|
 |
- Search
| Ann Geriatr Med Res > Volume 27(4); 2023 > Article |
|
Abstract
Background
Coronavirus disease 2019 (COVID-19) can cause multiple acute complications. This study evaluated the long-term functional status of older patients hospitalized for acute COVID-19.
Methods
We analyzed data from a multicenter ambispective cohort study on patients aged >60 years who were hospitalized for COVID-19 at two tertiary care hospitals in Argentina. The participants were contacted by telephone between November 2021 and September 2022 to collect data on their functional status. Ordinal logistic regression was used to identify factors associated with functional limitations after discharge.
Results
Among the 374 included patients, 205 (55%) showed functional limitations, including 58 (28%) who died during follow-up. The factors independently associated with functional limitations were low baseline functional status (odds ratio [OR]=9.19; 95% confidence interval [CI], 3.35–25.17) and admission to the intensive care unit (OR=4.41; 95% CI, 2.28–8.53). Men had lower odds of functional impairment (OR=0.55; 95% CI, 0.35–0.86).
Conclusion
Older patients had high mortality rates and poor functional status at 2 years post-discharge for COVID-19. Several factors at the time of discharge were associated with a higher risk of functional limitations and can be used to identify patients’ long-term needs for support and rehabilitation services.
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was first reported in December 2019 in Wuhan, China.1) It subsequently spread rapidly worldwide and was declared a pandemic by the World Health Organization in 2020. COVID-19 has high infection rates, significant morbidity, and mortality rates.2) Although the prevalence and mechanisms are not yet fully understood, several studies have reported persistent symptoms following acute COVID-19. This entity involves multiple systems and has been labeled as “long COVID-19 syndrome” or “post-COVID-19 syndrome.” The possible contributing factors include residual organ damage, persistent systemic inflammation, effects of hospitalization, and associated comorbidities.3) Because of the number of individuals affected and the substantial impact on well-being, the short- and long-term sequelae of COVID-19 have emerged as major public health concerns.4,5)
The impact of COVID-19 on physical and mental health has been documented.6,7) Studies have described functional status limitations after COVID-19 among patients with mild-to-severe acute disease, with more frequent and severe functional limitations after hospitalization. Huang et al.8-10) showed that up to 47% of patients requiring intensive care unit (ICU) admission experienced functional limitations 6 months after discharge, compared to 25% to 30% of other hospitalized patients. However, little is known about the rates of functional impairment in older patients hospitalized for COVID-19, a group at a higher risk of poor outcomes. Data from this vulnerable patient group are critical for planning appropriate rehabilitation care after discharge.
This study described the frequency and risk factors for functional limitations in older adults hospitalized for acute COVID-19 at two large tertiary care medical centers in Argentina.
We used data from a multicenter, ambispective cohort study conducted at Dr. César Milstein Hospital, a university hospital located in Buenos Aires City, Argentina, managed by the National Institute of Social Services for Retirees and Pensioners (INSSJP/PAMI), and the Regional Hospital Dr. Víctor Sanguinetti, a public hospital in the city of Chubut, Argentina, and associated with the National University of Patagonia San Juan Bosco. This study was approved by the Institutional Review Boards of IRB Hospital Dr. César Milstein (No. 5265) and Hospital Dr. Víctor Sanguinetti (No. 03/2023). Also, this study complied the ethical guidelines for authorship and publishing in the Annals of Geriatric Medicine and Research.11) Eligible participants were adults >60 years of age who survived hospitalization for acute COVID-19 at one of the participating hospitals between April 2020 and March 2022. SARS-CoV-2-19 infection was determined based on a positive polymerase chain reaction (PCR) or rapid antigen test. We excluded patients who could not be contacted by phone for follow-up and those who did not agree to participate in the study.
The participants were contacted by phone between November 2021 and September 2022 by trained study personnel, who conducted interviews to collect data on the study variables using a standardized questionnaire. Additional information was obtained from an institutional registry containing the sociodemographic and clinical characteristics of all patients admitted for COVID-19 to Víctor Sanguinetti Hospital. We also reviewed the medical records of patients admitted to both hospitals to complement the survey data. Finally, we reviewed the INSSJP/PAMI registry to identify patients who died after discharge and extracted data on the date of death.
The sociodemographic data included age, sex, and years of education (elementary/middle school, high school, college, or doctoral degree). We obtained information from medical records regarding comorbidities at admission, including a history of cardiovascular disease, cerebrovascular disease, chronic obstructive pulmonary disease (COPD), asthma, diabetes (DM), and cancer.
We used the Katz Index to characterize the patients’ ability to independently conduct activities of daily living before admission, which was collected by self-report at the time of the follow-up call. The instrument evaluates six basic functions of daily living (bathing, dressing, feeding, toilet use, continence, and mobility) and summarizes the patient’s status into eight categories, from total independence (A) to high dependence (H; loss of all functions). Hospitalization-related variables included ICU admission and length of hospital stay. The disposition locations (home vs. nursing home) at discharge were collected from medical records.
The primary outcome was functional status post-discharge, which was assessed at the time of the follow-up call using the Latin-American version of the Manual for the Post-COVID-19 Functional Status Scale.12) This validated scale classifies functional status into the following categories: no functional limitation (ability to live alone and perform daily activities without help and without experiencing symptoms); minimal functional limitation (ability to perform daily activities but with symptoms); mild functional limitation (need to reduce or avoid certain daily activities because of symptoms); moderate limitation (ability to perform certain daily activities but loss of ability to perform others); severe functional limitation (inability to live independently and perform daily activities); and death. For the analysis, we grouped the minimal, mild, moderate, and severe categories to create a four-level variable indicating no limitation, mild limitation, moderate limitation, or death.
The baseline characteristics of the study participants according to the four categories of functional status limitation were compared using analysis of variance (ANOVA), Kruskal–Wallis test, or chi-square test, as appropriate. The distribution of functional status impairments in the first year and >1-year post-discharge was calculated using descriptive statistics.
We used ordinal logistic regression to assess the independent associations of age, sex, education, history of cardiovascular disease, COPD, asthma, DM, baseline Katz index, ICU admission, length of stay, and discharge disposition with functional status. Regarding the age variable, we used a range between 60 and 70 years old as a reference value. For the multivariate analysis, we collapsed the Katz Index into Katz A as the reference value (no impairment in performing daily living activities), Katz B (mild impairment), and Katz C or worse (major impairment). The model was also adjusted for the time from discharge to the follow-up call to control for potential changes in functional status over time.
Power calculations showed that with a sample of approximately 370 patients, the study had >80% power to identify predictors, with a prevalence of 30% and a 15% absolute difference in functional status.
The statistical analyses were conducted using Stata version 13 (Stata Corporation, College Station, TX, USA) with two-tailed p-values and a significance level of 0.05.
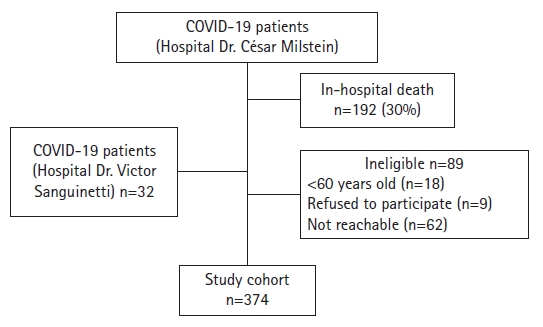
From November 2021 to September 2022, 623 patients were admitted for COVID-19 at Dr. César Milstein Hospital and were eligible for inclusion. Of these, 192 (30%) were excluded due to in-hospital death, and 89 (14%) were excluded due to age <60 years (3%), inability to be contacted (10%), or refusal to participate (1%), leaving a cohort of 342 patients. We also included 32 patients admitted to Dr. Víctor Sanguinetti Hospital, resulting in a final cohort of 374 patients (Fig. 1). The median time from discharge to follow-up was 425 days (interquartile range [IQR], 322–495 days). Interviews were conducted during the first year and between 12 and 24 months post-discharge in 133 (35%) and 240 (64%) participants, respectively.
Baseline characteristics and hospitalization-related variables according to functional status are shown in Table 1. Patients with worse functional status or those who died after discharge were older (p<0.001), more likely to be female (p=0.009), and less likely to have completed elementary/middle school (p=0.02). The two most prevalent comorbidities among the study participants were hypertension (68.1%) and DM (71.4%). Heart failure, chronic kidney disease, dementia, and cancer were more common in patients who died after discharge (p=0.04, p=0.02, p<0.001, and p=0.005, respectively). The levels of functional status at baseline differed significantly across the groups, with more severe impairment associated with worse post-discharge outcomes (p<0.001). The median overall length of stay was 12 days (IQR, 8–21 days), with longer stays in older patients with worse functional status post-discharge (p<0.001). ICU admission during hospitalization (p=0.003) and discharge to a rehabilitation or nursing home facility (p<0.001) were associated with poor functional outcomes post-discharge (Table 2).
Among 136 patients (36%) with 1-year follow-up data, 29.4%, 13.2%, and 22.7% reported no, mild, and moderate/severe limitations, respectively, while 35.3% of the patients had died. Among the 237 patients followed up at 2 years post-discharge, 53.5%, 16.4%, and 25.7%, reported no, mild, and moderate/severe limitations, respectively, while 4.2% had died (Fig. 2).
The factors significantly associated with functional limitations post-discharge in adjusted analyses were older age (odds ratio [OR]=1.86; 95% confidence interval [CI], 1.14–3.03), worse baseline functional status—Katz B (OR=9.19; 95% CI, 3.35–25.17), Katz C or worse (OR=13.30; 95% CI, 6.02–29.36)—and ICU admission (OR=4.41; 95% CI, 2.28–8.53). Conversely, male sex was associated with lower odds of functional limitations (OR=0.55; 95% CI, 0.35–0.86). Additionally, the model showed a significant association between the time since discharge and functional status, e.g., for every 6-month period after discharge, the odds of an increase in the functional limitation scale decreased by 0.50 (95% CI, 0.37–0.66).
COVID-19 is associated with multiple long-term conditions that can substantially and negatively affect patient health and quality of life. In this study, we observed high levels of functional limitations up to 2 years post-discharge from hospitalization among older adults with COVID-19. Additionally, we identified several predictors of poor functional status and mortality that could help identify patients who may require home support and/or rehabilitation services after discharge. This information can guide discharge planning and inform the development of interventions to support the health and maintain the independence of older adults requiring hospitalization for acute COVID-19.
Previous studies described the functional outcomes of patients admitted to hospital for COVID-19. A cohort study of 318 older patients who survived hospitalization for COVID-19 showed a 36% prevalence of functional limitations 3 months after discharge.13) Consistent with our findings, Battistela et al.14) found that 71% of COVID-19 survivors reported limitations in their daily activities 11 months post-discharge from the hospital. In addition, a Chinese ambispective cohort study including data from 2,469 survivors of COVID-19 hospitalization, also showed worse functional status rates compared to healthy controls 2 years after discharge.15)
In this study, we observed that male sex was associated with a lower likelihood of functional limitations. Likewise, worse baseline functionality, older age, and ICU admission were associated with poorer functional status. These findings are consistent with those of previous studies.16-19)
Moreover, our analyses showed that admission was associated with increased functional limitations and/or mortality after discharge. Previous studies described functional impairments following ICU admission owing to COVID-19 and other critical illnesses. Cavalleri et al.20) assessed functional status 1 year after hospital discharge and found that approximately 35% of critically ill patients experienced functional limitations without significant differences between those admitted as a consequence of COVID-19 and other conditions.
High rates of functional limitation after hospitalization have also been reported in patients not requiring critical care. A pre-pandemic prospective cohort of 230 older adults discharged from Milstein Hospital reported a 68% rate of short-term functional limitations.21) Long-term functional limitations after a non-COVID-19 acute illness requiring hospitalization were also reported in 27% of 369 patients in a Spanish cohort.22) These findings suggest that the high rates of long-term functional disability observed in our cohort may not solely be due to COVID-19, and may also represent the impact of acute disease, hospital-related complications, baseline limitations in functional status, comorbidities, and the well-described “post-ICU syndrome.”23,24)
We observed a 1-year post-discharge mortality rate of 12.8% and a cumulative mortality at 2 years of 16%. Other studies on older patients with acute COVID-19 showed heterogeneous long-term survival outcomes, ranging from <4% to 13%.25-28) High mortality rates (up to 20% or 33%) because of non-cardiovascular acute illnesses were observed in older adults discharged from hospitals.21,22) Similarly, cohorts of survivors of critical illness associated with respiratory failure in the pre-COVID-19 era reported mortality rates of 17% and 38% at 6 months and 2 years, respectively.29) These differences may be related to the baseline characteristics and pre-admission functional statuses of the populations reported in these studies.
This study had several strengths and limitations that should be considered when interpreting the results. The strengths of this study include the use of a well-validated scale to measure functional status, which was specifically designed to assess patients post-COVID-19. Additionally, we followed the participants for up to 2 years post-discharge to assess the long-term outcomes. The limitations of this study included the limited study sites. While we included patients from two large medical centers, most participants were admitted to Dr. César Milstein Hospital, which potentially limits the generalizability of our results. However, Dr. César Milstein is a major medical center in Buenos Aires that serves a large population of publicly insured inner-city older adults. Additionally, we collected self-reported data (e.g., pre-admission functional status) several months post-discharge, which may have been influenced by recall bias. However, several variables were obtained from medical records or institutional registries at the time of admission. Finally, we did not include a control group of patients without COVID-19. Thus, we could not explore whether the observed limitations in functional status were specifically related to COVID-19 or were generally associated with the need for hospitalization or ICU stay.
In conclusion, the results of our study showed relatively high rates of early severe functional limitations and mortality among older adults post-discharge for COVID-19. Our findings can help identify patients at high risk of poor functional outcomes following discharge and plan home support interventions to assist the needs of these patients. Early recognition and rehabilitation programs may be required to effectively prevent or manage the long-term complications of severe COVID-19 in older adults.
ACKNOWLEDGEMENTS
We thank the American Thoracic Society’s MECOR Program and faculty for their input in the design and analysis of this study.
ACKNOWLEDGMENTS
Fig. 2.
Functional status distribution among older patients discharge following COVID-19 hospitalization. Most deaths occurred during the first year post-discharge. More than 50% of patients had no functional limitations >1-year post-discharge.
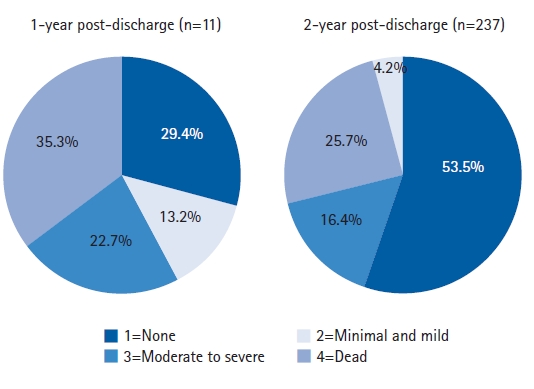
Table 1.
Sociodemographic and clinical baseline characteristics of study population
Table 2.
Adjusted associations between baseline characteristics and functional status after discharge
REFERENCES
1. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020;382:727–33.



2. Pan American Health Organization. COVID-19 situation report [Internet]. Washington, DC: Pan American Health Organization; c2023 [cited 2023 Sep 15]. Available from: https://www.paho.org/es/informes-situacion-covid-19.
3. Oronsky B, Larson C, Hammond TC, Oronsky A, Kesari S, Lybeck M, et al. A Review of Persistent Post-COVID Syndrome (PPCS). Clin Rev Allergy Immunol 2023;64:66–74.




4. Aiyegbusi OL, Hughes SE, Turner G, Rivera SC, McMullan C, Chandan JS, et al. Symptoms, complications and management of long COVID: a review. J R Soc Med 2021;114:428–42.




5. Pavli A, Theodoridou M, Maltezou HC. Post-COVID syndrome: incidence, clinical spectrum, and challenges for primary healthcare professionals. Arch Med Res 2021;52:575–81.



6. Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, et al. Post-acute COVID-19 syndrome. Nat Med 2021;27:601–15.




7. Nasserie T, Hittle M, Goodman SN. Assessment of the frequency and variety of persistent symptoms among patients with COVID-19: a systematic review. JAMA Netw Open 2021;4:e2111417.



8. Taboada M, Moreno E, Carinena A, Rey T, Pita-Romero R, Leal S, et al. Quality of life, functional status, and persistent symptoms after intensive care of COVID-19 patients. Br J Anaesth 2021;126:e110–3.



9. Baker HA, Safavynia SA, Evered LA. The ‘third wave’: impending cognitive and functional decline in COVID-19 survivors. Br J Anaesth 2021;126:44–7.



10. Daunter AK, Bowman A, Danko J, Claflin ES, Kratz AL. Functional decline in hospitalized patients with COVID-19 in the early months of the pandemic. PM R 2022;14:198–201.



11. Noh JH, Jung HW, Ga H, Lim JY. Ethical guidelines for publishing in the Annals of Geriatric Medicine and Research. Ann Geriatr Med Res 2022;26:1–3.




12. Klok FA, Boon GJ, Barco S, Endres M, Geelhoed JJ, Knauss S, et al. The Post-COVID-19 Functional Status scale: a tool to measure functional status over time after COVID-19. Eur Respir J 2020;56:2001494.



13. Prampart S, Le Gentil S, Bureau ML, Macchi C, Leroux C, Chapelet G, et al. Functional decline, long term symptoms and course of frailty at 3-months follow-up in COVID-19 older survivors: a prospective observational cohort study. BMC Geriatr 2022;22:542.




14. Battistella LR, Imamura M, De Pretto LR, Van Cauwenbergh SK, Delgado Ramos V, Saemy Tome Uchiyama S, et al. Long-term functioning status of COVID-19 survivors: a prospective observational evaluation of a cohort of patients surviving hospitalisation. BMJ Open 2022;12:e057246.



15. Huang L, Li X, Gu X, Zhang H, Ren L, Guo L, et al. Health outcomes in people 2 years after surviving hospitalisation with COVID-19: a longitudinal cohort study. Lancet Respir Med 2022;10:863–76.



16. Laskovski L, Felcar JM, Fillis MM, Trelha CS. Risk factors associated with limited functional status among out-of-hospital patients 30 days and one year after a diagnosis of COVID-19: a cohort study. Sci Rep 2023;13:3584.




17. Paradowska-Nowakowska E, Loboda D, Golba KS, Sarecka-Hujar B. Long COVID-19 syndrome severity according to sex, time from the onset of the disease, and exercise capacity-the results of a cross-sectional study. Life (Basel) 2023;13:508.



18. Pela G, Goldoni M, Solinas E, Cavalli C, Tagliaferri S, Ranzieri S, et al. Sex-related differences in long-COVID-19 syndrome. J Womens Health (Larchmt) 2022;31:620–30.


19. Combret Y, Kerne G, Pholoppe F, Tonneville B, Plate L, Marques MH, et al. Remote Assessment of Quality of Life and Functional Exercise Capacity in a Cohort of COVID-19 Patients One Year after Hospitalization (TELECOVID). J Clin Med 2022;11:905.



20. Cavalleri J, Treguier D, Deliege T, Gurdebeke C, Ernst M, Lambermont B, et al. One-year functional decline in COVID-19 and non-COVID-19 critically ill survivors: a prospective study incorporating a pre-ICU status assessment. Healthcare (Basel) 2022;10:2023.



21. Saenz V, Zuljevic N, Elizondo C, Martin Lesende I, Caruso D. Baseline functional status and one-year mortality after hospital admission in elderly patients: a prospective cohort study. Rev Fac Cien Med Univ Nac Cordoba 2020;77:143–8.



22. Baztan JJ, Galvez CP, Socorro A. Recovery of functional impairment after acute illness and mortality: one-year follow-up study. Gerontology 2009;55:269–74.



23. Rawal G, Yadav S, Kumar R. Post-intensive care syndrome: an overview. J Transl Int Med 2017;5:90–2.



24. Yuan C, Timmins F, Thompson DR. Post-intensive care syndrome: a concept analysis. Int J Nurs Stud 2021;114:103814.


25. Maestre-Muniz MM, Arias A, Mata-Vazquez E, Martin-Toledano M, Lopez-Larramona G, Ruiz-Chicote AM, et al. Long-term outcomes of patients with coronavirus disease 2019 at one year after hospital discharge. J Clin Med 2021;10:2945.



26. Mutch CP, Ross DA, Bularga A, Nicola Rose Cave R, Chase-Topping ME, Anand A, et al. Performance status: a key factor in predicting mortality in the first wave of COVID-19 in South-East Scotland. J R Coll Physicians Edinb 2022;52:204–12.




27. Shoucri SM, Purpura L, DeLaurentis C, Adan MA, Theodore DA, Irace AL, et al. Characterising the long-term clinical outcomes of 1190 hospitalised patients with COVID-19 in New York City: a retrospective case series. BMJ Open 2021;11:e049488.



- TOOLS