|
 |
- Search
| Ann Geriatr Med Res > Volume 26(4); 2022 > Article |
|
Abstract
Background
Frailty is associated with the incidence of disability in older adults; however, few studies have investigated differences in the association of frailty with mild and severe disabilities according to Japanese long-term care insurance certification. This study separately investigated the associations between frailty and the incidence of mild and severe disabilities.
Methods
This 3-year retrospective cohort study included community-dwelling adults in Okayama City aged Ōēź65 years. We assessed frailty status using the Kihon Checklist and defined the outcomes as mild and severe disabilities according to long-term care insurance certifications. We applied multinomial logistic regression analysis to investigate the association between frailty and the incidence of mild and severe disabilities.
Results
The analysis included a total of 36,043 participants. For mild disability, the odds ratios (ORs) comparing frail to robust and prefrail to robust were 3.85 (95% confidence interval [CI], 3.36ŌĆō4.42) and 1.82 (95% CI, 1.58ŌĆō2.10), respectively. Similarly, the corresponding ORs for severe disability were 4.35 (95% CI, 3.55ŌĆō5.34) and 1.78 (95% CI, 1.43ŌĆō2.21), respectively. In the age-stratified analysis of mild disability, the pre-old group (aged 65ŌĆō74 years) with frail showed a higher association than the old-age group (aged Ōēź75 years) with frail. Regarding severe disability, the older group with frailty showed a higher association than the pre-old group with frailty.
The Japanese population is aging rapidly. In 2020, the aged population (Ōēź65 years) accounted for 28.8% of the total Japanese population and is predicted to increase to 38.1% in 2060.1) In a super-aged society such as Japan, disability in older adults is an important issue. At the individual level, disability is associated with limited activity and a decreased quality of life. Consequently, family care and financial burdens increase at the macro level.
Since 2000, the Japanese government has implemented long-term care insurance (LTCI), depending on the degree of physical and mental disability, for every Japanese adult aged Ōēź65 years. Eligibility is assessed by a questionnaire about activities of daily living (ADL) and subsequently decided by the Certification Committee of Needed Long-Term Care based on the initial computer evaluation, home-visit report, and a family doctorŌĆÖs opinion.2) The seven LTCI certification levels include support levels 1ŌĆō2 and care need levels 1ŌĆō5. Care need levels require more care than support levels, with more care required at higher levels. The LTCI certification levels are defined as follows: support level 1, ŌĆ£requiring some support for instrumental activities of daily living (IADL) but independent in basic ADLŌĆØ; care level 1, ŌĆ£declining IADL ability beyond support levels, with partial care requiredŌĆØ; care level 3, ŌĆ£significantly declining ADL and IADL abilities, with almost constant care requiredŌĆØ; and care level 5, ŌĆ£requiring care in all tasks of ADL to live.ŌĆØ The LTCI costs are increasing annually, exceeding 10 trillion yen per year in 2018.3) As the aged population is expected to increase, the early identification of high-risk individuals for future disability is essential to delay or decrease LTCI certification.
Disability is an adverse outcome of frailty.4) Older adults with frailty have a higher risk of future disability compared to those without frailty.5,6) Previous studies have shown that frailty is associated with the incidence of disability using the Japanese LTCI certification.7-9) However, most previous studies integrated all five levels of care need of LTCI certification as a single outcome, although the disability levels differ widely, ranging from almost independent in basic ADL (corresponding to care need level 1) to requiring care in all ADL tasks (level 5). Moreover, while previous studies have investigated the association of frailty with the incidence of mild and severe disabilities separately,10) few have investigated this topic according to Japanese LTCI certification.
We hypothesized that frailty is differently associated with the incidence of mild and severe disabilities. Therefore, this study investigated the association between frailty and the incidence of mild and severe disabilities separately in older adults.
This 3-year retrospective cohort study was part of the Okayama Study, a longitudinal retrospective cohort study conducted in Okayama City. Okayama City, located in western Japan, is the capital city of Okayama Prefecture. The Okayama Study investigated the relationship between behavior and LTCI certification. The basic health examination used in this study included questions related to medical history, self-rated health, lifestyle habits, and physical activity. The cohort was followed up for up to 10 years to obtain information on LTCI certification. The participants were 54,851 community-dwelling adults aged Ōēź65 years in Okayama City who underwent a basic health examination in 2006 or 2007. Okayama City had a population of 660,996 in 2006, with 125,954 (19.1%) adults aged Ōēź65 years.11) The inclusion criteria were age Ōēź65 years at the baseline measurement and residents of Okayama City. We excluded individuals who were already certified in LTCI (care need) at baseline, had missing data on frailty status or covariates, died without any LTCI certification, and were lost to follow-up (e.g., moving out of the city) during the follow-up period.
This study was approved by the Ethics Committee of the Okayama University Graduate School of Medicine, Dentistry, and Pharmaceutical Sciences and Okayama University Hospital (No. K2106-038), which waived the requirement for informed consent because this study was retrospective and the data anonymized for analysis. This study followed the ethical guidelines for authorship and publication in the Annals of Geriatric Medicine and Research.12)
We applied the Kihon Checklist (KCL) to assess frailty status. The KCL is a questionnaire developed in Japan to identify older adults who are more likely to need care. It is a self-administered questionnaire with ŌĆ£yesŌĆØ and ŌĆ£noŌĆØ responses. It consists of 25 items divided into seven domains: ADL, physical function, nutrition, oral function, housebound, cognitive function, and depressive mood. One point was added for responses to each question on whether they had a problem, with a higher total score indicating a higher risk of disability. A previous study13) reported that KCL is associated with frailty status, as defined by the Cardiovascular Health Study (CHS) frailty index, a representative evaluation of frailty status. Based on that study, we defined frail as a total KCL score of Ōēź8 points, pre-frail as 4ŌĆō7 points, and robust as 0ŌĆō3 points.
We divided LTCI certification (care need levels 1ŌĆō5) into mild (care need levels 1 or 2) and severe (care need levels 3ŌĆō5) disabilities, which were defined as the outcomes. Some definitions of the LTCI certification levels are described above. At care need levels Ōēź3, ADL and IADL become severely restricted and the burden on the family increases.14,15) Therefore, we defined the outcome as mild and severe disabilities in the new LTCI certification. We obtained information on LTCI certifications at the end of each year.
The following baseline characteristics were recorded: age, sex, comorbidities, alcohol consumption, and smoking status. The comorbidities included heart disease, renal disease, diabetes, and anemia. We selected these variables as covariates because previous studies have demonstrated that they might be confounders between frailty and future disability,16-18) and these data were available in our database.
After descriptive analysis, multinomial logistic regression analysis was used to estimate the odds ratio (OR) and 95% confidence interval (CI) for the associations between frailty status and incidence of mild and severe disabilities. Model 1 was a crude model and Model 2 was adjusted for age and sex. Model 3 was additionally adjusted for comorbidities, alcohol consumption, and smoking status.
Stratified analyses were performed to assess the association between frailty and the incidence of mild and severe disabilities by age group. We stratified the participants into two groups: pre-old (age 65ŌĆō74 years) and old (Ōēź75 years).19)
All analyses were performed using Stata/SE 17.0 (Stata Corp LP, College Station, TX, USA).
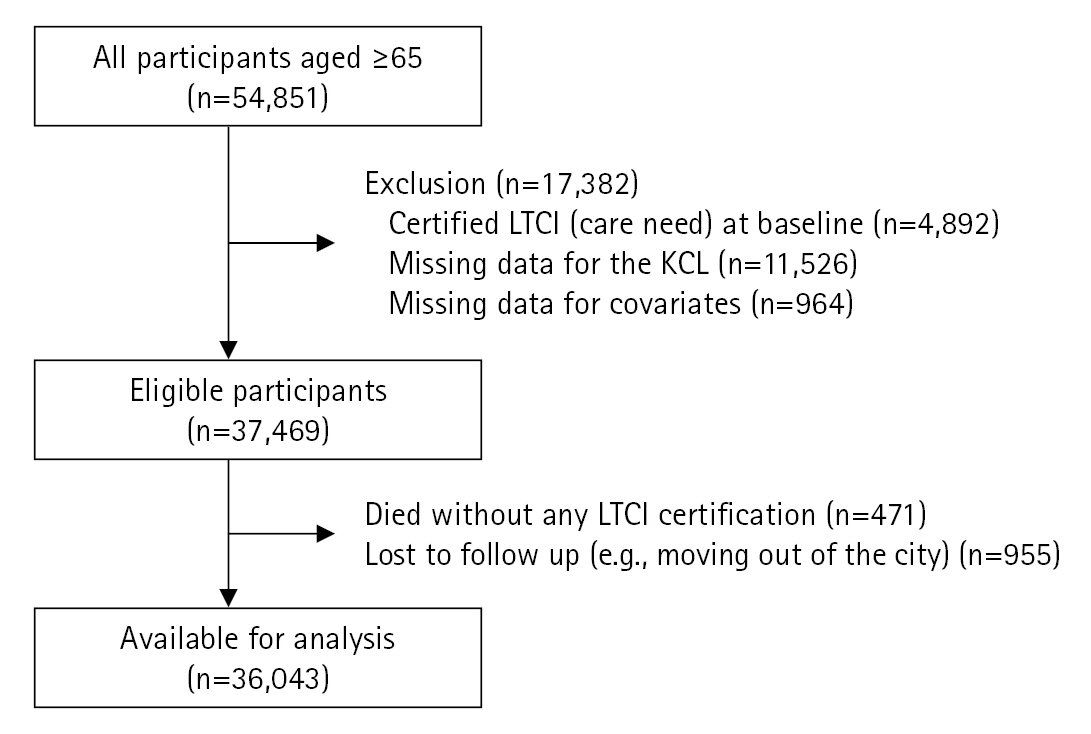
Fig. 1 shows the flow chart of the study participants. We excluded 17,382 of the 54,851 participants with certified LTCI (care need) at baseline (n=4,892), missing KCL scores (n=11,526), and missing covariate data (n=964). In addition, 471 participants died without any LTCI certification and 955 participants were lost during the 3-year follow-up. Finally, we analyzed 36,043 participants.
Table 1 shows the baseline characteristics of the participants. The median age of the participants was 74 years and 13,166 (36.5%) were male. The prevalence of frail was 21.0% (n=7,575), prefrail was 31.5% (n=11,357), and robust was 47.5% (n=17,111).
Table 2 presents the numbers of participants according to their disability level. Overall, 33,434 (92.8%) participants had no disability, 1,809 (5.0%) participants certified mild disability, and 800 (2.2%) participants certified severe disability.
Table 3 presents the results of the multinomial logistic regression analysis. In the fully adjusted model, the ORs comparing frail to robust and prefrail to robust for mild disability were 3.85 (95% CI, 3.36ŌĆō4.42) and 1.82 (95% CI, 1.58ŌĆō2.10), respectively. Similarly, the corresponding ORs for severe disability were 4.35 (95% CI, 3.55ŌĆō5.34) and 1.78 (95% CI, 1.43ŌĆō2.21), respectively.
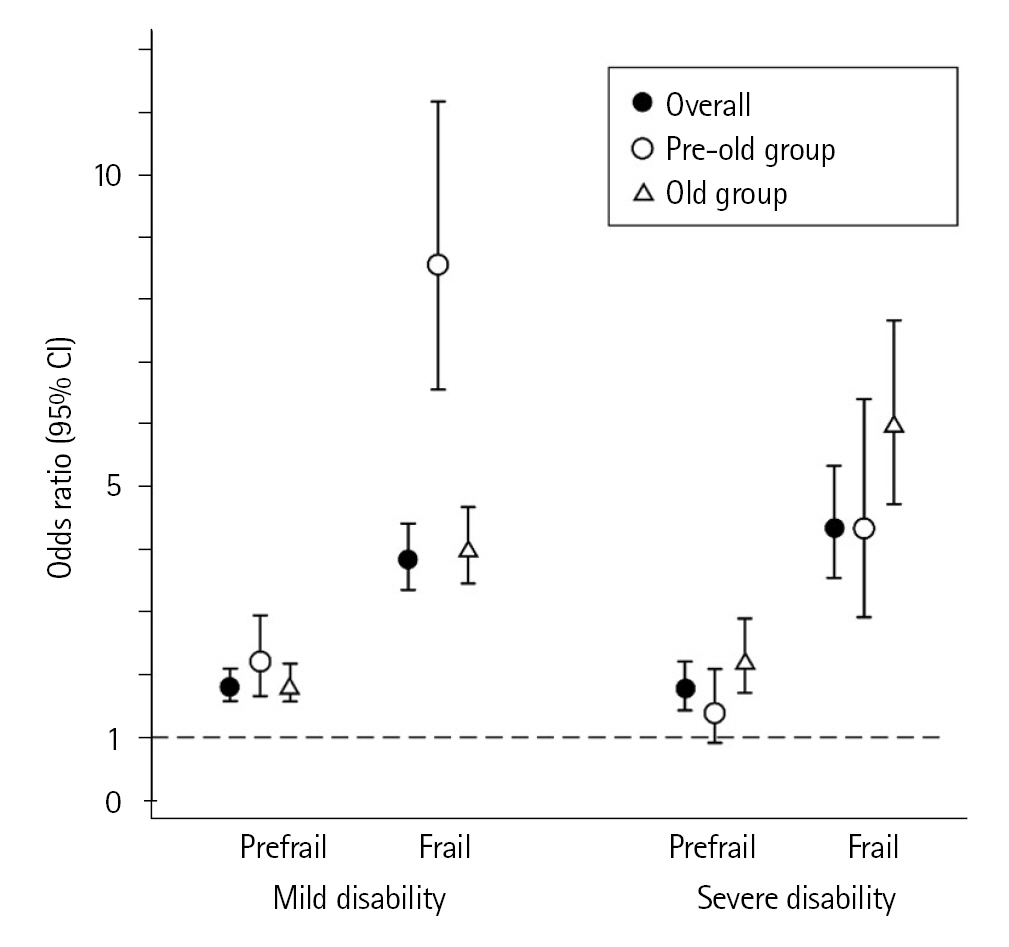
Table 4 and Fig. 2 present the results of stratified analysis by the two age groups (pre-old aged 65ŌĆō74 years; old Ōēź75 years). The pre-old group with frail (OR=8.56; 95% CI, 6.56ŌĆō11.17) showed a higher association with mild disability compared to that in the old group with frail (OR=4.02; 95% CI, 3.46ŌĆō4.68). In contrast, the old-age group with frailty showed a higher association with severe disability (OR=6.02; 95% CI, 4.73ŌĆō7.67) compared to that in the pre-old group (OR=4.33; 95% CI, 2.92ŌĆō6.41).
Using multinomial logistic regression analysis, we investigated the association between frailty and the incidence of mild and severe disabilities separately over a 3-year follow-up period. Both prefrail and frailty were associated with the incidence of mild and severe disabilities. Notably, in frail individuals, we observed different patterns of association between the pre-old and old age groups. Regarding mild disability, the pre-old group showed a higher association than the old group. Conversely, for severe disability, the old group showed a higher association than the pre-old group.
These results suggested that the older adults with frail were more likely to have severe disability. Generally, the physiological reserve gradually decreases with aging, and older adults are likely to experience decreased ADL function due to relatively minor stressor events.20) Furthermore, older age is associated with a low recovery of ADL function.20) Therefore, older adults may be more strongly affected by frailty and more likely to have severe disability compared to pre-old adults. In contrast, our results suggested that the pre-old adults with frail were more likely to have mild disability. Generally, the prevalence of frailty increases with age. A previous systematic review and meta-analysis reported an increased prevalence of frailty in Japan among adults in their late 70s and beyond.21,22) Therefore, frail individuals, despite pre-old age, may be relatively more vulnerable and their ADL function more likely to decline to mild disability, without progressing to severe disability.
Despite the different patterns between the pre-old and old age groups described above, the importance of preventing frailty may be the same across all ages. The causes of LTCI certification differ by age group.23) Specifically, lifestyle diseases (e.g., stroke, heart disease, and cancer) are more prevalent in the pre-old group, whereas the prevalence of frailty-related factors (e.g., dementia, fracture and fall, joint disorder, and weakness) is higher in the old group. Although the proportion of adults with frailty as a cause of disability may be low in the pre-old group of adults, those with frailty may be at high risk. In contrast, frailty may be a major factor directly related to severe disability in the old group. Therefore, interventions to prevent and improve frailty are essential to prevent the progression of disability.
A major strength of this study is the use of a large population-based sample and the reporting of separate ORs of frailty associated with mild and severe disabilities. However, this study has several limitations. First, more than half of the target population did not participate in health examinations. Our results might have been underestimated because the health status of older adults who did not participate in health examinations was reportedly poor.24) Second, there was the potential for unmeasured confounding. For example, other comorbidities (e.g., dementia and stroke) and social factors are reportedly associated with the incidence of disability.25,26) We could not obtain this information because this study was retrospective and used health examination data from the local government. Third, our results might have underestimated the incidence of disability since it is a factor that is strongly associated with death. This study did not include individuals who did not apply for LTCI or who became disabled due to rapid progression and died without LTCI certification. Fourth, the KCL is not an internationally representative scale for assessing frailty. Although a previous study reported an association between the CHS frailty index and reliability,13,27) the comparability requires consideration. Fifth, using a scale that primarily assesses disability may lead to errors in assessing frailty since disability is very often a consequence of frailty. Future studies should apply frailty assessment scales that are essentially independent of disability. Lastly, we were unable to determine the cause of the LTCI certification as this information was not available. Therefore, how frailty affects the incidence of disabilities remains unclear.
In conclusion, the results of our study showed that both prefrail and frail were associated with the incidence of mild and severe disabilities, with different patterns of association between the pre-old/old age groups. Our findings suggest that different interpretations and approaches to frailty should be considered by age group for disability prevention in older adults.
ACKNOWLEDGMENTS
Fig.┬Ā2.
Adjusted odds ratios and 95% confidence interval (CI) from multinomial logistic regression analysis. No disability is the reference. The pre-old group is aged 65ŌĆō74 years and the old group is aged Ōēź75 years.
Table┬Ā1.
Baseline characteristics
Table┬Ā2.
Number of participants according to disability level
| Disability (certified long-term care insurance: care need) | |||
|---|---|---|---|
| No disability | Mild disabilitya) | Severe disabilityb) | |
| Overall | 33,434 (92.8) | 1,809 (5.0) | 800 (2.2) |
| ŌĆāRobust | |||
| ŌĆāŌĆāTotal | 16,642 (97.3) | 332 (1.9) | 137 (0.8) |
| ŌĆāŌĆāŌĆāPre-old group (65ŌĆō74 y) | 11,490 (98.8) | 86 (0.7) | 52 (0.5) |
| ŌĆāŌĆāŌĆāOld group (Ōēź75 y) | 5,152 (94.0) | 246 (4.5) | 85 (1.5) |
| ŌĆāPrefrail | |||
| ŌĆāŌĆāTotal | 10,614 (93.5) | 529 (4.7) | 214 (1.8) |
| ŌĆāŌĆāŌĆāPre-old group (65ŌĆō74 y) | 5,956 (97.7) | 104 (1.7) | 39 (0.6) |
| ŌĆāŌĆāŌĆāOld group (Ōēź75 y) | 4,658 (88.6) | 425 (8.1) | 175 (3.3) |
| ŌĆāFrail | |||
| ŌĆāŌĆāTotal | 6,178 (81.6) | 948 (12.5) | 449 (5.9) |
| ŌĆāŌĆāŌĆāPre-old group (65ŌĆō74 y) | 2,384 (91.5) | 170 (6.5) | 52 (2.0) |
| ŌĆāŌĆāŌĆāOld group (Ōēź75 y) | 3,794 (76.4) | 778 (15.7) | 397 (7.9) |
Table┬Ā3.
Multinomial logistic regression for 3 years incidence of mild and severe disability
Values are presented as odds ratio (95% confidence interval).
No disability (not certified long-term care insurance) is reference; mild disability, care need level 1 or 2; severe disability, care need level 3ŌĆō5.
Model 1, crude; Model 2, adjusted for age and sex; Model 3, further adjusted for comorbidities (heart diseaseŌĆōrenal diseaseŌĆōdiabetesŌĆōanemia)ŌĆōalcohol consumption & current smoker.
Table┬Ā4.
Stratified analysis by age group
Values are presented as odds ratio (95% confidence interval).
No disability (not certified long-term care insurance) is reference; mild disability, care need level 1 or 2; severe disability, care need level 3ŌĆō5.
Adjusted for ageŌĆōsexŌĆōcomorbidities (heart diseaseŌĆōrenal diseaseŌĆōdiabetesŌĆōanemia)ŌĆōalcohol consumption & current smoker.
REFERENCES
1. Ministry of Internal Affairs and Communications. Statistical handbook of Japan 2021 [Internet]. Tokyo, Japan: Government of Japan; 2021 [cited 2022 Dec 16]. Available from: https://www.stat.go.jp/english/data/nenkan/70nenkan/index.html.
3. Ministry of Health, Labour and Welfare. Outline of long-term care insurance system [Internet]. Tokyo, Japan: Government of Japan; 2021 [cited 2022 Dec 16]. Available from: https://www.mhlw.go.jp/content/000801559.pdf.
4. Vermeulen J, Neyens JC, van Rossum E, Spreeuwenberg MD, de Witte LP. Predicting ADL disability in community-dwelling elderly people using physical frailty indicators: a systematic review. BMC Geriatr 2011;11:33.




5. Lee H, Chong J, Jung HW, Baek JY, Lee E, Jang IY. Association of the FRAIL scale with geriatric syndromes and health-related outcomes in Korean older adults. Ann Geriatr Med Res 2021;25:79ŌĆō85.




6. Kojima G. Frailty as a predictor of disabilities among community-dwelling older people: a systematic review and meta-analysis. Disabil Rehabil 2017;39:1897ŌĆō908.


7. Makizako H, Shimada H, Doi T, Tsutsumimoto K, Suzuki T. Impact of physical frailty on disability in community-dwelling older adults: a prospective cohort study. BMJ Open 2015;5:e008462.



8. Satake S, Shimokata H, Senda K, Kondo I, Toba K. Validity of total Kihon checklist score for predicting the incidence of 3-year dependency and mortality in a community-dwelling older population. J Am Med Dir Assoc 2017 18:552.e1-552.e6.

9. Kamegaya T, Yamaguchi H, Hayashi K. Evaluation by the basic checklist and the risk of 3 years incident long-term care insurance certification. J Gen Fam Med 2017;18:230ŌĆō6.




10. Kim HR, Lee H, Seong Y, Lee E, Jung HW, Park YR, et al. Longitudinal trajectory of disability in community-dwelling older adults: an observational cohort study in South Korea. BMC Geriatr 2020;20:430.




11. Okayama City. Statistics of Okayama City 2006 [Internet]. Okayama, Japan: Okayama City; 2007 [cited 2022 Dec 16]. Available from: https://www.city.okayama.jp/shisei/cmsfiles/contents/0000017/17051/000014560.pdf.
12. Noh JH, Jung HW, Ga H, Lim JY. Ethical guidelines for publishing in the annals of geriatric medicine and research. Ann Geriatr Med Res 2022;26:1ŌĆō3.




13. Satake S, Senda K, Hong YJ, Miura H, Endo H, Sakurai T, et al. Validity of the kihon checklist for assessing frailty status. Geriatr Gerontol Int 2016;16:709ŌĆō15.


14. Cabinet Office. Annual Report on the Ageing Society FY2021 [Internet]. Tokyo, Japan: Government of Japan; 2021 [cited 2022 Dec 16]. Available from: https://www8.cao.go.jp/kourei/whitepaper/w-2021/zenbun/pdf/1s2s_02.pdf.
15. Ministry of Health, Labour and Welfare. Structure of the certification of the long-term care insurance [Internet]. Tokyo, Japan: Government of Japan; 2014 [cited 2022 Dec 16]. Available from: https://www.mhlw.go.jp/topics/kaigo/kentou/15kourei/sankou3.html.
16. Liu F, Woodrow J, Loucks-Atkinson A, Buehler S, West R, Wang PP. Smoking and alcohol consumption patterns among elderly Canadians with mobility disabilities. BMC Res Notes 2013;6:218.




17. Beulens JW, Fransen HP, Struijk EA, Boer JM, de Wit GA, Onland-Moret NC, et al. Moderate alcohol consumption is associated with lower chronic disease burden expressed in disability-adjusted life years: a prospective cohort study. Eur J Epidemiol 2017;32:317ŌĆō26.




18. Ryan A, Wallace E, O'Hara P, Smith SM. Multimorbidity and functional decline in community-dwelling adults: a systematic review. Health Qual Life Outcomes 2015;13:168.



19. Ouchi Y, Rakugi H, Arai H, Akishita M, Ito H, Toba K, et al. Redefining the elderly as aged 75 years and older: proposal from the joint committee of Japan gerontological society and the Japan geriatrics society. Geriatr Gerontol Int 2017;17:1045ŌĆō7.



20. Covinsky KE, Palmer RM, Fortinsky RH, Counsell SR, Stewart AL, Kresevic D, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. J Am Geriatr Soc 2003;51:451ŌĆō8.


21. Kojima G, Iliffe S, Taniguchi Y, Shimada H, Rakugi H, Walters K. Prevalence of frailty in Japan: a systematic review and meta-analysis. J Epidemiol 2017;27:347ŌĆō53.



22. Makizako H, Nishita Y, Jeong S, Otsuka R, Shimada H, Iijima K, et al. Trends in the prevalence of frailty in Japan: a meta-analysis from the ILSA-J. J Frailty Aging 2021;10:211ŌĆō8.


23. Ministry of Internal Affairs and Communications. A comprehensive survey of living conditions 2019 [Internet]. Tokyo, Japan: Government of Japan; 2020 [cited 2022 Dec 16]. Available from: https://www.e-stat.go.jp/dbview?sid=0003441835.
24. Igarashi Y, Okuno T, Kodera K, Iritani O, Hamazaki Y, Himeno T, et al. Non-participation in health checkup and Kihon checklist predicts loss of certification-free survival in community-dwelling older adults. Geriatr Gerontol Int 2019;19:1206ŌĆō14.



25. Momose A, Yamaguchi S, Okada A, Ikeda-Kurakawa K, Namiki D, Nannya Y, et al. Factors associated with long-term care certification in older adults: a cross-sectional study based on a nationally representative survey in Japan. BMC Geriatr 2021;21:374.