Effect of Communication and Education within the Rehabilitation Team: Therapists’ and Nurses’ Views
Article information
Abstract
Background
To improve the rehabilitation team’s awareness of patient mobility and participation by enhancing communication between therapists and nurses and conducting patient education.
Methods
This study used a non-equivalent control group with a non-synchronized design. To facilitate communication between therapists and nurses, we used a manual for mobility management to improve the sharing of information on the functional status of patients. We also implemented patient education to improve their awareness of mobility and participation. Finally, we conducted newly devised surveys related to patient functional status and awareness that were applied by therapists and nurses.
Results
The nurses reported significantly lower functional levels of patients compared to those assessed by therapists. After the intervention, the kappa values representing the concordance between therapists and nurses improved to almost perfect agreement for transfer ability (κ=0.836), mobility (κ=0.664), and toileting (κ=1.000). We also observed a statistically significant increase in questionnaire scores with respect to nurses’ awareness (p<0.05).
Conclusion
Improving communication among the rehabilitation team, including nurses through the use of a continuous education program, was effective in promoting the mobility and functional level of patients in the inpatient ward.
INTRODUCTION
As modern society enters super-aging status, rehabilitation medical care is important to restore the independence of older adults and individuals with disabilities. In addition, as stated in the 2020–2030 Healthy Aging Decade, hospital culture should aim to be friendly to older adults and provide integrated care. In this context, multidisciplinary care centered on hospitalized older adults and individuals with disabilities is essential.1,2)
The goal of rehabilitation therapy is to improve the activities of daily living (ADL) and increase the participation of patients through functional recovery, which determines the time required for their return to daily life and their level of participation in the community.3,4) Among patients receiving rehabilitation therapy, the restoration of mobility and independence is essential for functional improvement.4,5) As limited time is available for receiving rehabilitation therapy in the gym and patients spend most of their time in the inpatient ward, patient mobility in the ward is also important.6) However, inappropriate hyperactivity that does not match the patient’s functional status can cause falls, which can lead to fractures, fear of walking, disability, increased hospital stays, and additional costs, thereby inhibiting more effective rehabilitation treatment.4,7) Therefore, to promote independence and prevent falls, individualized programs that consider patient function are needed to promote the mobility of patients in the ward.
However, unlike a therapist whose primary goal is to improve mobility and function, nurses in an inpatient rehabilitation ward tend to create dependency and immobility issues due to a lack of knowledge and experience regarding rehabilitation to improve mobility.5,8-11) Thus, patient mobility and participation levels differ between the gym and the ward. The insufficient education of nurses regarding rehabilitation leads to their lack of knowledge regarding the importance of rehabilitation for improving mobility. This prevents nurses from facilitating therapy continuation and integration, which play important roles in multidisciplinary rehabilitation team.12-15) In this context, the present study aimed to improve the mobility and participation of patients in an inpatient ward by enhancing communication between therapists and nurses and implementing an educational program.
MATERIALS AND METHODS
Study Design and Participants
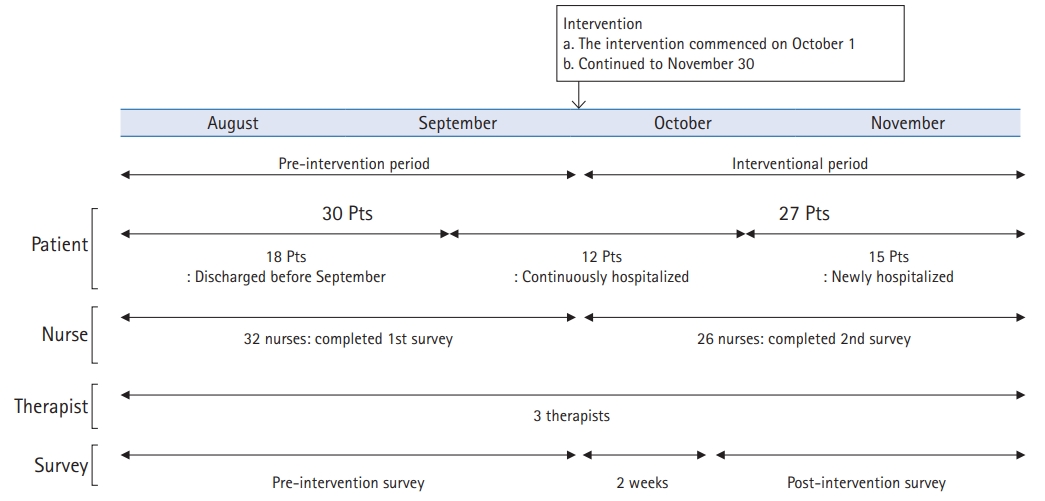
This study was performed between August and November 2019 at the rehabilitation unit of a community-based hospital in Korea. The participants comprised 45 patients admitted to the rehabilitation department, three therapists in charge, and 32 nurses dedicated to the inpatient rehabilitation ward. This study included all admitted patients receiving rehabilitation therapy, regardless of the diagnosis. The pre-intervention group included 30 patients hospitalized before the intervention period who participated in the survey without intervention, while the intervention group included 27 patients who participated in the survey after the intervention. The intervention group also included 12 patients in the pre-intervention group who were continuously hospitalized during the intervention period. We excluded patients who could not answer the survey questions or who did not agree to participate. We conducted the pre-intervention survey between August 1 and September 30, 2019. The intervention commenced on October 1, 2019 and we conducted the post-intervention survey after 2 weeks (Fig. 1). The surveys were administered on paper, and patients who were unable to complete the questionnaire due to cognitive problems were assisted by a caregiver. The nurses enrolled in this study were not familiar with rehabilitation to improve mobility because they had not received detailed rehabilitation education. Three therapists had extensive experience in rehabilitation for mobility. This study was approved by the Institutional Review Board of Seoul National University Bundang Hospital (No. B-2102-664-116).
Interventions
We conducted two kinds of interventions: efficient communication among rehabilitation staff and promoting awareness of mobility and functional status among nurses and patients (Fig. 2). To do so, the research team produced a manual called “My Rehabilitation Story.” This manual contained useful information about using devices for mobility, such as wheelchairs and walkers, and skills for improving transfer, walking, and toileting. In particular, it contained information about the functional status according to individual patient evaluation. It describes the functional level, such as rolling, sitting up, transitioning from sitting to standing, sitting balance, standing balance, transfer, and performing ADL. The functional level was categorized into four levels according to the degree of help required (independent, supervision, help, and impossible) and recorded, which allowed clear communication of the patient’s functional level by sharing the manual.

The study was designed to enable efficient communication between physicians, therapists, and nurses and improve activity-related education. We used an activity manual called “My Rehabilitation Story.” ADL, activities of daily living; PT, physical therapy.
First, the manual was used as a tool for communication between nurses and therapists to share information about each patient’s functional status. The patients’ safe mobility, transfer ability, and toileting level based on the results of the functional evaluation were marked by the therapists on the lists of activities in the manual, which was then delivered to the nurses in the ward as a form of communication. The manuals were kept in the ward to continuously monitor each patient’s level of activity and provide feedback to the patients, with all nurses checking the patient if necessary. In addition, to maximize communication, the rehabilitation team held a 30-minute team meeting once weekly. Second, the manual was used for patient education by therapists and nurses. At the same time, the nurses could also use the manual for self-directed learning.
Survey Methodology
This study applied two survey questionnaires devised by the research team. The first questionnaire was related to the patients’ functional status and was administered by the therapists and nurses after the initial functional assessment. The purpose of this survey was to determine the differences in each patient’s functional level, as assessed by therapists and nurses. The survey consisted of multiple-choice questions about transfer ability (Question 1), mobility (Question 2), and toileting (Question 3). The respondents were asked to choose the answer that best suited the patient’s functional level (Supplementary Table S1). Through these questions, we analyzed the agreement on the functional status of each patient between therapists and nurses before and after the intervention.
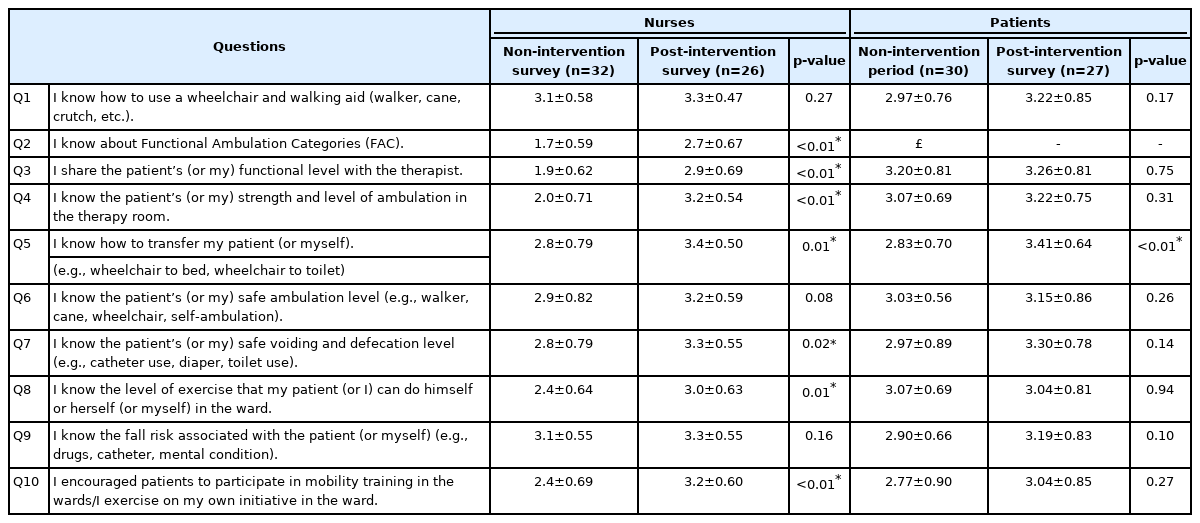
The second questionnaire was related to the awareness of mobility management. We applied this survey to nurses and patients before and after the intervention and assessed their overall understanding of mobility (Questions 1–2), understanding of patient mobility and function (Questions 3–9), and activity recommendation performance (Question 10). The nurses’ questionnaire consisted of 10 questions, while the patients’ questionnaire consisted of nine questions, as it excluded the question on functional ambulation categories (Question 2). We used a 4-point Likert scale to analyze and interpret the results of the survey (Table 1).
Statistical Analysis
Frequency analysis was performed using descriptive statistics to analyze the general characteristics of the participants. χ2 and Fisher exact tests were used to identify differences in participant characteristics between the two time points. Concordance between the therapists and nurses at the functional level was determined using Cohen’s kappa (κ). Response options 1 and 2 were combined into one category, “totally dependent,” whereas 3–6 were combined into the category “partially dependent or independent.” Agreement was defined as poor (<0.20), fair (0.21–0.40), moderate (0.41–0.60), good (0.61–0.80), or excellent (0.81–1).16) The analysis of the nurses’ and patients’ questionnaires used an ordinal 4-point Likert-type scale with possible responses of “fully disagree,” “partly disagree,” “partly agree,” and “fully agree.” Wilcoxon signed-rank tests were used to evaluate the significance of the differences in the responses to these questions. All analyses were performed using SPSS Statistics for Windows, version 22.0 (IBM SPSS, Armonk, NY, USA). In all analyses, statistical significance was set at p<0.05.
RESULTS
Patient Demographics
Table 2 summarizes the general demographic characteristics of the patients included in this study. The pre-intervention group included 13 men (43.3%) and 17 women (56.7%) with a mean age of 71.7±12.8 years, while the intervention group included 14 men (48.2%) and 13 women (48.2%) with a mean age of 67.2±14.0 years. The most common diagnosis was stroke in both groups—pre-intervention group, 17 patients (56.7%); intervention group, 15 patients (55.6%). In the pre-intervention group, the Functional Ambulation Category score was 2.54±1.50, the modified Barthel Index score was 54.95±24.25, the Mini-Mental State Examination-Dementia Screening score was 20.33±7.58, and the Global Deterioration Scale score was 3.44±1.54. In the intervention group, these scores were 2.44±1.72, 57.94±24.23, 20.46±7.04, and 3.54±1.45, respectively. We observed no significant differences in the characteristics or scores between the two groups (p>0.05).
Agreements on Patient Functional Levels between Therapists and Nurses
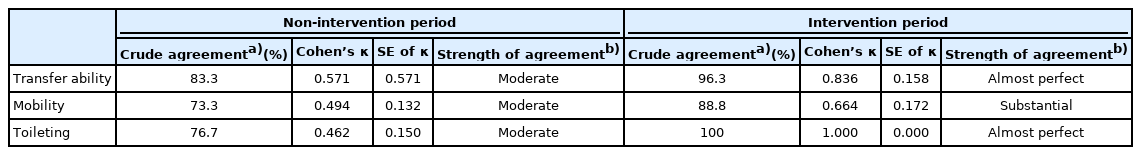
We analyzed the views of the therapists and nurses on each patient’s functional level. We compared the proportions of patients that therapists and nurses classified as immobile or totally dependent. Regarding transfer ability, nurses and therapists classified 33.3% and 16.7% of patients, respectively, as totally dependent. This difference decreased from 16.6% to 3.7% after the intervention (Fig. 3). Regarding mobility, nurses and therapists classified 53.3% and 30% of patients, respectively, as immobile. This difference of 23.3% (p=0.037) decreased to 11.1% (p=0.311) after the intervention. Regarding toileting, nurses and therapists classified 40% and 16.7% of patients, respectively, as totally dependent, with a difference of 23.3% (p=0.045). However, there was no difference between the two groups after the intervention (p=1.000) (Fig. 3). The inter-rater agreement (κ) rates between therapists and nurses on patient functional level was moderate before the intervention as follows: transfer ability, κ=0.571 (p<0.01); mobility, κ=0.494 (p<0.01); and toileting, κ=0.462 (p<0.01). However, the rates improved substantially to almost perfect agreement after the intervention as follows: transfer ability, κ=0.836 (p<0.01); mobility, κ=0.664 (p<0.01); and toileting, κ=1.000 (p<0.01) (Table 3, Fig. 4).
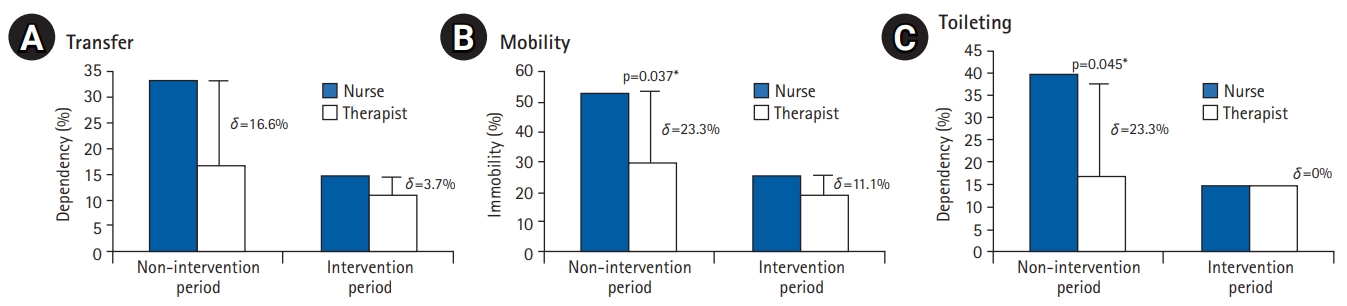
The proportion of patients determined to be immobile or totally dependent for activities of daily living by nurses and therapists. For all questions, the difference between nurses and therapists was reduced after the intervention, with decreases of 16.6% to 3.7%, 23.3% to 11.1%, and 23.3% to 0% observed for questions related to (A) transfer ability, (B) mobility, and (C) toileting, respectively. *p<0.05.
Descriptive statistics, Cohen’s kappa coefficient (κ), and measures of the strength of agreement for each item
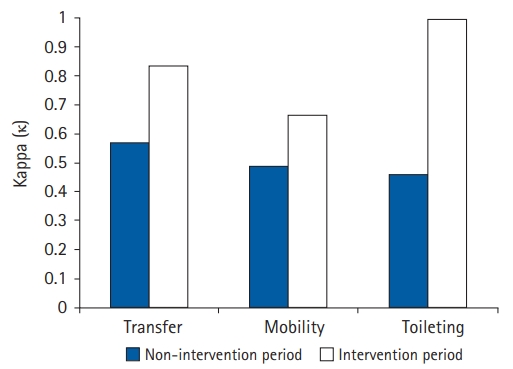
The inter-rater agreement (κ) between therapists and nurses regarding patient functional level. Moderate agreement was observed before the intervention, with agreement values of κ=0.571, κ=0.494, and κ=0.462 for questions related to transfer ability, mobility, and toileting, respectively. Agreement levels improved substantially to almost 100% after the intervention, with agreement values of κ=0.836, κ=0.664, and κ=1.000, respectively.
Results of Surveys Assessing Awareness of Nurses about Mobility Management
Analysis of the survey of nurses showed increased mean scores for all questions after the intervention. The score increases were significant (p<0.05) for all questions except for those on the use of aids (Question 1), identifying patient mobility level (Question 6), and fall risk assessment (Question 9). The three items that did not exhibit significantly different scores post-intervention had higher scores in the pre-intervention survey than the other items. The rate of disagreement in responses decreased from 42.5% before the intervention to 10.4% after the intervention (Table 1).
Results of Surveys Assessing Patient Awareness of Mobility Management
As with the results of the survey for nurses, the intervention group had higher average scores for all items. However, we observed no significant differences between the non-intervention and intervention groups, except for the question about transfer ability (Question 5, p<0.01) (Table 1). In addition, we compared the results of the surveys for nurses and patients conducted during the non-intervention period, as the questionnaire included the same questions except for Question 2. The mean score of the patient group was higher for all questions except for those about the use of aids (Question 1) and fall risk assessment (Question 9).
DISCUSSION
This study was conducted to improve the rehabilitation team’s awareness of patient mobility and participation by enhancing communication between therapists and nurses and conducting patient education. Our intervention yielded several findings. First, after the intervention, the nurses showed significant improvements in their awareness of patient mobility and safety. The survey conducted before the intervention indicated that the nurses lacked awareness of patient fall risk, mobility, and functional levels. However, these improved within a short time through communication and educational sessions. These results supported those of previous reports suggesting that a lack of awareness prevents nurses from promoting patient mobility.5,17,18) Our observations also underscored the need to emphasize patient mobility and functional levels in education programs for nurses.
Second, the different perceptions of patient functional levels between therapists and nurses confirmed the need for communication within the rehabilitation team.19) We observed moderate agreement between therapists and nurses before the intervention (κ=0.41–0.60). In particular, compared to therapists, nurses had a greater tendency to limit active participation in daily activities. A previous study reported differences in the perceptions of roles between nurses and therapists. According to Dalley and Sim,12) nurses tended to limit therapists’ roles in facilitating mobility and functioning. They also tended to consider therapists as having distinct and different roles in the rehabilitation team.12) Doherty et al.20) also reported that it was difficult for nurses to set an acceptable patient functional level. In contrast, Long et al.13) emphasized coordination and communication among nurses’ roles in a multi-professional rehabilitation team. They reported that nurses play a role in integrating rehabilitation care through ongoing communication with therapists.
The manual developed by our team, “My Rehabilitation Story,” improved the sharing of information related to the patient’s functional level. This written medium allowed both formal and informal communication, which helped to set appropriate patient mobility participation levels in the ward. Previous studies have demonstrated the effectiveness of communication processes in multidisciplinary teams. Papadimitriou and Cott21) reported that interprofessional communication allowed effective team performance and enhanced client-centered practice. Tyson et al.22) also reported that the use of objective measurement tools was effective in avoiding communication conflicts in a multidisciplinary team approach. However, all previous studies were qualitative, with case report designs. Therefore, they were insufficient to clarify the effects of communication. However, it is meaningful to analyze the effect of communication based on an objective and quantitative index; namely, inter-rater agreement (κ). To our knowledge, this study is the first to report a quantitative analysis of the effect of communication between therapists and nurses in a rehabilitation setting.
Third, education on mobility and participation improved patient awareness. This finding was consistent with those of previous studies showing that patient education prevented immobility and improved functional status, independence, and mobility.23-26) However, despite the overall improvement, we observed no statistically significant improvements in any of the question scores, except for Question 5 (p<0.01). This might have been due to the high survey scores by the pre-intervention group. Interestingly, the patients had a greater awareness of their mobility than their nurses. This was because, even during the non-intervention period, therapists provided education on mobility as part of the patients’ rehabilitation program.
Patients participating in rehabilitation therapy experience more falls due to the promotion of mobility and participation.4,27) Moreover, if they experience a serious fall, patients tend to passively participate in ADL.28) In this study, the number of falls did not increase, even though we promoted mobility. Only one fall occurred during both the non-intervention (907 person-days) and intervention (958 person-days) periods. Therefore, the intervention conducted in this study was suitable for promoting mobility without increasing fall accidents. Previous studies have highlighted this as an important element of mobility promotion programs.29)
The contribution of nurses to rehabilitation for improving mobility is important for maximizing patient functional outcomes.30-32) Nurses who promote patient ADL participation while communicating with therapists can speed patient recovery and reduce rehabilitation time.13) Burton33) reported that nurses also wanted to help patients to use the skills in their ADL that they had learned from therapists in the gym. The improvement in communication between therapists and nurses with the continuous educational program proposed in this study is consistent with the ideal nursing practice for promoting patient mobility advocated by King et al.34)
This study had some limitations. We included only a single site and a small sample size, which could potentially limit the generalizability of our findings. In addition, this was not a randomized controlled trial, which might have led to bias. Finally, due to the lack of clinical outcomes to assess the effectiveness of interventions, further studies are needed to determine whether mobility facilitation in an inpatient ward can, in turn, facilitate functional improvement.
The results of this study confirmed that improving communication among healthcare professionals from multiple disciplines, including nurses and therapists, through continuous educational programs promoted patient mobility and ADL participation in the inpatient ward. Therefore, our findings provide evidence of the benefits of a ward culture that facilitates a team approach to promote and recommend appropriate mobility for patients.
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via https://doi.org/10.4235/agmr.21.0085.
Survey items were designed to assess the agreement in patient functional status between therapists and nurses and consisted of multiple-choice questions on participation in ADL
Notes
CONFLICT OF INTEREST
The researchers claim no conflicts of interest.
FUNDING
None.
AUTHOR CONTRIBUTION
Conceptualization, KJY, JJH, KJY, KCH; Data curation, JJH; Investigation, KJY, KCH; Methodology, JJH, KJY; Project administration, LJY; Supervision, KJY, LJY; Writing-original draft, JJH; Writing-review & editing, KJY, LJY.