The Clinical Frailty Scale as a Risk Assessment Tool for Dysphagia in Older Inpatients: A Cross-Sectional Study
Article information
Abstract
Background
Dysphagia is a common problem with potentially serious consequences including malnutrition, dehydration, pneumonia, and death. However, there are challenges in screening for dysphagia in older adults. We assessed the feasibility of using the Clinical Frailty Scale (CFS) as a risk assessment tool for dysphagia.
Methods
This cross-sectional study was conducted at a tertiary teaching hospital from November 2021 to May 2022 and included 131 older patients (age ≥65 years) admitted to acute wards. We used the Eating Assessment Tool-10 (EAT-10), which is a simple measure for identifying individuals at risk of dysphagia, to assess the relationship between EAT-10 score and frailty status as measured using the CFS.
Results
The mean age of the participants was 74.3±6.7 years, and 44.3% were male. Twenty-nine (22.1%) participants had an EAT-10 score ≥3. The CFS was significantly associated with an EAT-10 score ≥3 after adjusting for age and sex (odds ratio=1.48; 95% confidence interval [CI], 1.09–2.02). The CFS was able to classify the presence of an EAT-10 score ≥3 (area under the receiver operating characteristic [ROC] curve=0.650; 95% CI, 0. 544–0.756). The cutoff point for predicting an EAT-10 score ≥3 was a CFS of 5 according to the highest Youden index, with a sensitivity of 82.8% and a specificity of 46.1%. The positive and negative predictive values were 30.4% and 90.4%, respectively.
Conclusion
The CFS can be used as a tool to screen for the risk of swallowing difficulty in older inpatients to determine clinical management encompassing drug administration routes, nutritional support, prevention of dehydration, and further evaluation of dysphagia.
INTRODUCTION
The ability to swallow is an essential aspect of human physiology and necessary for maintaining proper nutrition and hydration.1) Dysphagia, or difficulty swallowing, is a common problem that can have serious consequences, including malnutrition, dehydration, pneumonia, and even death.2) In addition to its negative health effects, dysphagia can affect the quality of life in older adults.3) Swallowing difficulty can lead to social isolation and decreased enjoyment of meals, which are important aspects of overall well-being.4,5)
As dysphagia disproportionately affects older adults with frailty, identifying dysphagia in frail individuals is crucial. The prevalence of dysphagia is up to one-third among community-dwelling older individuals.6) As frail older adults are more likely to have multiple chronic conditions and functional impairments,7) these populations are more likely to experience the adverse consequences of dysphagia.8) Furthermore, because exercise and nutritional support are important strategies to prevent the progression of frailty and improve functional status,9-11) dysphagia may preclude the beneficial impact of such interventions on frailty.
However, challenges exist in screening for dysphagia in older adults. Individuals at risk may be unable to report symptoms of dysphagia because of cognitive or functional impairments. In addition, the symptoms of dysphagia can be vague and nonspecific, making it difficult to diagnose without specialized testing. Furthermore, individuals may not seek medical attention for dysphagia unless their symptoms are severe, which can delay diagnosis and treatment. This can be particularly problematic in older adults with frailty who may not have easy access to healthcare providers or who may not be under the care of a geriatric specialist.
The Eating Assessment Tool-10 (EAT-10) is a simple and widely used screening measure for identifying individuals at risk of dysphagia.12) We postulated that the EAT-10 could be used as an easy screening tool for older adults with or without frailty. In this study, we assessed the relationship between the EAT-10 score and frailty status as measured using the Clinical Frailty Scale (CFS) in patients aged ≥65 years admitted to the acute wards at Asan Medical Center, a tertiary teaching hospital in Korea.
MATERIALS AND METHODS
Study Design and Participants
This cross-sectional study was conducted at Asan Medical Center, a tertiary teaching hospital in Seoul, Korea, between November 2021 and May 2022. The Institutional Review Board of Asan Medical Center reviewed and approved the study protocol (IRB No. 2022-1400) and waived the requirement for informed consent because evaluating the general health status of patients at admission is a routine procedure and no additional harm was anticipated. A convenience sample of older patients (age ≥65 years) admitted to acute wards who underwent a brief geriatric risk evaluation by a geriatric nurse specialist was included. Patients who were hemodynamically unstable or were approaching death were excluded from the study. Additionally, patients with neurological diseases such as stroke and Parkinson's disease, which can directly cause dysphagia, and patients hospitalized for respiratory infections and upper gastrointestinal diseases, which can temporarily cause or worsen dysphagia, were excluded from the analysis.
This study complied the ethical guidelines for authorship and publishing in the Annals of Geriatric Medicine and Research.13)
Patient Assessments
The CFS and EAT-10 were measured once on the day after admission by a trained geriatric nurse specialist and an occupational therapist, respectively.
Among the many tools available for measuring frailty, the CFS is a simple tool with a score ranging from 1 to 9 with brief descriptors and pictographs. It was developed to stratify older patients according to their relative degrees of frailty.14) After its initial validation, the CFS has been widely used in multiple settings to predict the clinical outcomes of the aging population.15) We used the Korean-translated version of the CFS, the construct validity of which has been established in Korean geriatric patients.16,17)
Dysphagia screening was performed using the EAT-10.18) The EAT-10 consists of 10 questions that are scored from 0 (no problem) to 4 (severe problem), resulting in a total score ranging from 0 to 40. Previous studies considered an EAT-10 score of ≥3 as positive for screening.8,18) In contrast, this study, defined each EAT-10 question with a score ≥1 as positive. The Korean translation of EAT-10 has also been validated in Korea.19) The baseline patient characteristics, including demographic, anthropometric, and laboratory data, were retrieved from electronic medical records. The Geriatric Nutritional Risk Index (GNRI) was calculated using the following formula derived from previous studies20,21):
GNRI = 1.489 × albumin (g/L) + 41.7 × (body weight/WLo).
WLo (Ideal weight calculated from the Lorentz equations) was calculated as was calculated as follows:
Statistical Analysis
All statistical analyses were performed using IBM SPSS Statistics for Windows, version 21.0 (IBM Corp., Armonk, NY, USA). Continuous variables are expressed as mean±standard deviation, while discrete variables are presented as counts and percentages. Statistical differences were assessed using t-test, Pearson chi-square test, or Fisher exact test. We performed binary logistic and linear regression analyses to evaluate the relationship between the EAT-10 score and frailty status as measured by the CFS. To assess the ability to classify for the presence of an EAT-10 score ≥3 and positivity for each question of the EAT-10, we performed receiver operating characteristic (ROC) analyses using the CFS as the test variable and these outcomes as the state variables. The cutoff point of the CFS was determined according to the highest Youden index, and the sensitivity, specificity, and positive and negative predictive values were determined. All statistical analyses were two-tailed, and statistical significance was set at p<0.05.
RESULTS
General Characteristics of the Study Participants
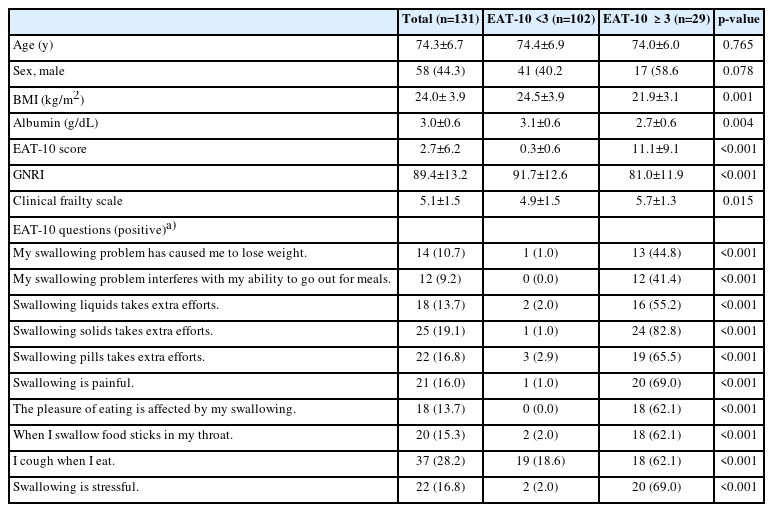
During the study period, we assessed the EAT-10 and CFS in 131 patients aged ≥65 years who were admitted to acute wards. The mean age of the patients was 74.3±6.7 years and 44.3% were male. Twenty-nine (22.1%) patients had an EAT-10 score ≥3. The general characteristics of the study participants with EAT-10 scores <3 or ≥3 are presented in Table 1. Patients with EAT-10 scores ≥3 had significantly lower body mass index and albumin levels than those with EAT-10 scores <3. In addition, their CFS scores were higher and they had a greater risk of malnutrition.
Relationship between EAT-10 Score and Frailty Status
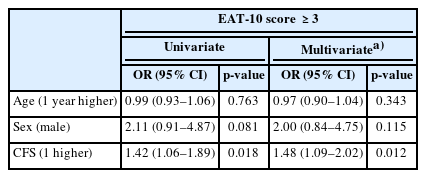
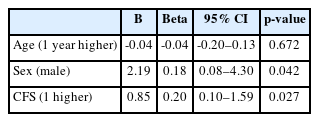
To identify the factors associated with an EAT-10 score ≥3, we performed binary logistic regression analysis. After adjusting for age and sex, CFS was significanlty associated with an EAT-10 ≥3 (odds ratio=1.48; 95% confidence interval [CI], 1.09–2.02) (Table 2). Linear regression analysis performed to identify factors associated with the EAT-10 score revealed that CFS was significantly associated with EAT-10 score (p=0.027) (Table 3).
CFS as a Dysphagia Indicator
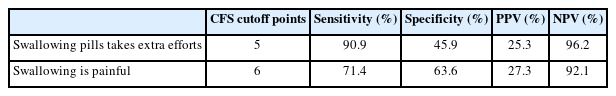
CFS was able to classify the presence of an EAT-10 score ≥3 (area under the ROC curve [AUC]=0.650; 95% CI, 0.544–0.756) (Fig. 1). A CFS score of 5 was the cutoff score for predicting the presence of an EAT-10 score ≥3, according to the highest Youden index, with a sensitivity of 82.8% and a specificity of 46.1%. The positive and negative predictive values were 30.4% and 90.4%, respectively. The CFS was able to predict positivity for two questions of the EAT-10 (Fig. 2); namely pill swallowing difficulty (AUC=0.700; 95% CI, 0.590–0.810) and painful swallowing (AUC=0.718; 95% CI, 0.603–0.833). The CFS cutoff score according to the highest Youden index for each question and the corresponding sensitivity, specificity, and positive and negative predictive values are shown in Table 4.
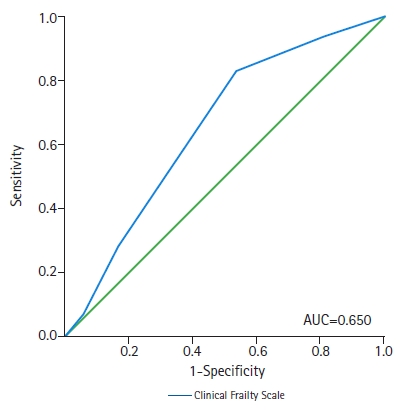
Receiver operating characteristic (ROC) curve for the presence of EAT-10 score ≥3. AUC, area under ROC curve; EAT-10, Eating Assessment Tool-10.
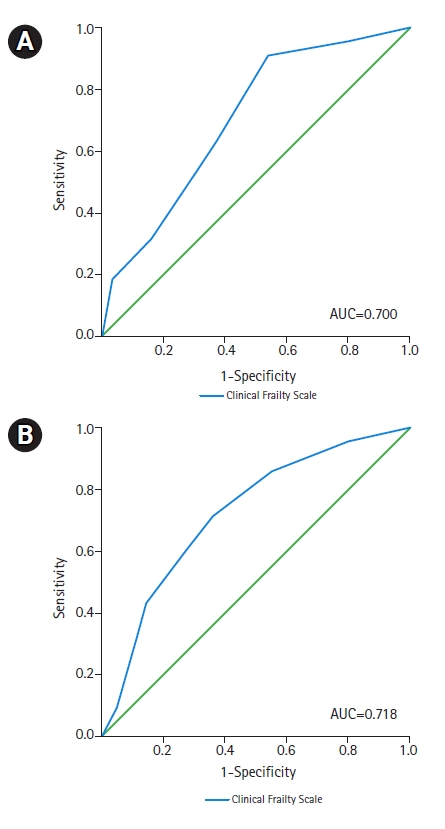
Receiver operating characteristic (ROC) curves for positivity for EAT-10 questions: (A) pill-swallowing difficulty and (B) painful swallowing. AUC, area under ROC curve; EAT-10, Eating Assessment Tool-10.
DISCUSSION
Our results showed a higher risk of malnutrition among older patients with an EAT-10 score ≥3 admitted to acute wards. CFS score was significantly associated with the EAT-10 score, and a CFS of 5 was the cutoff score predicting the presence of an EAT-10 score ≥3. Additionally, the CFS could also be used to predict pill-swallowing difficulty and swallowing pain.
Dysphagia is common in older adults and can occur due to problems during various eating phases. Oropharyngeal dysphagia commonly occurs after stroke and during the course of many neurodegenerative diseases such as dementia and Parkinson disease.22) The prevalence of dysphagia varies among studies. Several meta-analyses have reported estimated prevalence rates of dysphagia of >10% and >20% in community-dwelling and hospitalized older patients, respectively.6,23) Dysphagia is known to increase the risk of malnutrition.24) As nutrition is considered a cornerstone in the concept of the “cycle of frailty,” a self-deteriorating cycle of negative energy balance, reduced physical activity, and further decline in physical performance,25,26) several studies have suggested that dysphagia is associated with frailty.27,28) In addition, dysphagia is a risk factor for the development of aspiration pneumonia,29) and increased dysphagia is associated with reduced health-related quality of life.30) Therefore, in an aging society, identifying older adults at risk of dysphagia, performing diagnostic tests, and administering appropriate treatments based on the test results are important.
Frailty, which reflects a decline in physiological reserves, is strongly associated with biological age,31) concurrent medical conditions, morbidity, and reduced survival in older adults.32,33) Frailty is generally assessed through different operational definitions, and the prominent models encompass physical and biological models, deficit accumulation models, and multidimensional biopsychosocial models.34) Among the many tools for measuring frailty, the CFS has the advantage of being able to intuitively assess the frailty status of patients. Studies have shown that the CFS can predict vulnerability to various adverse geriatric outcomes in both community-dwelling older adults and hospitalized patients. As shown in the present study, the CFS may be useful for screening for dysphagia and stratifying hospitalized older patients according to frailty status.
Assessing the presence of dysphagia in hospitalized older adult patients is essential for several reasons. First, the oral route is widely utilized and favored for drug administration owing to its benefits, including its noninvasive nature, patient compliance, and convenience in drug delivery.35) Therefore, the presence or absence of dysphagia must be evaluated in hospitalized older adult patients who must maintain the effects of drugs through steady drug administration. The use of the CFS at the time of hospitalization and using a defined cutoff point may effectively identify patients who require evaluation for dysphagia. Following evaluation, interventions such as changing the dosage form or administration route for patients with dysphagia can be considered.
Second, screening acutely hospitalized older patients at high risk for dysphagia is useful for reducing the risk of aspiration or malnutrition and identifying patients who can benefit from nutritional interventions. Malnutrition has a severe impact on recovery from disease and is associated with increased morbidity and mortality.36,37) Poor nutritional status is also associated with the development of geriatric syndrome.38) Previous studies confirmed the role of malnutrition in the occurrence of delirium and pressure ulcers in hospitalized older patients.39,40) Additionally, malnutrition upon hospital admission is a significant risk factor for falls during hospital stays.41) A cutoff point is useful for identifying high-risk patients requiring accurate testing and close observation.
Third, older adults have decreased thirst sensation and a decline in urinary concentration ability2); if additional functional problems are present, dehydration can easily occur. Dehydration is very common, particularly in patients with dysphagia, with the prevalence of dehydration ranging from 44% to 75%.42,43) As a result, dehydration ranks as one of the top 10 most commonly diagnosed medical conditions leading to hospital admission among older adults.44) Dehydration is also associated with the development of geriatric syndromes such as delirium and falls.45,46) Identification of the risk of dysphagia in hospitalized older adult patients is necessary to reduce the risk of dehydration.
Given the challenges in screening for dysphagia in older adults, particularly in those with cognitive or functional impairments, the use of the CFS as a dysphagia indicator can aid healthcare providers in identifying at-risk patients and facilitating early interventions. By incorporating CFS assessment into routine geriatric care, healthcare providers can enhance their ability to detect swallowing difficulties in frail older adults, ultimately reducing the risks of malnutrition, dehydration, pneumonia, and other adverse consequences of dysphagia. Additionally, timely intervention may improve the effectiveness of exercise and nutritional support in preventing the progression of frailty and improving patient functional status. Future research should explore the implementation of CFS-based screening strategies in various healthcare settings and their impact on dysphagia management and frailty outcomes.47)
Of the 131 patients included in the study, only two underwent a videofluoroscopic swallow study (VFSS), a substantially low number considering the prevalence of patients at risk according to the EAT-10 questionnaire. Many factors may contribute to the potential underuse of formal evaluation methods for treating dysphagia, including the current bottleneck in VFSS volume per day in Korean academic hospitals.
Although the pathophysiology of dysphagia is complex and the spectrum of its severity is wide, some issues can be addressed using this simple scale. Suspecting dysphagia in patients, especially in those with advanced frailty, may prevent delayed recognition of dysphagia after pneumonia caused by repeated aspiration. Additionally, this approach has the advantage of being widely applicable in real clinical settings due to its relatively simple predictive nature. A clinical suspicion of dysphagia using the CFS may provide healthcare professionals with an early opportunity to perform formal, in-depth assessments of this condition in patients, especially those with medical conditions that affect their swallowing ability.
This study has several limitations. First, the cross-sectional design limited our ability to establish causality between the EAT-10 score and frailty status as measured by the CFS. Longitudinal studies are needed to investigate the causal relationship between dysphagia and frailty in older adults. Second, this study was conducted at a single tertiary teaching hospital in South Korea, which may limit the generalizability of the findings to other healthcare settings and populations. Future research should include larger and more diverse samples from multiple centers to enhance the generalizability of the results. Third, this study relied on self-reported measures to assess dysphagia using the EAT-10, which may have been influenced by recall bias and subjectivity. Objective assessments of swallowing function, such as VFSS, would provide more accurate information on dysphagia presence and severity. Finally, we excluded patients who were hemodynamically unstable or approaching death, which may have led to an underestimation of the prevalence of dysphagia and its association with frailty in the overall older adult population.
In conclusion, the CFS can be used as a risk assessment tool for dysphagia in hospitalized older adults. The presence or absence of dysphagia has important implications for determining the drug administration route, nutritional intervention, and prevention of dehydration in acutely hospitalized patients. Therefore, the CFS can be effectively used to determine whether interventions can be performed to improve the prognosis of older inpatients.
Notes
CONFLICT OF INTEREST
Hee-Won Jung cofounded Dyphi Inc, a startup company developing sensor technologies for human movement and robotics. Otherwise, authors declare that there are no potential conflicts of interest.
FUNDING
None.
AUTHOR CONTRIBUTIONS
Conceptualization, MK, EL, IYJ, HWJ; Data curation, SHJ, YKP, JYB, SHL, HWJ; Investigation, SHJ, YHK, YS, SHL, HWJ; Methodology: MK, EL, IYJ, HWJ; Project administration: SHJ, YKP, JYB, YHK, YS, SHL; Supervision, EL, IYJ, HWJ; Writing–original draft: MK, HWJ; Writing–review & editing: MK, SHJ, YKP, JYB, YHK, YS, SHL, EL, IYJ, HWJ.