0.23, and 0.10, respectively) (Fig. 1).
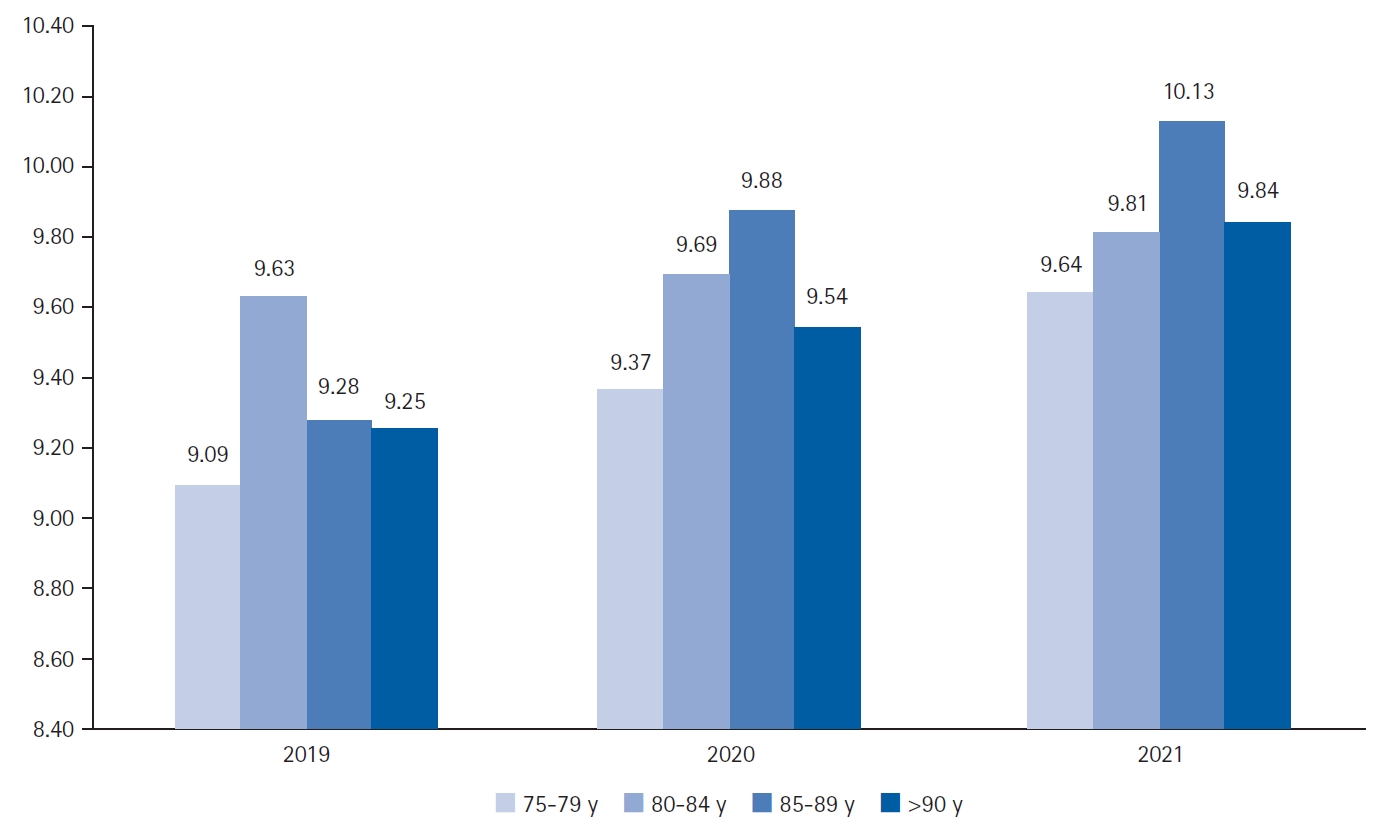
Moreover, examination of the mean number of drugs prescribed by the age range and year of the study showed that despite the observed upward trend, the number of drugs prescribed per patient according to age did not differ significantly (p=0.1, 0.2, and 0.3). Fig. 2 shows the annual trends observed in each year.
An average of 12.9, 14.2, 12.9, and 10.5 drugs were prescribed to patients aged 75–79, 80–84, 85–89, and >90 years, respectively. The result of the t-test showed statistically significant differences between groups (p<0.01) (Fig. 3). The sub-analysis comparing the mean numbers of drugs prescribed between patients >90 years and those aged 75–89 years showed no statistically significant difference.
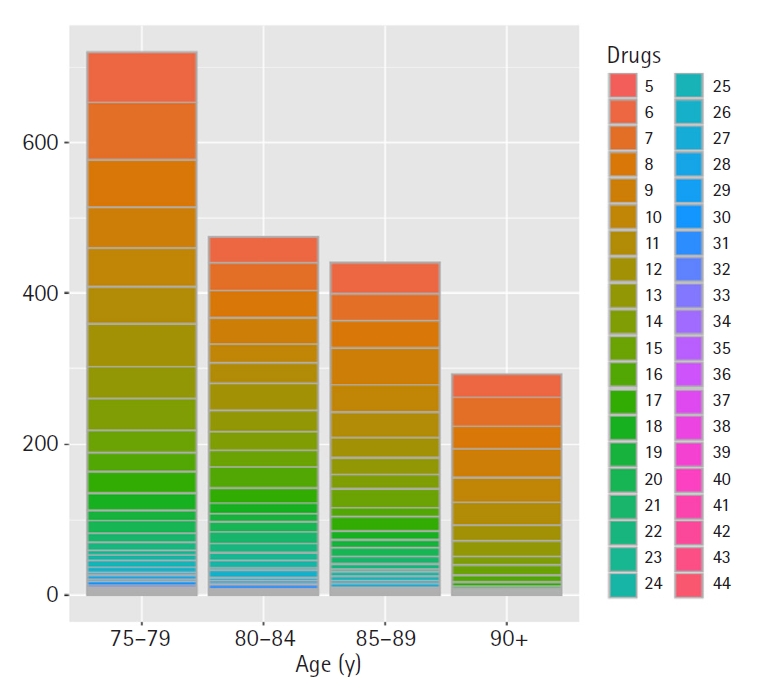
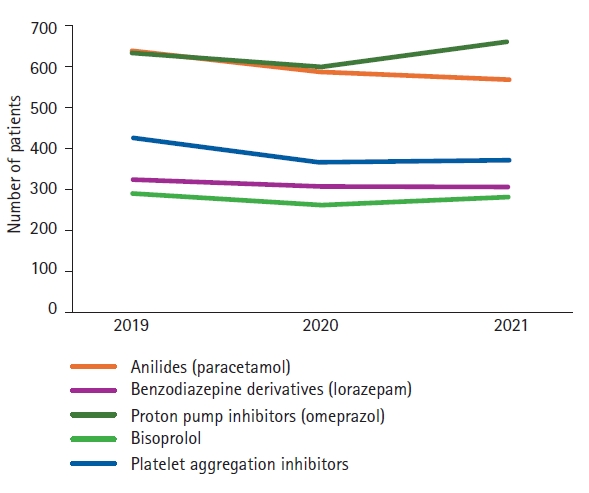
The results of the examination of the prevalence of excessive polypharmacy (≥10 medications) revealed an increase over the 3-year period, with 538 (39.4%), 506 (41.5%), and 551 (45.1%) patients in 2019, 2020, and 2021, respectively. Pearson product-moment correlation test identified a high correlation between the year and percentage of patients with excessive polypharmacy (R2=0.98); however, this relationship was not statistically significant (p=0.07). The most commonly prescribed drugs during the study period were anilides (paracetamol), proton pump inhibitors (PPIs), acetylic acid, lorazepam, and bisoprolol (Fig. 4).
The analysis of the prevalence of anticholinergic medication use revealed that 46% of the patients were on a drug with a low risk of anticholinergic activity, while 37.5% were prescribed a drug with high anticholinergic risk, a significant difference (p=0.006). Analysis of patients taking at least one anticholinergic drug across age groups showed that 73.7% of individuals aged 75–79 years were prescribed such medications; this percentage increased significantly to 89% among patients aged >90 years (p=0.0) (Fig. 5). Likewise, women were prescribed more anticholinergic drugs than men (p<0.01). The results of the comparative analysis of prescriptions of drugs with anticholinergic risk between patients under and over 90 years of age revealed that such drugs were prescribed to only 10.96% in patients <90 years and 89.5% among those aged >90 years; a statistically significant difference was observed (p<0.01).
As most patients were prescribed several drugs, which could be related to multimorbidity, we also analyzed the mean number of pathologies. The mean number of diseases was significantly lower in men (7.1) than in women (7.4). and showed a statistical difference (p=0.007). In contrast, while the mean number of diagnoses per patient ranged from 6.81 to 7.10 across age groups, the differences were not statistically significant (p=0.1). Additionally, the mean number of pathologies for 2019, 2020, and 2021 were 6.2, 6.4, and 6.5, respectively, and did not differ significantly (p=0.2). The most prevalent diseases in the patients included in the study were arterial hypertension (K86), non-insulin-dependent diabetes (T90), arterial hypertension (K86), lipid metabolism disorders (T93), and atrial fibrillation (K78).
The results of this study revealed a significant increase in the mean number of drugs prescribed over the 3-year study period, from 9.4 in 2019 to 10.4 in 2021. These results should be interpreted with caution as this increase cannot be attributed solely to the impact of the pandemic. Factors other than COVID-19 may have contributed to this increase, as new diseases may have occurred during this period. Moreover, the growing survival rate of the older population also increases the probability of developing multiple chronic diseases. The presence of two or more diseases affects approximately 40% of individuals aged ≥65 years, and this prevalence increases with age, increasing the likelihood of polypharmacy.12,34)
Considering the high vulnerability of the older population to polypathology and the impact of COVID-19, which has resulted in not only respiratory complications but also cardiac, hematological, and other health problems, a remarkable increase in the prescription of specific drugs designed to address these various medical conditions has been observed.35-37) Furthermore, the impact of the virus extends beyond the physical realm, with the older population experiencing elevated stress and anxiety levels due to the threat of the virus, pandemic uncertainties, and social isolation measures. Healthcare practitioners frequently prescribe antidepressants and anxiolytics to manage such psychological burdens.38,39)
We did not identify any research directly comparable to our findings, which underscores the need for further research to improve our understanding of medication patterns and their implications for older patients in primary care settings.
Regarding the characteristics of the included patients, 63.4% of the patients were women. This distribution is consistent with that of previous research that has related female sex to a higher prevalence of polypharmacy.12,14,40-42) This can be attributed to several factors. First, the demographic structure of the population plays an important role as women tend to have a longer life expectancy than men. Secondly, greater longevity exposes women to a higher likelihood of developing multiple chronic diseases, leading to polypharmacy.41) Concerning age, in the present study, 720 patients (37.3%) were 75–79 years of age, which is consistent with results reported by Gutiérrez-Valencia et al., in which polypharmacy was more frequent in individuals aged 76–85 years.14) Contrary to many studies suggesting that polypharmacy increases with age,13,40) we did not observe this trend in our study. One possible explanation could be that patients attending primary care centers present a relatively younger profile than those usually studied in polypharmacy research.
Our analysis of the number of polypharmacy patients across different age ranges revealed a decline throughout the 3-year study period. However, the number of patients attending health centers also decreased each year. This decline may be attributed to various factors, particularly the COVID-19 pandemic. In 2020 and 2021, many patients could not visit their healthcare facilities for regular care, as they may have followed safety guidelines and stayed home. Additionally, some individuals may have been relocated to alternative living arrangements such as staying with relatives or being admitted to nursing homes. Furthermore, some patients may have died during the study period. These factors may have contributed to the observed decrease in the number of patients receiving polypharmacy over time.
We also analyzed the number of drugs prescribed according to age groups; the average number of drugs dispensed during the study period according to age groups was >12.9 drugs in the 75–89 age group, which decreased to 10.5 in patients over >90 years of age. These results are consistent with those of a study conducted in octogenarians with polypharmacy, in which the number of medications gradually decreased with age.9) Furthermore, the mean number of drugs prescribed during the study period, 9.3±0.15, is concordant with the findings of a previous study conducted in primary care that identified the associations of comorbidities such as heart failure and ischemic heart disease with higher levels of medication prescription. Specifically, the authors identified a mean of nine medications for patients with heart failure and eight for those with ischemic heart disease.13) In contrast to our study, other investigations reported lower mean numbers of medications. Hazen et al. reported a mean of eight chronic medications.43) Additionally, another study on oncology patients reported 7.3±3.4 drugs (range 0–18).10) These findings highlight the variability in the number of medications prescribed among different patient populations.
In addition, our analysis of the prevalence of excessive polypharmacy among participants over the 3-year period revealed a gradual, although not statistically significant, increase in the number of patients experiencing this geriatric syndrome. Approximately 40%–45% of patients were affected by excessive polypharmacy. Compared with a study of 1,140 octogenarian patients that reported excessive polypharmacy in 16.9% and 20.7% of men and women, respectively, we observed a significantly higher prevalence in our cohort. These similarities with our study are significant because they reiterate the need for physicians to be aware of the potential complications arising from multiple drug interactions. These complications include adverse effects such as drug-drug interactions, increased risk of falls and fractures, cognitive impairment, and decreased functional capacity. Moreover, these findings emphasize the importance of carefully managing polypharmacy to minimize adverse effects and optimize patient outcomes.9,44,45)
Our sub-analysis of patients aged >90 years compared to the rest of the participants did not reveal a significant difference in the average number of prescribed drugs. In 2021, both groups were prescribed an average of 9.8 drugs. This finding suggests that we may be overlooking the issue of de-prescription in this age group and that measures should be taken to address this issue and ensure appropriate medication management for older adults.
Our study results revealed that the most commonly prescribed drugs were anilides, PPIs, benzodiazepine derivatives, and platelet aggregation inhibitors (excluding heparin). These results are consistent with those of a Spanish study in Barcelona that analyzed the electronic records of 916,619 people aged >65 years. In that study, 49.9% of the participants had polypharmacy, and the same five drugs were identified as the most frequently prescribed. Several studies have confirmed that PPIs and antithrombotic agents are the most commonly used drugs.4,43) These findings highlight the prevalence of this problem, with a significant number of prescriptions considered inappropriate owing to the unnecessary continuation of PPIs and a lack of appropriate indications. Our results underscore the need for healthcare professionals to exercise caution when prescribing PPIs to older adults, considering the potential risks and benefits, and ensuring that the indications are appropriate.46) Likewise, this caution is required not only for PPIs but also for every medication prescribed to older patients to avoid the inappropriate use of PPIs in older patients discharged from acute care hospitals.
Our analysis using the anticholinergic risk scale revealed a significant difference between sexes, with a higher prevalence of anticholinergic drug prescriptions among women, which is consistent with previous studies.47) Sex disparities in anticholinergic prescription patterns may be attributed to various factors, including differences in disease prevalence, healthcare-seeking behaviors, and pharmacokinetic and pharmacodynamic properties.41,42) Our results showed that 73.7% of patients aged 75–79 years were prescribed drugs with anticholinergic effects. We also observed a significant increase up to 89.4% in patients >90 years. These rates were higher than those reported in a study that was also conducted in the primary care setting, which reported that 25.8% of patients received at least one drug with anticholinergic action.48) Our results also revealed age-related changes in the use of anticholinergic medications, with a notably higher prevalence among individuals aged >90 years. This finding aligns with the fact that advanced age is often accompanied by multiple pathologies such as cognitive impairment, dementia, Parkinson disease, and incontinence.5) This contributes to an increased likelihood of patients taking at least one drug with anticholinergic properties as they age.49) Recent investigations have highlighted the adverse effects of anticholinergic drugs, including an increased incidence of dementia. This emphasizes the importance of close monitoring and controlling the use of anticholinergic medications to reduce short-, medium-, and long-term adverse effects.50)
In conclusion, we observed an increase in the mean number of drugs prescribed over a 3-year study period in patients aged >75 years. Although partly attributable to the COVID-19 pandemic, this growth underscores the complexity of polypharmacy in older adults, which requires vigilant monitoring and management. This study also revealed sex disparities, with a higher prevalence of polypharmacy in women, and a notable prevalence of anticholinergic medications, especially among those aged >90 years. Further research is required to better understand the underlying factors that contribute to polypharmacy and anticholinergic risk in geriatric patients. All healthcare professionals should prioritize the minimization of drug use and be cautious when prescribing new medications.
ACKNOWLEDGEMENTS
The authors would like to thank the Aragonese Primary Care Research Group (GAIAP, B21_23R) that is part of the Department of Innovation, Research and University at the Government of Aragón (Spain) and the Institute for Health Research Aragón (IIS Aragón); the Research Network on Chronicity, Primary Care and Health Promotion (RICAPPS, RD21/0016/0005) that is part of the Results-Oriented Cooperative Research Networks in Health (RICORS) (Carlos III Health Institute); and ERDF “Another way to make Europe,” NextGenerationEU funds and the University of Zaragoza.
ACKNOWLEDGMENTS
FUNDING
This work was supported by Aragonese Primary Care Research Group (GAIAP, B21_23R) that is part of the Department of Innovation, Research and University at the Government of Aragón (Spain) and the Institute for Health Research Aragon (IIS Aragon). The funders have no role in study design, data collection and analysis, decision to publish or manuscript preparation.
AUTHOR CONTRIBUTIONS
Conceptualization, RMB, BOB, AGR, PM; Data curation, PM, IFP, ATL, AGR, VCV; Formal analysis, BOB, RMB, ATL, VCV, PM; Writing-original draft, RMB, BOB, PM; writing-review & editing, PM, BOB, IFP, ATL, AGR, VCV, RMB. All authors have read and agreed to the published version of the manuscript.
Fig. 5.
Anticholinergic risks of the prescribed medications by age groups. ACB scale, anticholinergic cognitive burden scale.

Table 1.
Demographics and clinical characteristics of patients with polypharmacy (n=1,928)
REFERENCES
1. Cristea M, Noja GG, Stefea P, Sala AL. The impact of population aging and public health support on EU labor markets. Int J Environ Res Public Health 2020;17:1439.



2. United Nations, Department of Economic and Social Affairs. World population ageing 2020 highlights: living arrangements of older persons. New York, NY: United Nations; 2020.
3. Tran PB, Kazibwe J, Nikolaidis GF, Linnosmaa I, Rijken M, van Olmen J. Costs of multimorbidity: a systematic review and meta-analyses. BMC Med 2022;20:234.




4. Piccoliori G, Mahlknecht A, Sandri M, Valentini M, Vogele A, Schmid S, et al. Epidemiology and associated factors of polypharmacy in older patients in primary care: a northern Italian cross-sectional study. BMC Geriatr 2021;21:197.




5. Kojima T. The need for actions against polypharmacy in older people with frailty. Ann Geriatr Med Res 2018;22:111–6.



6. Lai X, Zhu H, Huo X, Li Z. Polypharmacy in the oldest old (≥80 years of age) patients in China: a cross-sectional study. BMC Geriatr 2018;18:64.




7. Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE. What is polypharmacy? A systematic review of definitions. BMC Geriatr 2017;17:230.




8. Pazan F, Wehling M. Polypharmacy in older adults: a narrative review of definitions, epidemiology and consequences. Eur Geriatr Med 2021;12:443–52.




9. Strehblow C, Smeikal M, Fasching P. Polypharmacy and excessive polypharmacy in octogenarians and older acutely hospitalized patients. Wien Klin Wochenschr 2014;126:195–200.



10. Prithviraj GK, Koroukian S, Margevicius S, Berger NA, Bagai R, Owusu C. Patient characteristics associated with polypharmacy and inappropriate prescribing of medications among older adults with cancer. J Geriatr Oncol 2012;3:228–37.



11. Bonaga B, Sanchez-Jurado PM, Martinez-Reig M, Ariza G, Rodriguez-Manas L, Gnjidic D, et al. Frailty, polypharmacy, and health outcomes in older adults: the frailty and dependence in albacete study. J Am Med Dir Assoc 2018;19:46–52.


12. Midao L, Giardini A, Menditto E, Kardas P, Costa E. Polypharmacy prevalence among older adults based on the survey of health, ageing and retirement in Europe. Arch Gerontol Geriatr 2018;78:213–20.


13. Payne RA, Avery AJ, Duerden M, Saunders CL, Simpson CR, Abel GA. Prevalence of polypharmacy in a Scottish primary care population. Eur J Clin Pharmacol 2014;70:575–81.



14. Gutierrez-Valencia M, Aldaz Herce P, Lacalle-Fabo E, Contreras Escamez B, Cedeno-Veloz B, Martinez-Velilla N. Prevalence of polypharmacy and associated factors in older adults in Spain: data from the National Health Survey 2017. Med Clin (Barc) 2019;153:141–50.


15. Aubert CE, Streit S, Da Costa BR, Collet TH, Cornuz J, Gaspoz JM, et al. Polypharmacy and specific comorbidities in university primary care settings. Eur J Intern Med 2016;35:35–42.


16. Yang PJ, Lee YT, Tzeng SL, Lee HC, Tsai CF, Chen CC, et al. Potentially inappropriate prescribing in disabled older patients with chronic diseases: a screening tool of older persons' potentially inappropriate prescriptions versus beers 2012 criteria. Med Princ Pract 2015;24:565–70.




17. Perez-Jover V, Mira JJ, Carratala-Munuera C, Gil-Guillen VF, Basora J, Lopez-Pineda A, et al. Inappropriate use of medication by elderly, polymedicated, or multipathological patients with chronic diseases. Int J Environ Res Public Health 2018;15:310.



18. Chang CB, Chen JH, Wen CJ, Kuo HK, Lu IS, Chiu LS, et al. Potentially inappropriate medications in geriatric outpatients with polypharmacy: application of six sets of published explicit criteria. Br J Clin Pharmacol 2011;72:482–9.



19. Tiihonen J, Suokas JT, Suvisaari JM, Haukka J, Korhonen P. Polypharmacy with antipsychotics, antidepressants, or benzodiazepines and mortality in schizophrenia. Arch Gen Psychiatry 2012;69:476–83.


20. Ahmed B, Nanji K, Mujeeb R, Patel MJ. Effects of polypharmacy on adverse drug reactions among geriatric outpatients at a tertiary care hospital in Karachi: a prospective cohort study. PLoS One 2014;9:e112133.



21. Filkova M, Carvalho J, Norton S, Scott D, Mant T, Molokhia M, et al. Polypharmacy and unplanned hospitalizations in patients with rheumatoid arthritis. J Rheumatol 2017;44:1786–93.


22. Gutierrez-Valencia M, Izquierdo M, Cesari M, Casas-Herrero A, Inzitari M, Martinez-Velilla N. The relationship between frailty and polypharmacy in older people: a systematic review. Br J Clin Pharmacol 2018;84:1432–44.




23. Cao YJ, Mager DE, Simonsick EM, Hilmer SN, Ling SM, Windham BG, et al. Physical and cognitive performance and burden of anticholinergics, sedatives, and ACE inhibitors in older women. Clin Pharmacol Ther 2008;83:422–9.


24. Reinold J, Schafer W, Christianson L, Barone-Adesi F, Riedel O, Pisa FE. Anticholinergic burden and fractures: a systematic review with methodological appraisal. Drugs Aging 2020;37:885–97.




25. Carnahan RM, Lund BC, Perry PJ, Pollock BG, Culp KR. The Anticholinergic Drug Scale as a measure of drug-related anticholinergic burden: associations with serum anticholinergic activity. J Clin Pharmacol 2006;46:1481–6.


26. Blomaard LC, van der Linden CM, van der Bol JM, Jansen SW, Polinder-Bos HA, Willems HC, et al. Frailty is associated with in-hospital mortality in older hospitalised COVID-19 patients in the Netherlands: the COVID-OLD study. Age Ageing 2021;50:631–40.




27. Modesti PA, Wang J, Damasceno A, Agyemang C, Van Bortel L, Persu A, et al. Indirect implications of COVID-19 prevention strategies on non-communicable diseases: an Opinion Paper of the European Society of Hypertension Working Group on Hypertension and Cardiovascular Risk Assessment in Subjects Living in or Emigrating from Low Resource Settings. BMC Med 2020;18:256.



28. Pimentel-Tormon F, Dino MJ, Francis J, Espiritu E, Garcia RR, Patomchai JU, et al. The negative impact of COVID-19 on elderly: a systematic review. New Trends Qual Res 2022;11:e543.

29. Poblador-Plou B, Carmona-Pirez J, Ioakeim-Skoufa I, Poncel-Falco A, Bliek-Bueno K, Cano-Del Pozo M, et al. Baseline chronic comorbidity and mortality in laboratory-confirmed COVID-19 cases: results from the PRECOVID study in Spain. Int J Environ Res Public Health 2020;17:5171.



30. Ghasemi H, Darvishi N, Salari N, Hosseinian-Far A, Akbari H, Mohammadi M. Global prevalence of polypharmacy among the COVID-19 patients: a comprehensive systematic review and meta-analysis of observational studies. Trop Med Health 2022;50:60.




31. Noh JH, Jung HW, Ga H, Lim JY. Ethical guidelines for publishing in the Annals of Geriatric Medicine and Research. Ann Geriatr Med Res 2022;26:1–3.




32. World Organization of Family Doctors (WONCA). [CIAP-2 International Classification of Primary Care]. Barcelona, Spain: Masson; 1999.
33. Lubin Pigouche P, Macia Anton MA, Rubio de Lemus P. [Mathematical psychology II]. Madrid, Spain: Universidad Nacional de Educacion a Distancia; 2005.
34. Silva IR, Goncalves LG, Chor D, Fonseca MJ, Mengue SS, Acurcio FA, et al. Polypharmacy, socioeconomic indicators and number of diseases: results from ELSA-Brasil. Rev Bras Epidemiol 2020;23:e200077.


35. Flaherty GT, Hession P, Liew CH, Lim BCW, Leong TK, Lim V, et al. COVID-19 in adult patients with pre-existing chronic cardiac, respiratory and metabolic disease: a critical literature review with clinical recommendations. Trop Dis Travel Med Vaccines 2020;6:16.




36. Nikoloski Z, Alqunaibet AM, Alfawaz RA, Almudarra SS, Herbst CH, El-Saharty S, et al. Covid-19 and non-communicable diseases: evidence from a systematic literature review. BMC Public Health 2021;21:1068.




37. Kang Y, Chen T, Mui D, Ferrari V, Jagasia D, Scherrer-Crosbie M, et al. Cardiovascular manifestations and treatment considerations in COVID-19. Heart 2020;106:1132–41.



38. Maresova P, Javanmardi E, Barakovic S, Barakovic Husic J, Tomsone S, Krejcar O, et al. Consequences of chronic diseases and other limitations associated with old age: a scoping review. BMC Public Health 2019;19:1431.




39. Siso-Almirall A, Kostov B, Sanchez E, Benavent-Areu J, Gonzalez de Paz L. Impact of the COVID-19 pandemic on primary health care disease incidence rates: 2017 to 2020. Ann Fam Med 2022;20:63–8.



40. Haider SI, Johnell K, Weitoft GR, Thorslund M, Fastbom J. The influence of educational level on polypharmacy and inappropriate drug use: a register-based study of more than 600,000 older people. J Am Geriatr Soc 2009;57:62–9.


41. Venturini CD, Engroff P, Ely LS, Zago LF, Schroeter G, Gomes I, et al. Gender differences, polypharmacy, and potential pharmacological interactions in the elderly. Clinics (Sao Paulo) 2011;66:1867–72.


42. Thurmann PA, Hompesch BC. Influence of gender on the pharmacokinetics and pharmacodynamics of drugs. Int J Clin Pharmacol Ther 1998;36:586–90.

43. Hazen AC, Zwart DL, Poldervaart JM, de Gier JJ, de Wit NJ, de Bont AA, et al. Non-dispensing pharmacists' actions and solutions of drug therapy problems among elderly polypharmacy patients in primary care. Fam Pract 2019;36:544–51.



44. Wastesson JW, Morin L, Tan EC, Johnell K. An update on the clinical consequences of polypharmacy in older adults: a narrative review. Expert Opin Drug Saf 2018;17:1185–96.


45. Walckiers D, Van der Heyden J, Tafforeau J. Factors associated with excessive polypharmacy in older people. Arch Public Health 2015;73:50.



46. Schepisi R, Fusco S, Sganga F, Falcone B, Vetrano DL, Abbatecola A, et al. Inappropriate use of proton pump inhibitors in elderly patients discharged from acute care hospitals. J Nutr Health Aging 2016;20:665–70.



47. Raei K, Rahimi A, Hosseini SR, Moghadamnia AA, Bijani A. Anticholinergic drug use in elderly people: a population- based study in Iran. Caspian J Intern Med 2021;12:593–9.


48. Grande G, Tramacere I, Vetrano DL, Clerici F, Pomati S, Mariani C, et al. Role of anticholinergic burden in primary care patients with first cognitive complaints. Eur J Neurol 2017;24:950–5.