Effects of the COVID-19 Pandemic on Psychological Status and Quality of Life among Participants of the Malaysian Elders Longitudinal Research (MELoR) Study
Article information
Abstract
Background
This study aimed to identify differences in quality of life before and during the coronavirus disease 2019 (COVID-19) pandemic and determine the influence of psychological status on the observed changes in the quality of life among older adults.
Methods
The Malaysian Elders Longitudinal Research study recruited Malaysians aged at least 55 years from 2013 to 2015. Follow-ups were conducted between September and December 2020. Quality of life was determined using the 12-item Control, Autonomy, Self-Realization, and Pleasure questionnaire. Psychological statuses were assessed using the 21-item Depression Anxiety and Stress Scale, 15-item Geriatric Depression Scale, and 4-item Perceived Stress Scale.
Results
This study included data from 706 individuals (mean age, 73.3±6.8 years). We observed reduced quality of life and increased anxiety among 402 (43.1%) and 144 (20.9%) participants, respectively. Participants felt “out of control,” “left out,” “short of money,” and “life was full of opportunities” less often and could “please themselves with what they did” more often. Multivariate analyses revealed increased depression, anxiety, and stress as independent risk factors for reduced quality of life.
Conclusion
Individuals with increased depression, anxiety, and stress levels during the pandemic experienced a worsening quality of life. Thus, the development of effective strategies to address the mental health of older adults is needed to mitigate the effects of the pandemic on their quality of life.
INTRODUCTION
The emergence of novel severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) represents a major public health threat globally. Preventive measures against the transmission of the deadly virus have recommended shielding older adults, physical distancing, and infection control measures.1) Albeit necessary, the enforcement of social isolation has significantly altered day-to-day living among older adults.2) Strict movement control orders (MCOs) in Malaysia were abruptly implemented with limited forewarning over 18 months, depriving older persons of their usual routines, outdoor activities, social interactions, and family gatherings. All these, alongside the fear or effect of contracting coronavirus disease 2019 (COVID-19) and the loss of family members and friends due to COVID-19, have raised concerns of unseen adverse effects on the mental health and quality of life (QoL) of older adults.
Studies conducted throughout the COVID-19 pandemic have reported worsening of QoL indicators in various populations.2,3) In a study of Italian older adults with dementia, Tondo et al.4) found that lockdowns affected social interactions, increased obstacles in coping with daily life constraints and routine disruption, and also restricted access to healthcare. As such, older adults were faced with the double-edged sword of being unable to leave their premises and inability to cope with social isolation.5) Longer lockdown durations, like that experienced in Malaysia, were associated with increased neuropsychiatric symptoms, resulting in behavioral disturbance.6) Correspondingly, several studies described increased anxiety and depressive symptoms among older adults throughout the pandemic, which could have stemmed primarily from the fear of contracting COVID-19, fear for the safety and well-being of their next of kin, and fear for the future.5) Furthermore, the common stressors reported by older adults included quarantines/movement restrictions, worry for others, and seclusion.7) Physical activity restriction and lifestyle changes have led to reduction in psychological health and quality of life among older adults.8)
However, other studies reported little to no adverse effects of the pandemic on the QoL and mental health in older adults. For instance, in their study of Swedish older adults, Kivi et. al.9) reported higher than average well-being compared to previous years. Similarly, a study of Polish and German older adults reported better QoL, and well-being compared to the younger population. The study also described lower trait anxiety, higher ability to relax, and higher optimism among older adults than their younger counterparts.10)
The effects of the pandemic on the mental health of the global population are expected to persist well beyond the pandemic.11,12) Further, the negative effects of depression and anxiety on QoL increase with age.13) Quantification of the changes in psychological status associated with the COVID-19 pandemic and its effect on QoL will be invaluable for resource allocation and informing policymakers. Therefore, this study aimed to determine the QoL before and during the COVID-19 pandemic and further explore the role of psychological status in relation to these changes among older adults in Malaysia.
MATERIALS AND METHODS
Study Design
This study utilized a longitudinal cohort study design involving two measures: changes in QoL and psychological status. We operationally defined changes in QoL within the context of this study as a difference in overall QoL scores over 6 to 8 years of follow-up using the 12-item Control Autonomy Self-Realization and Pleasure (CASP-12) scale. Psychological status within the context of this study included measures of depression, anxiety, and stress, which we operationally defined as changes in depression, anxiety, and stress scores. We obtained ethics approval from the University of Malaya Medical Centre Medical Ethics Committee and the study was conducted in accordance with the Principles of the Declaration of Helsinki 1983 (MREC ID: 20191231-8121).
This study complied the ethical guidelines for authorship and publishing in the Annals of Geriatric Medicine and Research.14)
Study Population
The Transforming Cognitive Frailty into Later-Life Self Sufficiency (AGELESS) study is an ongoing longitudinal study of aging formed by combining three pre-existing cohorts.15) We extracted only information from participants originally included in the Malaysian Elders Longitudinal Research (MELoR) study as anxiety and QoL were not included in the previous waves of the other original cohorts. The first wave of this study involved face-to-face interviews from 2013 to 2015. The study recruited 1,565 participants aged above 55 years and older via stratified simple random sampling from the parliamentary electoral rolls of the Petaling Jaya North, Petaling Jaya South, and Lembah Pantai constituencies. The inclusion criteria were age 55 years and older and the ability to provide written informed consent.16) Follow-up interviews were conducted virtually during the COVID-19 MCO between September and December 2020.15)
Quality of Life Measure
We applied the CASP-12 age-specific tool to measure changes in QoL. The CASP-12 was derived from the CASP-19, which was utilized in the SHARE studies.17) The CASP-12 consists of two domains (control/autonomy and self-realization/pleasure) assessed through 12 items on a 4-point Likert-type scale ranging from often to never. Each item consists of a statement to denote how the participant feels about or perceives their life. Some of the items involved reverse scoring. The total scores ranged from 0 to 36, where higher scores indicated a higher QoL.
Psychological Measures
Anxiety
The 21-item Depression Anxiety and Stress Scale (DASS-21) was administered at baseline. The scale includes three subscales: depression, anxiety, and stress. Each subscale consisted of seven items rated on a 4-point Likert scale ranging from 0 (did not apply to me at all) to 3 (applied to me very much, or most of the time). Only the seven items in the anxiety subscale were administered during follow-up virtual interviews.18) Thus, the maximum total score for each subscale was 21.
Depression
As mentioned above, depression was determined using the DASS-Depression scale at baseline and the 15-item Geriatric Depression Scale (GDS-15). The GDS-15 has been extensively used to measure depression among older adults, with each item drawing a dichotomous response of “Yes” or “No.” Positive responses in 10 items and negative responses in the remaining five items were assigned scores of one, with scores of five or more indicating the presence of depression.19,20)
Stress
Stress was measured with the DASS-Stress scale at baseline and the Perceived Stress Scale (PSS-4) at follow-up.21) The four-item scale measure stress based on a Likert-type scale ranging from 0 (never) to 4 (very often). Scoring was reversed for positive items. The maximum attainable score is 16, with higher scores denoting higher levels of stress.
Data Analysis
We performed the data analysis using IBM SPSS Statistics for Windows, version 27.0 (IBM Corp., Armonk, NY, USA). We subtracted the total anxiety scores for Wave 1 from those in Wave 4 to calculate the change in anxiety scores. Individuals with changes in anxiety scores of one and above were then categorized into the increased anxiety group, while those with a change in anxiety scores of zero or less were categorized into the no-change or decreased anxiety group. Since depression and stress were assessed at baseline with DASS-21 depression and stress subscales, respectively, and at follow-up with GDS-15 and PSS-4, respectively, we harmonized the baseline and follow-up data by categorizing the scores into four groups utilizing the 50th, 75th and 95th percentile cut-offs for DASS-Depression and DASS-Stress scores obtained at baseline and GDS-15 and PSS-4 at the Wave 4 follow-up. It was not possible to obtain four equal groups due to the ordinal nature of the data and the large proportion of participants with total scores of 0 for DASS-anxiety, DASS-depression, and PSS-4. Thus, we categorized individuals who moved up the centile groups into the increased depression or stress groups, while those who remained in the same group or dropped to a lower group were categorized into the no change/decreased depression or stress groups. We then performed general descriptive and frequency analyses for both categorical and continuous variables; the former is presented as frequencies and percentages and the latter as means and standard deviation. Hypothesis testing was conducted using Friedman and Wilcoxon signed-rank tests to determine the differences in psychological status and QOL between baseline and follow-up. We then used linear regression analyses to determine the influence of psychological status at follow-up and changes in psychological status on alterations in QoL scores. The parameter estimate, B, and 95% confidence interval (CI) were presented. B was considered the correlation or adjusted correlation coefficient in the unadjusted and adjusted models for continuous variables in the total anxiety, depression, and stress scores, while depression and stress were considered the mean difference for the dichotomous independent variables of increased anxiety. We considered the relationships in the linear regression models to be statistically significant if the 95% CI did not cross the null value. The potential confounders for multiple linear regression analyses were selected from variables with p<0.05 in Table 1. We created dummy variables for categorical variables utilized within the multiple linear regression models. Statistical significance was set at p<0.05.
RESULTS
Participant Characteristics
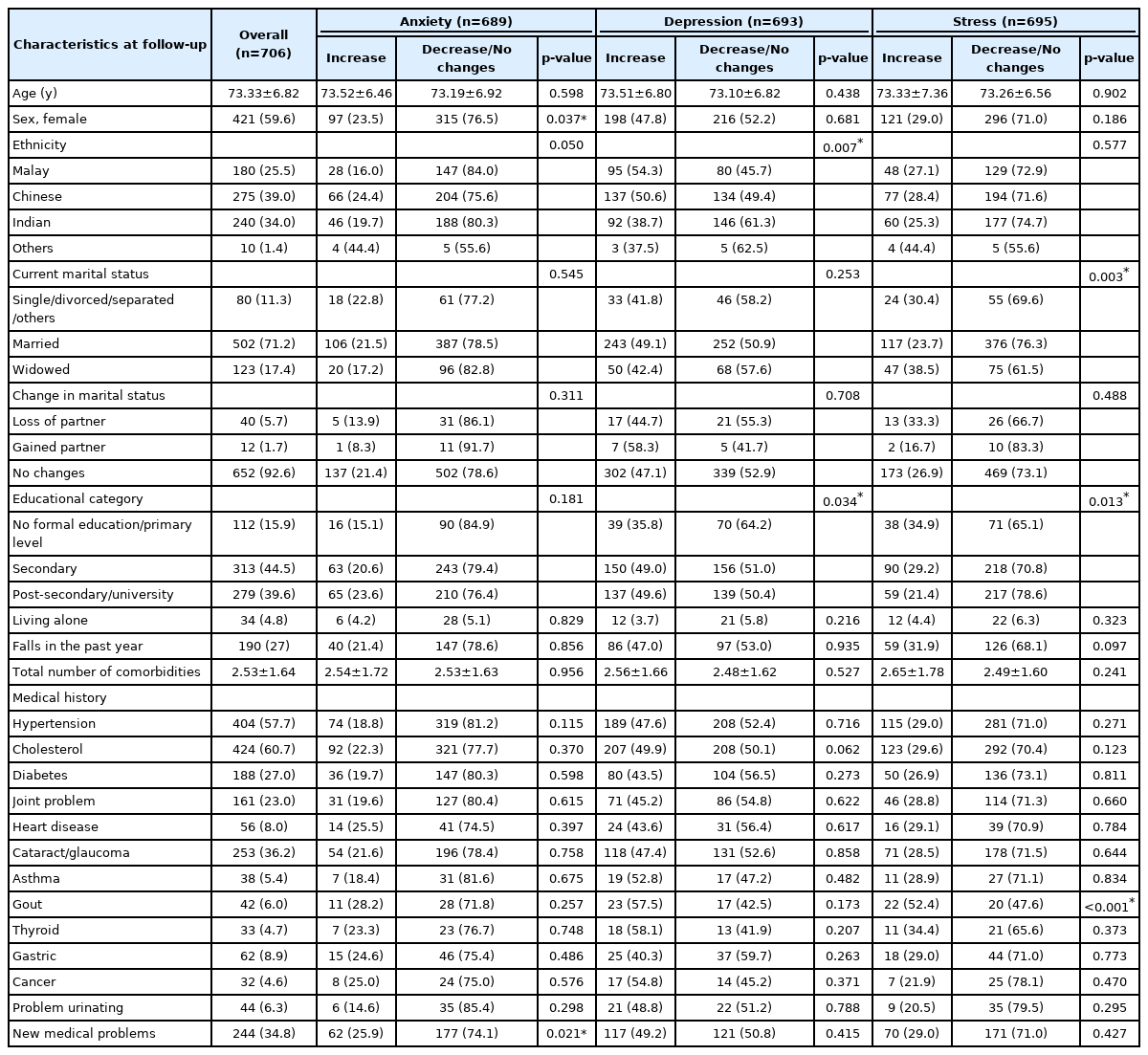
Follow-up data for the variables of interest were available for 750 participants from the original MELoR cohort. We observed increased anxiety scores in 144 (20.9%) participants, with 327 (47.2%) and 189 (27.2%) participants assigned to the increased depression and increased stress groups, respectively. Table 1 shows the comparisons among the groups with increased and no change or decreased anxiety, depression, and stress.
Changes in Psychological Status
At baseline, the mean±standard deviation scores for depression, anxiety, and stress measured using DASS-21 were 1.24±2.17, 3.53±4.03, and 2.15±2.82, respectively. The mean±standard deviation scores for depression, anxiety, and stress at follow-up measured using the GDS-15, DASS-anxiety and PSS-4 were 6.49±1.55, 1.93±3.21, and 2.98±2.89, respectively. The anxiety scores were significantly higher before the COVID-19 pandemic compared to those during the COVID-19 pandemic (p<0.001). No direct comparisons between depression and stress scores were possible due to the different scales used.
Changes in QoL
We observed no difference in total CASP-12 scores between baseline and Wave 4 follow-up (Table 2). A total of 304 (43.1%) participants showed reduced total CASP-12 scores. Four of the 12 items showed improvements in individual item scores, three of which were reverse scored items, with participants reporting that they felt “out of control,” “left out of things,” and “short of money” less often, and able to “please themselves in what they did” more often. We observed deteriorations in scores in two items, with participants less often indicating that they felt “life was full of opportunities” and “full of energy.” The total control/autonomy domain scores were higher at follow-up compared to those at baseline while the total self-realization/pleasure domain scores were lower at follow-up compared to those at baseline.
Influence of Psychological Status on Changes in QoL
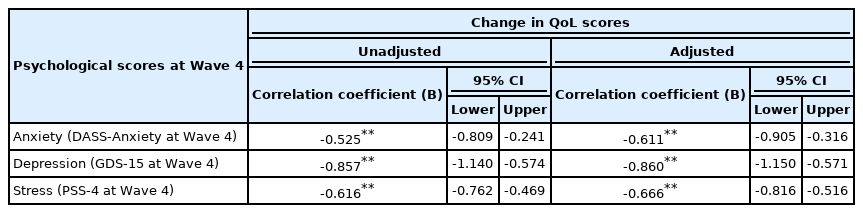
Tables 3 and 4 summarize the results of the linear regression analyses of changes in CASP-12 scores from baseline to the Wave 4 follow-up as the dependent variable.
Psychological Scores at Follow-up
We included the total anxiety, depression, and stress measured during the Wave 4 follow-up using the DASS-Anxiety, GDS-15, and PSS-4 as independent variables in separate models. Within the unadjusted models, total anxiety, depression, and stress scores at the Wave 4 follow-up were significantly negatively correlated with changes in QoL scores, with correlation coefficients of -0.525, -0.857, and -0.617, respectively, indicating strong negative correlations. The anxiety, depression, and stress levels at follow-up remained significantly negatively correlated with changes in QoL scores after adjusting for the potential confounders of age, gender, marital status, ethnicity, educational level, and presence of new medical condition (Table 3).
Increased Anxiety, Depression, and Stress
The presence of increased anxiety, depression, and stress was associated with significantly reduced QoL scores in the unadjusted linear regression models. The negative association between changes in QoL scores with increased anxiety, depression, and stress remained significant following adjustment for age, gender, ethnicity, marital status, educational level, and presence of a new medical problem. The CASP-12 scores in individuals with increased anxiety, depression, and stress were 2.6, 2.9, and 4.0 points lower, with a maximal attainable CASP-12 score of 36 (Table 4).
DISCUSSION
Individuals who experienced increased anxiety, depression, and stress during the COVID-19 pandemic compared to the baseline values at recruitment showed significant reductions in total QoL scores measured using the CASP-12. We observed a significant reduction in total anxiety scores and no change in QoL scores during the COVID-19 pandemic compared to baseline data collected from 2013 to 2015. Considering the lack of longitudinal data on older adults’ QoL and psychological status, the results of this study provide important novel information on the impact of COVID-19 on the lives of older adults in a multiracial middle-income developing nation.
Previous studies have shown that older adults faced a general lack of social activity leading to little social support during the COVID-19 pandemic.22-24) However, in our study, anxiety levels were lower during the COVID-19 pandemic compared to those before the pandemic. This suggests a different societal structure in terms of greater reliance on family members for social support rather than community or friends.25) Hence, a loss of social activity in our community did not negatively influence the mental health of older people, which may also imply low social activity among our older adults even before the pandemic.
Social isolation and restrictions enforced to try to curb the spread of COVID-19 are expected to lead to major changes in the QoL of older adults. However, amidst these challenging times, the older adults in our study felt less out of control, less left out, and less short of money but were more likely to feel that they lacked energy and that life lacked opportunities compared to 6–8 years ago. This reflected a potential lack of optimism for the future but a refreshing level of resilience. Unlike developed countries, where 20% to 27% of older adults live alone,26) only 4.8% of our cohort lived alone. Hence, when lockdown measures were in place, adult children and other family members were more likely to be at home. Thus, society currently holds to filial piety values, which are considered core for Asian culture.27) In times of crisis, communities ensure what the older adult population is provided for. Indeed, older adults were prioritized for vaccinations and admission to the hospital during the COVID-19 pandemic.28) Furthermore, days were more predictable; therefore, older adults felt more in control and were able to manage their spending.
The social determination theory corroborates that motivation are driven by human being’s basic psychological need for autonomy, competence, and relatedness.29) Our study’s population scored better in the domains of control and autonomy during the pandemic. Despite restrictions, older adults experienced elements of control and autonomy within their households as Asian older adults maintain significant decision-making powers and head of household stature, especially those living within multi-generational households. Lower scores in the self-realization and pleasure domains may be due to a lack of exposure to leisure, entertainment, and social contact with their peers. Furthermore, demotivation is expected and a natural process of any prolonged crisis, which over time forces individuals to adopt various coping mechanisms.30,31)
Overall, our older adults reported being more pleased with what they did during the COVID-19 pandemic. Similarly, Bidzan-Bluma et al.10) reported that older Polish and German adults were more content with life compared to younger adults during the COVID-19 pandemic. The participants in the present study were born and raised amidst the Japanese occupation and communist insurgency in Malaysia (then known as Malaya) from 1941 to 1960. Therefore, adhering to curfews and strict restrictive measures were not new to them. The lessons learned based on their experience from past life events may also have inculcated resilience among them to undergo dire situations like the pandemic. Furthermore, the attributes of later-life resilience include the ability to experience positive phenomena during a crisis, as observed among participants in this study.32,33)
Studies conducted among Asian populations before the COVID-19 pandemic reported the impacts of depressive, anxiety, and stress symptoms on health-related QoL.34,35) The results of the present study indicated that the anxiety, depression, and stress levels as well as the presence of increased anxiety, depression, and stress had negative effects on the QoL of older individuals. There is a general expectation that the QoL in older adults, particularly those in developing countries, is influenced by access to healthcare, the availability of necessities such as food and clothing, and economic status. However, the adverse effects of psychological symptoms such as anxiety could have led to physical manifestations, resulting in an inability to continue with activities of daily living.5) QoL remains foreign in terms of importance among the Malaysian population. While numerous studies have explored QoL across different populations in Malaysia, there remains a general lack of emphasis on QoL within Malaysian households. The link between individual psychological status and QoL observed within this study calls for urgent attention to both mental health and maintaining QoL among older adults, with and without the presence of a pandemic.
The COVID-19 pandemic required the administration of virtual surveys for data collection.13) Thus, the data obtained could favor older adults with access to telecommunication and smart devices, possibly representing a more educated group. This may have led to a survival advantage, as reflected by the improved anxiety scores and comparable QoL scores before and during the pandemic. As the AGELESS study subsumes three existing cohorts, compromises occurred in the harmonization of the dataset, therefore limiting our ability to make direct comparisons among depression and stress scores. Few studies have explored the relationship between psychological status and QoL using the CASP-12, as psychological status and QoL are often measured concurrently.36) The strong correlation between QoL and psychological scores may be due to overlaps between the aspects measured by these scales rather than a true influence of psychological status on QoL. Regardless, we have demonstrated the strong impact of current and changes in psychological status on QoL among older adults. These findings may drive the development of policies to address mental health in older adults during and after the pandemic. Future studies should also consider strategies to address mental health among older adults and the effect of interventions in mental health on overall QoL.
In conclusion, overall, the findings of this study revealed that older adults did not experience changes in QoL during the COVID-19 pandemic compared to measurements obtained before the pandemic. However, increased anxiety, depression, and stress negatively influenced QoL among older adults during the pandemic. Therefore, measures to mitigate the effect of the pandemic on the overall QoL of our older population should consider mental health interventions.
Notes
We are grateful for the invaluable contributions offered by all the authors as well as the participants and investigators involved in the MELoR and AGELESS study for their role in ensuring successful data collection and study progression.
Part of the findings was presented at the Malaysian Hybrid Conference on Healthy Ageing (MCHA) 2022 held at Bayview Hotel, Georgetown, Penang, Malaysia on March 15–17, 2022. Part of the findings was also presented at the eMalaysian Congress of Geriatric Medicine 2021 (eMCGM) incorporating the Asia Pacific Geriatric Conference 2021 on August 19–21, 2021.
CONFLICT OF INTEREST
The researchers claim no conflicts of interest.
FUNDING
The Transforming Cognitive Frailty to Later Life Self-sufficiency (AGELESS) study is funded by the Ministry of Higher Education Malaysia Long Term Research Grant Scheme (LRGS/1/2019/UM//1/1).
AUTHOR CONTRIBUTIONS
Conceptualization, KA, TAH, RI, NIS, KH, HM; Data curation, SM; Funding acquisition, MPT; Investigation, KA, SM; Methodology, KA, KM, MPT; Project administration, MPT; Supervision, KM, SM, MPT; Writing_original draft, KA; Writing_review & editing, KM, SM, TAH, RI, NIS, KH, HM, MPT.