|
 |
- Search
| Ann Geriatr Med Res > Volume 27(2); 2023 > Article |
|
Abstract
Background
Reducing the risk of falling by improving balance and leg strength may be a preventive strategy. This study evaluated the integrated effects of Thai essential oil and balance exercises on parameters associated with Falls in community-dwelling older adults at risk of falling.
Methods
Fifty-six participants were randomly allocated to either the intervention group (IG), which performed balance exercises while smelling Thai essential oil scents of Zanthoxylum limonella (Dennst.) Alston, or the control group (CG), which performed balance exercises while receiving a control patch. Balance exercises were practiced for 12, 30-minute sessions over 4 weeks. Static and dynamic balance with eyes open and eyes closed (EC), leg muscle strength, agility, and fear of falling were assessed at baseline, after the 4-week intervention, and at 1 month after the last intervention session.
Results
Both groups showed significant improvements in static and dynamic balance, ankle plantarflexor strength, and agility after the 4-week intervention (p<0.05), which persisted at the 1-month follow-up (p<0.05). Compared to the CG, the IG demonstrated significantly better static balance in terms of elliptical sway area (p=0.04) and center of pressure (CoP) velocity (p=0.001) during EC, as well as ankle plantarflexor strength (p=0.01). The IG also maintained a significantly greater improvement in CoP velocity during EC (p=0.01).
Although advances in medicine and public health have increased life expectancy, the sanitary and social costs associated with dependency and mortality have risen significantly.1) Falls are a major public health issue in community-dwelling older adults, resulting in a lower quality of life and dependency.2,3) In particular, impaired balance and sensory perception, leg muscle weakness, and decreased agility have been proposed as major risk factors for falls and increased fear of falling.3-5) Previous research identified moderate correlations between poor balance, low physical activity, and decreased agility in older adults.6) Therefore, potential and simple-to-implement interventions focusing on improving balance and physical fitness in older adults at risk of falling may be advantageous.7)
Postural control is a complex motor task that involves maintaining, achieving, or restoring balance during any posture or activity.8) Maintaining postural control requires three major systems: the visual, vestibular, and somatosensory systems. However, the functions of these systems deteriorate with age.8) Balance exercises have been used to improve balance ability and reduce the rate of falling in older adults.9) Martial art-based balance exercises, such as Thai boxing exercise (TBE), could make exercise more appealing to older adults.7,10) Areeudomwong et al.7) supported the use of TBE in older adults at risk of falling to improve static and dynamic balance, leg muscle strength, body flexibility, and agility.
Neurophysiological studies have revealed that various brain structures, in addition to the three major systems, appear to play important roles in balance and postural control.11) For instance, postural orientation and balance may be involved in automated and reflexive spinal programs influenced by the cerebral cortex, olfactory bulb, cerebellum, brainstem, and several distinct and separate supraspinal centers.8,11,12)
Scent strongly stimulates a wide range of areas of the cerebral cortex, including the orbitofrontal cortex, the insula cortex, and the cerebellum.13-16) Moreover, scent stimulation can improve balance control and reduce falls in older adults.17,18) Essential oils of Zanthoxylum limonella (Dennst.) Alston, an evergreen tree belonging to the Rutaceae family, have been used in traditional Thai medicine.19,20) Limonene, a monoterpene with an orange aroma, is one of the main compounds in Z. limonella.19) A recent study reported that use of Z. limonella (Dennst.) Alston as an essential massage oil reduced calf muscle pain.20) One study on the effects of d-limonene on transient cerebral ischemia and physical function in stroke-prone spontaneously hypertensive rats reported that d-limonene may provide protective effects against ischemic damage and increase grip strength in rats21); however, neither Z. limonella (Dennst.) Alston nor limonene have been studied in older adults.
Kwon et al.22) proposed that scent stimulation may induce positive feelings, decrease fatigue, and improve exercise performance. Thus, the present study investigated the integrated effects of a Thai essential oil (TEO; Z. limonella (Dennst.) Alston) patch and TBE on balance, leg muscle strength, agility, and fear of falling in community-dwelling older adults at risk of falling.
This randomized controlled trial was conducted in the Physiotherapy Laboratory of Mae Fah Luang University, Chiang Rai, Thailand, between December 2021 and September 2022. The Human Research Ethics Committee of the Mae Fah Luang University approved the study protocol (COA 275/2021), which was registered in the Thai Clinical Trials Registry (TCTR20211114002).
This study complied the ethical guidelines for authorship and publishing in the Annals of Geriatric Medicine and Research.23)
Fifty-six eligible male and female non-disabled, community-dwelling older adults living in Chiang Rai, Thailand, were recruited to participate in this study through local advertisements. The older adults were asked to complete a questionnaire that included demographic information such as marital status and education level. They were also screened by a medical doctor who was blinded to the recruitment and intervention methods. The inclusion criteria were age 60 years and older and the ability to walk independently without the use of ambulation aids, a Berg Balance Scale, used to assess the risk of falling, score of <49,24) clear comprehension, and adequate vision and hearing. Older adults with a Mini-Mental State Examination score of <24,25) major unstable cardiopulmonary conditions, neurological conditions, neuropathy, anosmia, vestibular conditions, allergic reaction to the smell, or regular use of Z. limonella (Dennst.) Alston essential oil or almond base oil, cancer, and serious orthopedic conditions such as stenosis, joint infection, arthritis of the lower limbs, and lower limb discomfort of more than 4 on the numerical rating scale, as determined by oral history taking and physical examination, were excluded.
The objectives and processes of this study were explained to all participants, who provided informed written consent before their study participation.
The G*Power software (version 3.1.9.2) sample size calculation showed that 56 participants were needed to detect an effect size of 0.20 with a power of 90%, a significance level of p<0.05, two intervention groups, three measurement times, and correlations among repetitive measures.
Convenience sampling was used to select the study population, which was randomly divided into an intervention group (IG) or a control group (CG) using block randomization with block sizes of two, four, and six. The randomization results were concealed in sealed and opaque envelopes. Randomization was performed by a research assistant blinded to the assessment and intervention procedures.
A trained assessor with 5 years of experience in clinical evaluation, who was blinded to the randomization method, assessed the outcomes. The participants were evaluated at baseline, at the end of the 4-week intervention, and 1 month after the last intervention session. The adverse effects of the interventions were recorded during the 4-week intervention period.
The primary outcome measures were static and dynamic balance abilities, which were tested using a force platform (PDM-S, multifunction force measuring plate; zebris, Isny im Allg├żu, Germany) with 2,560 embedded force sensors arranged in a 35 cm├Ś54 cm matrix.26) The sampling frequency was 120 Hz, and the measured pressure had a range of 1ŌĆō120 N/cm2. The platform was calibrated before recording. The following balance parameters were extracted from the center of pressure (CoP) data during the tandem stand test (TST) and functional reach test (FRT): elliptical sway area (mm2) and CoP velocity (mm/s).27,28) Smaller elliptical sway area and CoP velocity indicated better balance ability.29) To assess static balance ability, the TST was performed. The participants stood barefoot on the force platform with the dominant foot positioned behind the non-dominant foot and arms crossed at the chest. They performed the TST with the eyes open (EO), focusing on a point 2 m ahead, and with the eyes closed (EC). Timing was terminated after 10 seconds or until the participants contacted external support, moved out of tandem stance, or opened their eyes in the TST with EC. The test under each condition was performed three times with a 1-minute interval between each test. The average value was recorded.
The FRT was used to assess dynamic balance ability.30) The participants stood barefoot on the force platform with their dominant arm close to but not touching the wall. They made a closed fist and raised their dominant arm to 90┬░ shoulder flexion. The participants were instructed to keep their feet flat on the force platform and reach as far as possible while maintaining a horizontal arm position for 3 seconds. Each participant repeated the test three times at 1-minute intervals. The average of the three trials was recorded.
The secondary outcomes were lower limb strength, agility, and fear of falling. The strengths of the hip flexors and extensors, knee flexors and extensors, and ankle plantarflexors and dorsiflexors of the dominant leg were measured using a digital pushŌĆōpull dynamometer (Baseline hydraulic dynamometer 100 lb/45 kg) as previously described.7) Each muscle was tested three times at 1-minute intervals. The average value was recorded.
The 8-foot up and go test assesses agility. The participants were asked to stand up from an armless chair and walk 8 feet as quickly and safely as they could, turn around a cone, and return to their chairs. This test was performed twice with a 30-second rest period between trials. The maximum score, in seconds, was recorded.7)
The fear of falling was assessed using the Thai version of the Falls Efficacy Scale-International (Thai FES-I). It consists of 16 items rated on a four-point Likert scale that assesses the level of concern about falling during daily activities. The total score ranges from 16 to 64, with a higher score indicating greater fear of falling.31)
The participants were randomly assigned to either the IG (receiving TEO of Z. limonella (Dennst.) Alston patch while performing 4-week TBE) or CG (4-week TBE with a control patch). One week before the experiment, the participants in both groups were acquainted with the TBE, which was designed as a group exercise with a maximum of ten participants. Participants in both groups received TBE training from three certified instructors with 5 years of TBE teaching experience. The protocol described by Areeudomwong et al.7) was followed for the TBE intervention, which included warm-up, TBE, and cool-down sessions.
The participants performed specific patterns and stepped in a square-like direction following a Thai boxing song. During TBE, a TEO patch was attached to each IG participant with three drops (0.3 mL) of Z. limonella (Dennst.) Alston essential oil (100% essential oil made by the Medical Plant Innovation Center of Mae Fah Luang University, Thailand) on their clothing in the manubrium area. A control patch containing three drops (0.3 mL) of sweet almond base oil (Chanjao Longevity Co., Ltd., Bangkok, Thailand) was attached to the clothing of the CG participants in the manubrium area. During the TBE practice, all participants in both groups were asked to inhale the scent from their patches.
IBM SPSS version 20.0 (IBM Corp, Armonk, NY, USA) was used for statistical analysis based on the intention-to-treat method. The mean, standard deviation, and 95% confidence interval (95% CI) for each outcome measure are shown. The KolmogorovŌĆōSmirnov test confirmed a normal distribution of the data. A 3├Ś2 mixed-model analysis of variance (ANOVA), with time (baseline, 4-week intervention, and 1-month follow-up) as a within-subject variable and group (IG and CG) as a between-subject variable, was used to analyze the effects of interventions on the outcome measures and to identify significant group-by-time interactions. Significant interaction effects were compared using post hoc Bonferroni pairwise comparisons. Statistical significance was set at p<0.05. The between-group effect size was calculated using CohenŌĆÖs d coefficient with effect sizes (ES) of 0.15, 0.40, and 0.75 considered small, moderate, and large, respectively.32)
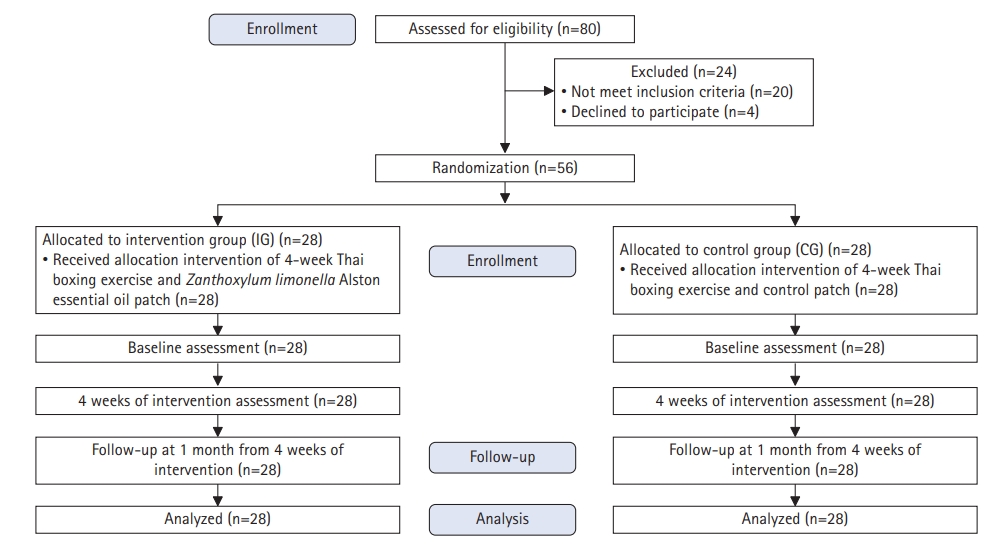
Fig. 1 depicts the flow of the participants in this study. Of the 80 participants, 56 were considered eligible and 24 were excluded. Table 1 shows that the baseline characteristics of the participants were similar across groups. The participants complied at a high rate, and there were no dropouts during the study period. The participants in this study reported no adverse effects of the interventions.
The 3├Ś2 mixed-model ANOVA revealed a significant time├Śgroup interaction effect for elliptical sway area and CoP velocity during the TST with EC (F2,108=3.32, p=0.04 and F2,108=3.81, p=0.03, respectively). The participants in IG had a greater decrease in both elliptical sway area and CoP velocity after the 4-week intervention compared to those in the CG (between-group mean difference [BGMD] elliptical sway area=57.39 mm2, 95% CI 57.39ŌĆō27.56, p=0.04; CoP velocity=3.62 mm/s, 95% CI 2.14ŌĆō112.64, p=0.001) (Fig. 2). The elliptical sway area and CoP velocity had a moderate ES of 0.56 and a large ES of 0.91, respectively.
At the 1-month follow-up, the IG had a greater reduction in CoP velocity compared to the CG, with a moderate ES of 0.69 (BGMD=3.30 mm/s, 95% CI 0.73ŌĆō5.87, p=0.01) (Fig. 2). Comparison of the baseline data at each time point in each group revealed reductions in the elliptical sway area and CoP velocity during the TST with EC at 4-week intervention (p<0.001) in both the IG and CG, and the effects in both groups on CoP velocity were maintained at the 1-month follow-up (p<0.01). While the CG showed a retention effect on the elliptical sway area (p=0.001), the IG did not (Table 2).
Although we observed no statistically significant interactions for the elliptical sway area (F2,108=0.49, p=0.61) and CoP velocity (F2,108=2.50, p=0.09) during the TST with EO, we observed a significant main effect of time, with both groups showing improved elliptical sway area and CoP velocity at all follow-up periods (p<0.05) (Table 2).
The mixed-model ANOVA did not reveal a statistically significant interaction effect for the elliptical sway area and CoP velocity during the FRT (F2,108=2.42, p=0.09 and F2,108=0.29, p=0.75, respectively) (Fig. 2). We observed a main effect of time, with both groups showing a decreased elliptical sway area (FM2,54=31.57, p<0.001) and CoP velocity (F2,54=16.07, p<0.001) after the 4-week intervention compared with those at baseline (p<0.001). At the 1-month follow-up, the IG demonstrated a reduction in CoP velocity (p=0.002), whereas the CG demonstrated a reduction in the elliptical sway area (p=0.001) (Table 2).
A 3├Ś2 mixed-model ANOVA showed a significant interaction for ankle plantarflexor strength (F2,108=2.70, p=0.04) but not for hip flexors (F2,108=0.87, p=0.42), hip extensors (F2,108=0.13, p=0.88), knee flexors (F2,108=0.07, p=0.93), knee extensors (F2,108=0.08, p=0.93), and ankle dorsiflexors (F2,108=1.44, p=0.24). The IG had a greater increase in ankle plantarflexor strength than that of the CG after the 4-week intervention (BGMD=1.67 kg, 95% CI 0.40ŌĆō2.96, p=0.01), with a moderate ES of 0.70 (Fig. 3). Comparison of lower limb strength within each group showed improved ankle plantarflexor strength alone at the 4-week intervention in both groups (p<0.05) (Table 2).
The mixed-model ANOVA showed no statistically significant interaction in the 8-foot up and go test (F2,108=0.93, p=0.07) (Fig. 2). There was a main effect of time (F2,54=6.48, p=0.003), with IG significantly increasing agility at the 1-month follow-up when compared to that at baseline (p<0.001) (Table 2).
To our knowledge, this is the first randomized controlled study to investigate the integrated effects of TEO (Z. limonella (Dennst.) Alston) and TBE as a balance exercise in older adults at risk of falling. Our findings showed that both groups demonstrated significantly increased static and dynamic balance abilities, ankle plantarflexor strength, and agility after the 4-week intervention. At the 1-month follow-up, the detraining effects of greater balance abilities were observed in both groups. The IG outperformed the CG in terms of elliptical sway area, CoP velocity during EC, and ankle plantarflexor strength. Furthermore, compared to the CG, the IG demonstrated better static balance control during EC due to a lower CoP velocity at the 1-month follow-up.
We observed that both the IG and CG had greater improvements in the elliptical sway area and CoP velocity variables of static balance in EO and EC conditions, and dynamic balance, after 4 weeks and 1-month follow-up compared to the baseline values; however, the detraining effects at 1 month were not observed in the IG for the elliptical sway area of the TST and dynamic balance. Although the studies differed in methodology and interventions, making comparisons difficult, previous studies that used martial arts-based exercises support our findings.7,33,34) Areeudomwong et al.7) showed that TBE training improved static and dynamic balance, leg strength, body flexibility, and agility in older adults compared to a fall prevention booklet intervention. Noopud et al.34) reported that traditional Thai dance prevented age-related mobility and balance declines, and risk of falls in older adults. Furthermore, Buransri and Phanpheng33) demonstrated improved dynamic balance among community-dwelling older adults after 12 weeks of practicing traditional Srichiangmai dance.
The plausible mechanisms underlying the effects of TBE on balance parameters include the following: (1) TBE involves placing light loads on the knees and ankles, requiring a body transition from double-leg standing to alternating feet or single-leg standing, emphasizing weight shifts and changing the base of support, which may challenge the postural control system7,34) and (2) TBE stepping was designed to be performed in a square shape, which may increase balance performance in multiple directions. This speculation was supported by the results reported by Dejvajara et al.35) that multidirectional step exercises could improve the dynamic balance of community-dwelling older adults.
At 4 weeks of intervention and the follow-up, neither group showed an improvement in the strength of the hip and knee flexors and extensors. This contradicts the findings of Areeudomwong et al.,7) who found greater improvement in hip and knee strength after 4-week TBE practice. Although our study used the TBE protocol of Areeudomwong et al.7) in both groups, the differences in the results may be due to differences in participant age between the studies. The average age of our participants was 75ŌĆō76 years, whereas that of the participants in the study by Areeudomwong et al.7) was 66ŌĆō67 years. A previous study proposed that muscle and physical functions may differ in community-dwelling older adults aged 75 years compared to those in younger older adults.36)
The results of this study revealed that, compared to the CG, the IG using a TEO patch while performing a 4-week TBE provided a greater improvement in static balance during the EC condition. Additionally, we observed a greater increase in ankle plantarflexor strength in the IG than that in the CG. The mechanism by which Z. limonella (Dennst.) Alston essential oil improves balance is speculative. The improved static balance parameters and ankle plantarflexor strength in the IG during EC could be attributed to widespread cerebral cortex stimulation.13-15) Numerous brain structures, in addition to the visual, vestibular, and somatosensory systems, may play a role in balance and postural control.11) Although no studies have investigated the effects of Z. limonella Alston (Rutaceae) essential oil on balance-related outcomes in older adults, previous research has shown that other types of essential oils can help with balance in older adults. Additionally, limonene may have anti-stress effects and improve cognitive function.37)
Freeman et al.17) showed that lavender and black pepper essential oils reduced postural sway in frail older adults while standing. Sakamoto et al.18) reported that lavender oil reduced the incidence of falls among older adults. Standing balance is a complex task that requires automated and reflexive spinal programs influenced by vestibular, visual, and proprioceptive senses; cognitive integration; attention and executive function; cerebellar function; and sensorimotor feedback.8,11,12) Scent is one of the strongest stimuli through a wide area of the cerebral cortex, particularly the insular cortex.37) The insula integrates and processes various sensory inputs, including olfactory, visual, vestibular, attention, and emotion processing.39,40) Z. limonella (Dennst.) Alston essential oil may activate the insular cortex and cerebellum, providing additional benefits for static balance in older adults at risk of falling. Because our TEO may stimulate different brain areas, particularly the motor cortex, it may provide a greater increase in ankle plantarflexor strength compared to that in the controls. As a result, the greater ankle plantarflexor strength in older adults may be related to a greater ability to recover balance if it is distorted unexpectedly, such as in a forward fall, which is a high-intensity perturbation.5)
The strengths of this study include the assessor-blinded randomized controlled design, which reduced the possibility of measurement bias. Furthermore, the results were not affected by participant attrition.
This study had several limitations. First, most participants in this study were female; thus, future studies should include more male participants. Second, this study only examined the effectiveness of combining Z. limonella (Dennst.) Alston essential oil with TBE on balance-related parameters; other outcomes, such as cognitive function, attention, and cardiovascular fitness should be investigated further. Third, we observed no evidence of an association between Z. limonella (Dennst.) Alston essential oil and balance, physical performance, and brain function in older adults at risk of falling. The effects of Z. limonella (Dennst.) Alston essential oil, longer intervention periods, and longer follow-up should be performed. Finally, as the study was conducted among community-dwelling older adults, the results cannot be extrapolated to those living in nursing homes or hospitals.
In conclusion, integrating Z. limonella (Dennst.) Alston essential oil while performing 4-week TBE results in greater improvements in static balance ability during EC and ankle plantarflexor strength than TBE with a sweet almond base oil in community-dwelling older adults at risk of falling.
ACKNOWLEDGMENTS
This study would like to thank the primary hospitals in the districts of Nang Lae and Mae Khao Tom, Chiang Rai, Thailand, for recruiting participants, as well as all participants for their cooperation throughout the study period.
Fig.┬Ā2.
Elliptical sway area during Tandem stance test with eyes opened (A) and eyes closed (B), center of pressure velocity during Tandem stance test with eyes opened (C) and eyes closed (D), elliptical sway area (E), and center of pressure velocity (F) during functional reach test, 8-foot up and go test (G), and Thai version of the Falls Efficacy Scale International (H) at baseline, at 4 weeks of intervention, and at 1-month follow-up, in the intervention group (IG, n=28) and control group (CG, n=28). *p<0.05, **p<0.01 for the difference between groups at each time point analyzed using the 3├Ś2 mixed-model analysis of variance.
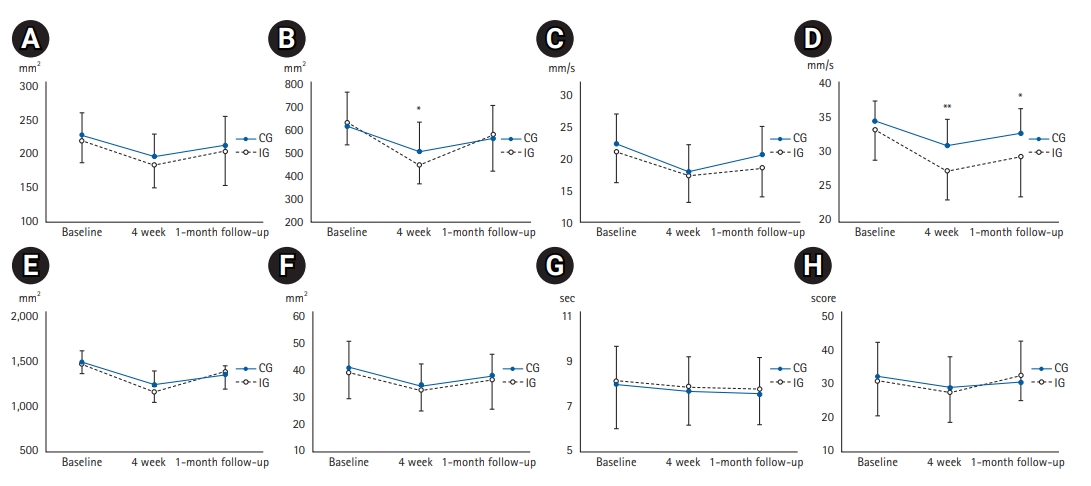
Fig.┬Ā3.
Strength of hip flexors (A), hip extensors (B), knee flexors (C), knee extensors (D), ankle plantarflexors (E), and ankle dorsiflexors (F) at baseline, at 4 weeks of intervention, and at 1-month follow-up, in the intervention group (IG, n=28) and control group (CG, n=28). *p<0.05 for the difference between groups at each time point analyzed using the 3├Ś2 mixed-model analysis of variance.

Table┬Ā1.
Baseline characteristics of the participants
Table┬Ā2.
Comparison of groups at baseline versus follow-ups for static and dynamic balance performance, agility, fear of falling, and lower limb strength analyzed using the 3├Ś2 mixed-model analysis of variance
Values are presented as mean┬▒standard deviation (95% confidence interval).
EO, eyes open; EC, eyes closed; TST, tandem stance test; FRT, functional reach test; FES-I, Falls Efficacy Scale International.
a)Integrated Zanthoxylum limonella Alston essential oil and Thai boxing exercise.
*p<0.05, **p<0.01, ***p<0.001.
REFERENCES
1. Haagsma JA, Olij BF, Majdan M, van Beeck EF, Vos T, Castle CD, et al. Falls in older aged adults in 22 European countries: incidence, mortality and burden of disease from 1990 to 2017. Inj Prev 2020;26(Supp 1):i67ŌĆō74.



2. Kumfu S, Poncumhak P. Predictive ability of the three-time stand and walk test to determine frailty and its associations with fear of falling and cognitive function in community-dwelling older adults. Ann Geriatr Med Res 2022;26:316ŌĆō22.




3. Hopewell S, Adedire O, Copsey BJ, Boniface GJ, Sherrington C, Clemson L, et al. Multifactorial and multiple component interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2018;7:CD012221.



4. Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas 2013;75:51ŌĆō61.


5. Bok SK, Lee TH, Lee SS. The effects of changes of ankle strength and range of motion according to aging on balance. Ann Rehabil Med 2013;37:10ŌĆō6.



6. Jeoung BJ. Correlation between physical fitness and fall efficacy in elderly women in Korea. J Exerc Rehabil 2015;11:151ŌĆō4.




7. Areeudomwong P, Saysalum S, Phuttanurattana N, Sripoom P, Buttagat V, Keawduangdee P. Balance and functional fitness benefits of a Thai boxing dance program among community-dwelling older adults at risk of falling: a randomized controlled study. Arch Gerontol Geriatr 2019;83:231ŌĆō8.


9. Yoo IG, Do JH. Multisensory balance training for unsteady elderly people: a scoping review. Technol Disabil 2021;33:1ŌĆō9.

10. Tantiwiboonchai N, Kritpet T, Yuktanandana P. Effects of Muay Thai aerobic dance on biochemical bone markers and physical fitness in elderly women. J Exerc Physiol Online 2017;20:188ŌĆō99.
11. Surgent OJ, Dadalko OI, Pickett KA, Travers BG. Balance and the brain: a review of structural brain correlates of postural balance and balance training in humans. Gait Posture 2019;71:245ŌĆō52.



12. Maki BE, McIlroy WE. Cognitive demands and cortical control of human balance-recovery reactions. J Neural Transm (Vienna) 2007;114:1279ŌĆō96.



13. de Araujo IE, Rolls ET, Velazco MI, Margot C, Cayeux I. Cognitive modulation of olfactory processing. Neuron 2005;46:671ŌĆō9.


14. Miyanari A, Kaneoke Y, Noguchi Y, Honda M, Sadato N, Sagara Y, et al. Human brain activation in response to olfactory stimulation by intravenous administration of odorants. Neurosci Lett 2007;423:6ŌĆō11.


15. Zatorre RJ, Jones-Gotman M, Evans AC, Meyer E. Functional localization and lateralization of human olfactory cortex. Nature 1992;360:339ŌĆō40.



16. Ferdon S, Murphy C. The cerebellum and olfaction in the aging brain: a functional magnetic resonance imaging study. Neuroimage 2003;20:12ŌĆō21.


17. Freeman S, Ebihara S, Ebihara T, Niu K, Kohzuki M, Arai H, et al. Olfactory stimuli and enhanced postural stability in older adults. Gait Posture 2009;29:658ŌĆō60.


18. Sakamoto Y, Ebihara S, Ebihara T, Tomita N, Toba K, Freeman S, et al. Fall prevention using olfactory stimulation with lavender odor in elderly nursing home residents: a randomized controlled trial. J Am Geriatr Soc 2012;60:1005ŌĆō11.


19. Charoensup R, Duangyod T, Phuneerub P, Singharachai C. Pharmacognostic specification of Zanthoxylum limonella (Dennst.) Alston: fruits and seeds in Thailand. J Adv Pharm Technol Res 2016;7:134ŌĆō8.



20. Imphat C, Woottisin N. Development of massage oil containing essential oil from Zanthoxylum limonella fruit and pain relief effect on calf muscles in healthy volunteers. J Thai Tradit Altern Med 2021;19:147ŌĆō60.
21. Wang X, Li G, Shen W. Protective effects of D-Limonene against transient cerebral ischemia in stroke-prone spontaneously hypertensive rats. Exp Ther Med 2018;15:699ŌĆō706.



22. Kwon S, Ahn J, Jeon H. Can aromatherapy make people feel better throughout exercise? Int J Environ Res Public Health 2020;17:4559.



23. Noh JH, Jung HW, Ga H, Lim JY. Ethical guidelines for publishing in the Annals of Geriatric Medicine and Research. Ann Geriatr Med Res 2022;26:1ŌĆō3.




24. Santos GM, Souza AC, Virtuoso JF, Tavares GM, Mazo GZ. Predictive values at risk of falling in physically active and no active elderly with Berg Balance Scale. Rev Bras Fisioter 2011;15:95ŌĆō101.


25. Limpawattana P, Tiamkao S, Sawanyawisuth K, Thinkhamrop B. Can Rowland Universal Dementia Assessment Scale (RUDAS) replace Mini-mental State Examination (MMSE) for dementia screening in a Thai geriatric outpatient setting? Am J Alzheimers Dis Other Demen 2012;27:254ŌĆō9.




26. Golriz S, Hebert JJ, Foreman KB, Walker BF. The reliability of a portable clinical force plate used for the assessment of static postural control: repeated measures reliability study. Chiropr Man Therap 2012;20:14.




27. Ruhe A, Fejer R, Walker B. The test-retest reliability of centre of pressure measures in bipedal static task conditions: a systematic review of the literature. Gait Posture 2010;32:436ŌĆō45.


28. Joo B, Marquez JL, Osmotherly PG. Ten-second tandem stance test: a potential tool to assist walking aid prescription and falls risk in balance impaired individuals. Arch Rehabil Res Clin Transl 2021;4:100173.



29. Areeudomwong P, Buttagat V. Proprioceptive neuromuscular facilitation training improves pain-related and balance outcomes in working-age patients with chronic low back pain: a randomized controlled trial. Braz J Phys Ther 2019;23:428ŌĆō36.



30. Ferreira S, Raimundo A, Marmeleira J. Test-retest reliability of the functional reach test and the hand grip strength test in older adults using nursing home services. Ir J Med Sci 2021;190:1625ŌĆō32.



31. Thiamwong L. Psychometric testing of the falls efficacy scale-international. Songklanagarind Med J 2012;29:277ŌĆō87.
32. Brydges CR. Effect size guidelines, sample size calculations, and statistical power in gerontology. Innov Aging 2019;3:igz036.




33. Buransri M, Phanpheng Y. Effects of Traditional Srichiangmai dance on balance and mobility in the elderly. Muscles Ligaments Tendons J 2021;11:215ŌĆō22.

34. Noopud P, Suputtitada A, Khongprasert S, Kanungsukkasem V. Effects of Thai traditional dance on balance performance in daily life among older women. Aging Clin Exp Res 2019;31:961ŌĆō7.



35. Dejvajara D, Aungkasuraphan R, Palee P, Piankusol C, Sirikul W, Siviroj P. Effects of home-based nine-square step exercises for fall prevention in Thai community-dwelling older adults during a COVID-19 lockdown: a pilot randomized controlled study. Int J Environ Res Public Health 2022;19:10514.



36. Hebert R, Brayne C, Spiegelhalter D. Incidence of functional decline and improvement in a community-dwelling, very elderly population. Am J Epidemiol 1997;145:935ŌĆō44.


37. Vieira AJ, Beserra FP, Souza MC, Totti BM, Rozza AL. Limonene: aroma of innovation in health and disease. Chem Biol Interact 2018;283:97ŌĆō106.


38. Lackner JR, DiZio P. Vestibular, proprioceptive, and haptic contributions to spatial orientation. Annu Rev Psychol 2005;56:115ŌĆō47.