 |
 |
- Search
| Ann Geriatr Med Res > Volume 26(4); 2022 > Article |
|
Abstract
Background
The intra-articular application of platelet-rich plasma and hyaluronic acid have gained popularity as treatment options for knee osteoarthritis. Although intra-articular platelet-rich plasma injections have been suggested to be superior to hyaluronic acid injections in the general population of patients with osteoarthritis, the effect of older age on both treatment options has not been thoroughly evaluated. Therefore, this study compared the results of platelet-rich plasma and hyaluronic acid injections in geriatric patients with knee osteoarthritis.
Methods
This study evaluated a total of 226 patients treated with intra-articular injections for knee osteoarthritis. The patients were divided into two groups: those who received platelet-rich plasma and those who received hyaluronic acid. All patients attended follow-up appointments at the 1st, 3rd, and 6th months.
Results
After applying the exclusion criteria, this study included 202 patients. The clinical results revealed significant improvements in all parameters compared to the baseline assessments in both groups (p<0.05). The inter-group comparisons indicated significantly lower pain in the hyaluronic acid recipients at the first and third months compared to those in patients receiving platelet-rich plasma (p<0.05).
Conclusion
Intra-articular platelet-rich plasma and hyaluronic acid injections appear to be effective in patients with knee osteoarthritis. In the geriatric patient population, hyaluronic acid showed superior effects on pain compared to platelet-rich plasma, contrary to the results in the general population.
Knee osteoarthritis is a disease seen in patients of all ages that causes a loss of function and significantly reduces the quality of life, especially in older adult patients. Moreover, its frequency has been increasing.1) Knee osteoarthritis currently affects approximately 250 million people worldwide, 46% of whom are geriatric (aged >65 years).2)
The management of knee osteoarthritis involves three primary treatment stages. Initially, exercise, weight control, and anti-inflammatory drugs are applied. When these methods prove insufficient, intra-articular therapeutics are indicated. The final management option is surgical intervention.3) Due to the progressive nature of knee osteoarthritis, lifestyle changes tend to prove inadequate and, combined with patient desire to avoid surgical treatment, intra-articular injections are the most widely used option for the treatment of knee osteoarthritis.4,5)
Previous studies have demonstrated the effectiveness of intra-articular injections.4-6) Several injection options are available, although the most commonly studied agents are hyaluronic acid (HA) and platelet-rich plasma (PRP). Previous studies have shown that PRP has superior effects in terms of pain and function in both the medium- and long-term. One possible reason for this is that the growth factors in PRP stimulate anabolic processes and increase cartilage biosynthesis.11-14) However, the effect of intra-articular application of HA may have more mechanical therapeutic mechanisms of action, including absorption, joint lubrication, anti-inflammatory effects, chondroprotection, and proteoglycan synthesis.15)
Previous studies have reported a gradual decrease in wound healing and cartilage regeneration potential and accelerated degeneration processes in aging populations.16) The decrease in the potential of this new cartilage formation raises questions regarding the potential differences in the effectiveness of biological treatments such as PRP in different age groups.
Therefore, we hypothesized that PRP may show relatively limited effects in geriatric patients aged >65 years owing to their reduced capacity for tissue regeneration. Our review of the literature did not yield any comparative studies evaluating patients aged >65 years. Therefore, the present study investigated the effects of intra-articular HA and PRP application on pain and function in geriatric patients with knee osteoarthritis.
This retrospective observational study included patients aged >65 years who were admitted to our outpatient clinic due to knee pain and diagnosed with gonarthrosis. All initially evaluated patients (n=226) were treated conservatively with intra-articular injections between January and June 2021. The minimum follow-up period for the study was 6 months. Approval to conduct this study was obtained from the Institutional Review Board of Rumeli University Ethics Committee (No. E-53938333-050.06-9245). Informed consent to use their information in scientific studies was obtained from all patients who received intra-articular injections.
This study complied the ethical guidelines for authorship and publishing in the Annals of Geriatric Medicine and Research.17)
We evaluated a total of 226 patients for inclusion in the present study. After the evaluation, 24 patients were excluded for declining to participate (11 patients), receiving intra-articular corticosteroid treatment (six patients), systemic corticosteroid use (two patients), recent febrile illness (four patients), and history of malignancy (one patient). All the patients included in the study received injections into one knee. No other injections were administered to any patient until 6 months before this injection. During the study, no treatment was applied except for the treatments mentioned.
All patients had Kellgren-Lawrence grade 2ŌĆō3 knee osteoarthritis (OA), a visual analog scale pain score of Ōēź40, and did not respond to pharmacological treatment (paracetamol 500 mg twice daily for 1 month, and topical ibuprofen twice daily). Patients whose pain did not decrease on the 15th day additionally received 400 mg ibuprofen twice daily, with the recommended use with a proton pump inhibitor. Patients whose complaints did not improve were evaluated for intraarticular injection. Patients scheduled for intra-articular knee injections were informed about the PRP and HA treatments. We selected the agent for injection according to the individual patientŌĆÖs preference. We provided the patients with detailed information about the PRP and HA injections and explained their respective advantages and disadvantages. Patient age, sex, body mass index (BMI), and clinical outcome were recorded. The inclusion and exclusion criteria are listed in Table 1.
A 4-mL ready-to-inject HA preparation (lightly cross-linked sodium hyaluronate, Monovisc; DePuy Synthes, Raynham, MA, USA) was administered to the patients in the HA group. For PRP preparation, 50 mL of venous blood was obtained, transferred to a PRP separation system containing acid citrate, and centrifuged (3200 rpm for 15 minutes), as recommended by the manufacturer. A 4-mL aliquot including the resultant buffy coat was drawn into a syringe and used for the intra-articular injection into the knee joint. In all patients, the injections were performed under aseptic conditions using an anterolateral parapatellar approach with the patients in a sitting position. The injected area was cleaned with 10% povidone iodide. A vapocoolant spray was then applied at 15 cm. The PRP and HA injections were performed using 21-G needles. HA and PRP injections were administered to each patient as a single dose throughout the study. A single physician (CP) administered all injections. After the injections, the patients were advised to restrict their activity for 24 hours, rest, and apply cold packs.
We used the patientsŌĆÖ International Knee Documentation Committee (IKDC) subjective knee evaluation form,18) 100-mm visual analog scale (VAS), and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores to evaluate the treatment results.19) Patient assessments were performed at the 1st, 3rd, and 6th months following injection. A physician (Faruk Uysal) who did not participate in the study performed the post-interventional assessments.
All continuous data are expressed as means and standard deviation, while all categorical data are expressed as frequencies (n) and percentage. Kolmogorov-Smirnov tests (with Lilliefors correction) were applied to each continuous variable to assess the presence of a normal distribution. The patientsŌĆÖ baseline demographic characteristics and mean improvement from baseline for each clinical outcome were assessed during each follow-up visit. Continuous variables were compared between the two groups using either Student t-test (for normally distributed continuous data) or Mann-Whitney U test (for non-normally distributed continuous data). Pearson chi-square tests were used to evaluate differences in the distributions of categorical variables between the two groups. All analyses were performed using IBM SPSS Statistics for Windows, version 21.0 (IBM Corp., Armonk, NY, USA). Statistical significance was set at p<0.05.
This study included a final total of 202 patients, 98 and 104 of which received PRP and HA injections, respectively (Fig. 1). The two groups were similar in terms of age, sex, BMI, and Kellgren-Lawrence OA grade (Table 2).
During the clinical evaluations, the baseline mean IKDC scores in the HA and PRP groups were 45.3┬▒10.7 and 44.2┬▒9.9, respectively. The VAS scores in the HA and PRP groups were 60.5┬▒5.5 and 59.7┬▒6.2, respectively. The WOMAC scores in the HA and PRP groups were 37.4┬▒11.6 and 36.9┬▒10.8, respectively.
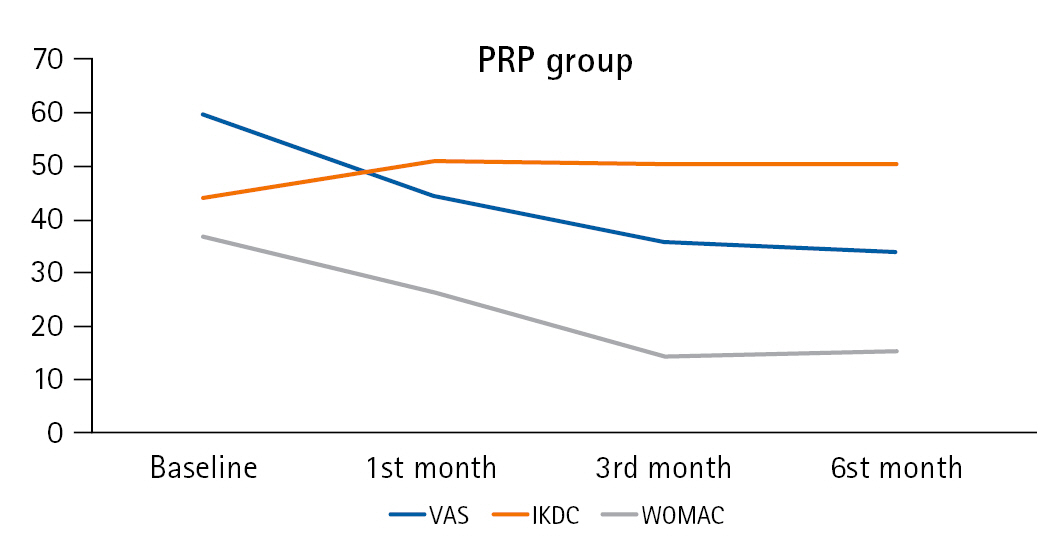
We observed significant improvements compared to baseline in all outcome parameters (IKDC, VAS, and WOMAC scores) at the 1-, 3-, and 6-month follow-up appointments in both groups. The mean VAS, WOMAC, and IKDC values at the follow-up visits compared to baseline showed significantly improved results in all scores at the 1-, 3-, and 6-month follow-up assessments in both groups (p<0.001) (Figs. 2, 3). Regarding the between-group evaluations, the average IKDC score was significantly higher in the HA group than that in the PRP group at the 3-month follow-up appointment (p=0.018). The groups showed similar IKDC results at other time points. A comparison of pain levels between the groups showed significantly lower VAS scores among the HA recipients compared to those among the PRP recipients at the 1- and 3-month follow-up appointments (p=0.039 and p=0.019, respectively). The groups showed similar VAS scores at the 6-month follow-up appointments. No significant differences in WOMAC scores were observed between the two groups at any time point (Table 3). We identified no serious side effects in any patient who received intra-articular injections.
The important role of injections in the knee joint in the treatment of knee OA is well established.2) The results of the present study demonstrated decreased pain and increased knee function compared to baseline in patients receiving intra-articular PRP and HA injections for knee OA. Moreover, the intergroup comparisons (PRP vs. HA) showed better 3-month IKDC scores in the HA group, although the WOMAC scores did not support this apparent functional difference. We observed no significant differences in other functional results. However, the HA recipients showed better pain-related outcomes compared to those in the PRP recipients throughout the first 3 months of the follow-up period. Although the efficacy of intra-articular agents remains controversial, several studies have shown that PRP is generally more effective than other agents. However, our findings indicate that this situation may be different for treatments administered in a geriatric patient population.
HA and PRP injections are the two most commonly used methods for the non-operative treatment of knee osteoarthritis. HA is a natural component of the synovial fluid and articular cartilage and is primarily responsible for providing lubrication.20) In contrast, PRP is obtained from platelet-rich blood acquired by whole-blood centrifugation. Growth factors and proteins in PRP contribute to cartilage cell regeneration and reduced rates of articular erosion.8) In addition, the contents of PRP samples obtained from different age groups differ. Previous studies reported especially high levels of tumor necrosis factor-╬▒ and matrix metalloproteinase in these different age groups, as well as increased chondrocyte responses to matrix synthesis and macrophage activation.16) In the previous study, a comparison of PRP samples showed higher growth factor, cytokine, and platelet concentrations in the younger age group compared to the older age group. The present study compared the 23ŌĆō33 years and 62ŌĆō85 years age groups. Other studies comparing the clinical results of PRP and HA applications assessed wide ranges of age groups such as 27ŌĆō84 and 33ŌĆō80 years.21,22) Although a consensus is still lacking, evaluation of these studies in terms of PRP and HA injections showed better results for PRPs. However, when evaluated together with studies reporting different PRP content and efficacy according to age group, the reliability of the results of evaluations in such a wide age range is controversial. Our study is the first to focus on the evaluation of the aging population to demonstrate that the clinical results of HA application are better than those of PRP, especially in pain scores, contrary to the previous literature.
Previous studies have assessed whether HA or PRP injections are the most effective treatment for knee OA. For example, a study including 50 patients demonstrated that intra-articular PRP injection was more effective than HA injection, in which magnetic resonance imaging (MRI) revealed reduced articular erosion reduced in patients receiving PRP.14) Moreover, previous reports showed that the application of PRP led to better functional results and reduced pain scores compared to the application of HA.11,23) However, the age distributions in these studies were not homogeneous, and our findings demonstrated better outcomes following the application of HA in older patients. Given the limited regenerative ability of the articular cartilage among the geriatric population, the mechanical lubrication caused by HA may be relatively more important and, therefore, lead to better results compared to those for PRP.
Studies evaluating the effects of PRP application on knee pain and function showed that PRP improved WOMAC and VAS scores.5,12,13) We also observed this effect in the comparisons of the follow-up results to the baseline assessments. However, none of the previous studies included control groups, as the effectiveness of PRP was investigated directly rather than through comparisons with other agents.
Previous studies failed to demonstrate significant differences in functional results between PRP and HA. However, some reports indicated that side effects are more common following PRP. The mechanism underlying these side effects has been associated with synovial reactions caused by white and red blood cells, which are likely to be present in small amounts within PRP.11,24) We observed no significant differences in functional results between the two groups. Moreover, our evaluation of the adverse effects of the treatments did not reveal any significant differences between the groups.
Recent studies have compared the use of PRP and HA dual therapy with the use of HA or PRP alone. The findings of these studies suggested that dual therapy may lead to better outcomes. However, one of the advantages of intra-articular applications is their low cost; thus, dual therapy should only be considered if its use does not result in an excessive increase in costs. In terms of cost, we observed differences between the groups within the first 3 months of the follow-up period, indicating a loss of efficacy after this point. Therefore, although the use of quarterly injections appears to be a viable option based on the current data, there is still room to discuss the use of dual therapy.25,26) Additional studies are needed to assess the costs and treatment efficacy associated with the use of these two treatment approaches before proposing new suggestions for the treatment of patients with knee OA.
The retrospective study design is a primary limitation, as it prevents definitive conclusions regarding the treatment efficacies of PRP and HA in geriatric patients. Blind injection was not possible due to the distinctly different colors of PRP and HA. Another limitation was the evaluation of single-injection HA and PRP. Previous studies showed that multiple injections are more effective, although there remains no consensus regarding this issue. Thus, a randomized controlled trial comparing single- and multiple-dose administration of PRP and HA is needed. Repeated administration reportedly shows better clinical results than single-dose administration. The present study compared patients to the control group that received intraarticular injections 1 week apart. However, another study reported no difference between the administration of single and two doses at a 1-week interval. Moreover, a consensus has not yet been reached. However, both studies reported no difference between single- and multiple-dose administration in patients with advanced osteoarthritis.21,22)
This study did not evaluate radiological improvements and MRI results in the patients; thus, we could not determine whether the observed functional and pain-related improvements were associated with the clinical characteristics of the pathology. However, as this study aimed to compare the functional outcomes of these two modalities in older patients, the lack of imaging did not prevent functional comparisons.
In conclusion, the results of this study showed that intra-articular PRP and HA injections were both effective treatment modalities in geriatric patients with knee OA, as demonstrated by the observed pain-related and functional improvements, particularly within the first 3 months after the interventions. However, HA was relatively more effective than PRP, especially in terms of pain management, in this population. These findings highlight the need for further studies evaluating larger randomized controlled series among populations with homogeneous age distributions.
ACKNOWLEDGMENTS
Fig.┬Ā2.
Improvement in HA group scores during follow-up. VAS, visual analog scale; IKDC, International Knee Documentation Committee; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index.

Fig.┬Ā3.
Improvement in PRP group scores during follow-up. VAS, visual analog scale; IKDC, International Knee Documentation Committee; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index.
Table┬Ā1.
Inclusion and exclusion criteria
Table┬Ā2.
Demographic characteristics of patients
| HA (n=104) | PRP (n=98) | p-valuea) | |
|---|---|---|---|
| Age (y) | 72.5┬▒5.4 | 0.372 | |
| Sex | 0.704 | ||
| ŌĆāFemale | 85 | 74 | |
| ŌĆāMale | 19 | 24 | |
| Body mass index (kg/m2) | 25.9┬▒2.3 | 25.2┬▒2.7 | 0.404 |
| Kellgren-Lawrence grade | 0.751 | ||
| ŌĆā2 | 55 | 54 | 0.751 |
| ŌĆā3 | 49 | 44 | |
| 100-mm VAS score | 60.5┬▒5.5 | 59.7┬▒6.2 | 0.691 |
| IKDC score | 45.3┬▒10.7 | 45.3┬▒10.7 | 0.155 |
| WOMAC total score | 37.4┬▒11.6 | 37.4┬▒11.6+ | 0.196 |
Table┬Ā3.
Clinical outcomes as improvement from baseline
| HA (n=104) | PRP (n=98) | p-valuea) | |
|---|---|---|---|
| 100-mm VAS score | |||
| ŌĆā1 month | 14.8┬▒3.2 | 14.9┬▒5.9 | 0.039 |
| ŌĆā3 months | 20.4┬▒5.5 | 23.8┬▒2.7 | 0.018 |
| ŌĆā6 months | 24.2┬▒3.0 | 25.6┬▒3.1 | 0.147 |
| IKDC score | |||
| ŌĆā1 month | 11.9┬▒8.4 | 10.5┬▒9.2 | 0.387 |
| ŌĆā3 months | 17.1┬▒9.9 | 15.1┬▒7.8 | 0.018 |
| ŌĆā6 months | 18.6┬▒8.3 | 18.1┬▒8.6 | 0.497 |
| WOMAC total score | |||
| ŌĆā1 month | 8.7┬▒4.3 | 10.4┬▒8.9 | 0.194 |
| ŌĆā3 months | 12.4┬▒10.1 | 14.3┬▒9.7 | 0.175 |
| ŌĆā6 months | 14.9┬▒5.9 | 15.2┬▒8.6 | 0.165 |
REFERENCES
1. Wallace IJ, Worthington S, Felson DT, Jurmain RD, Wren KT, Maijanen H, et al. Knee osteoarthritis has doubled in prevalence since the mid-20th century. Proc Natl Acad Sci U S A 2017;114:9332ŌĆō6.



3. Hussain SM, Neilly DW, Baliga S, Patil S, Meek R. Knee osteoarthritis: a review of management options. Scott Med J 2016;61:7ŌĆō16.



4. Goncars V, Jakobsons E, Blums K, Briede I, Patetko L, Erglis K, et al. The comparison of knee osteoarthritis treatment with single-dose bone marrow-derived mononuclear cells vs. hyaluronic acid injections. Medicina (Kaunas) 2017;53:101ŌĆō8.


5. Shen L, Yuan T, Chen S, Xie X, Zhang C. The temporal effect of platelet-rich plasma on pain and physical function in the treatment of knee osteoarthritis: systematic review and meta-analysis of randomized controlled trials. J Orthop Surg Res 2017;12:16.




6. Anil U, Markus DH, Hurley ET, Manjunath AK, Alaia MJ, Campbell KA, et al. The efficacy of intra-articular injections in the treatment of knee osteoarthritis: a network meta-analysis of randomized controlled trials. Knee 2021;32:173ŌĆō82.


7. Eymard F, Ornetti P, Maillet J, Noel E, Adam P, Legre-Boyer V, et al. Intra-articular injections of platelet-rich plasma in symptomatic knee osteoarthritis: a consensus statement from French-speaking experts. Knee Surg Sports Traumatol Arthrosc 2021;29:3195ŌĆō210.




8. Park YB, Kim JH, Ha CW, Lee DH. Clinical efficacy of platelet-rich plasma injection and its association with growth factors in the treatment of mild to moderate knee osteoarthritis: a randomized double-blind controlled clinical trial as compared with hyaluronic acid. Am J Sports Med 2021;49:487ŌĆō96.



9. Mojica ES, Markus DH, Hurley ET, Blaeser AM, Jazrawi LM, Campbell KA, et al. Estimated time to maximum medical improvement of intra-articular injections in the treatment of knee osteoarthritis: a systematic review. Arthroscopy 2022;38:980ŌĆō8.


10. Migliorini F, Driessen A, Quack V, Sippel N, Cooper B, Mansy YE, et al. Comparison between intra-articular infiltrations of placebo, steroids, hyaluronic and PRP for knee osteoarthritis: a Bayesian network meta-analysis. Arch Orthop Trauma Surg 2021;141:1473ŌĆō90.



11. Jalali Jivan S, Monzavi SM, Zargaran B, Hamidi Alamdari D, Tavakol Afshari J, Etemad-Rezaie A, et al. Comparative analysis of the effectiveness of intra-articular injection of platelet-rich plasma versus hyaluronic acid for knee osteoarthritis: results of an open-label trial. Arch Bone Jt Surg 2021;9:487ŌĆō95.


12. Bansal H, Leon J, Pont JL, Wilson DA, Bansal A, Agarwal D, et al. Platelet-rich plasma (PRP) in osteoarthritis (OA) knee: correct dose critical for long term clinical efficacy. Sci Rep 2021;11:3971.




13. Dorio M, Pereira RM, Luz AG, Deveza LA, de Oliveira RM, Fuller R. Efficacy of platelet-rich plasma and plasma for symptomatic treatment of knee osteoarthritis: a double-blinded placebo-controlled randomized clinical trial. BMC Musculoskelet Disord 2021;22:822.




14. Louis ML, Dumonceau RG, Jouve E, Cohen M, Djouri R, Richardet N, et al. Intra-articular injection of autologous microfat and platelet-rich plasma in the treatment of knee osteoarthritis: a double-blind randomized comparative study. Arthroscopy 2021;37:3125ŌĆō37.


15. Moreland LW. Intra-articular hyaluronan (hyaluronic acid) and hylans for the treatment of osteoarthritis: mechanisms of action. Arthritis Res Ther 2003;5:54ŌĆō67.



16. O'Donnell C, Migliore E, Grandi FC, Koltsov J, Lingampalli N, Cisar C, et al. Platelet-rich plasma (PRP) from older males with knee osteoarthritis depresses chondrocyte metabolism and upregulates inflammation. J Orthop Res 2019;37:1760ŌĆō70.




17. Noh JH, Jung HW, Ga H, Lim JY. Ethical guidelines for publishing in the Annals of Geriatric Medicine and Research. Ann Geriatr Med Res 2022;26:1ŌĆō3.




18. Irrgang JJ, Anderson AF, Boland AL, Harner CD, Kurosaka M, Neyret P, et al. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med 2001;29:600ŌĆō13.



19. McConnell S, Kolopack P, Davis AM. The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC): a review of its utility and measurement properties. Arthritis Rheum 2001;45:453ŌĆō61.


20. Migliore A, Blicharski T, Plebanski R, Zegota Z, Gyula G, Rannou F, et al. Knee osteoarthritis pain management with an innovative high and low molecular weight hyaluronic acid formulation (HA-HL): a randomized clinical trial. Rheumatol Ther 2021;8:1617ŌĆō36.




21. Gormeli G, Gormeli CA, Ataoglu B, Colak C, Aslanturk O, Ertem K, et al. Multiple PRP injections are more effective than single injections and hyaluronic acid in knees with early osteoarthritis: a randomized, double-blind, placebo-controlled trial. Knee Surg Sports Traumatol Arthrosc 2017;25:958ŌĆō65.



22. Patel S, Dhillon MS, Aggarwal S, Marwaha N, Jain A. Treatment with platelet-rich plasma is more effective than placebo for knee osteoarthritis: a prospective, double-blind, randomized trial. Am J Sports Med 2013;41:356ŌĆō64.



23. Li M, Huang Z, Wang S, Di Z, Zhang J, Liu H. Intra-articular injections of platelet-rich plasma vs. hyaluronic acid in patients with knee osteoarthritis: preliminary follow-up results at 6-months. Exp Ther Med 2021;21:598.



24. Han SB, Seo IW, Shin YS. Intra-articular injections of hyaluronic acid or steroids associated with better outcomes than platelet-rich plasma, adipose mesenchymal stromal cells, or placebo in knee osteoarthritis: a network meta-analysis. Arthroscopy 2021;37:292ŌĆō306.


- TOOLS








