Functional Constipation is Associated with a Decline in Word Recognition 2 Years Later in Community-Dwelling Older Adults: The Korean Frailty and Aging Cohort Study
Article information
Abstract
Background
Consumption and cognitive impairment are the most common health problems among older adults. This study aimed to determine the effects of functional constipation on cognitive decline in community-dwelling older adults.
Methods
This was a 2-year longitudinal analysis of Korean Frailty and Aging Cohort Study data, including 851 community-dwelling residents who participated in both the baseline and follow-up surveys. A neuropsychological test, the Consortium to Establish a Registry for Alzheimer's Disease Assessment Battery (CERAD-K), and the Korean version of the Frontal Assessment Battery (FAB) were used to evaluate cognitive function. Functional constipation was defined according to the ROME IV criteria. An analysis of covariance was used to identify the association between functional constipation and cognitive decline.
Results
Among the 851 participants, 8.9% had functional constipation. The patients in the constipation group were more likely to have low physical activity (15.8% vs. 8.8%), polypharmacy (61.8% vs. 45.5%), and depression (30.3% vs. 17.4%) than the non-constipation group. After adjusting for potential confounding factors, including age, sex, education years, low physical activity, polypharmacy, type 2 diabetes mellitus, depression, and baseline Cognitive Function Test score, the mean changes in Word Recognition test scores from 2018 to 2020 were -0.07 and -0.54 in the non-constipation and constipation groups, respectively (p=0.007). Other cognitive function tests (Mini-Mental State Examination, word list memory, word list recall, digit span, trail-making test, and FAB) did not show any difference in decline between the two groups (p>0.05).
Conclusions
Functional constipation at baseline was associated with a decline in word recognition after 2 years.
INTRODUCTION
Constipation is an unsatisfactory defecation disorder characterized by infrequent stools, difficult stool passage, or both, and it is one of the most common health problems encountered in older adults.1-3) Functional constipation was defined by the Rome Foundation to help standardize the diagnosis of chronic constipation without physiological abnormalities identified by routine diagnostic examinations, as deemed clinically appropriate.4) The worldwide prevalence of functional constipation in adults is 10.1%,5) and the prevalence of functional constipation increases with age. Functional constipation has been reported in 30%–40% of older adults worldwide6) and 19.6% of Korean adults aged 72–86 years.7)
Cognitive impairment is a major personal and public health problem in older adults. Therefore, identifying the risk factors for cognitive impairment is essential for preventing cognitive disorders and can help promote successful cognitive aging.8)
As an important manifestation of autonomic nerve dysfunction, constipation is well known to be the most common non-motor complication of Parkinson disease. Santos García et al.9) found that constipation predicts cognitive decline in Parkinson disease. In a cross-sectional population-based cohort study, Wang et al.10) showed that a higher prevalence of constipation is associated with dementia and non-amnestic mild cognitive impairment. However, no prospective cohort study has yet explored the predictive effects of functional constipation on cognitive decline. Therefore, we investigated the relationship between functional constipation and cognitive decline in community-dwelling older adults using the Korean Frailty and Aging Cohort Study (KFACS) longitudinal database.
MATERIALS AND METHODS
Study Population
The KFACS is a nationwide multicenter longitudinal study with a baseline survey conducted in 2016 and 2017 to identify factors contributing to frailty and aging in community-dwelling individuals aged 70–84 years. The baseline survey for the cohort study was conducted at 10 centers, with 1,559 participants in 2016 and 1,455 in 2017.11) The participants were recruited from urban, suburban, and rural communities nationwide. To investigate the prevalence of frailty among the three age groups and consider the higher attrition rate in the oldest age group, the KFACS cohort adopted quota sampling stratified by age (70–74, 75–79, and 80–84 years, with a ratio of 6:5:4). This quota sampling is based on oversampling of the older group using population distribution data from the Korean Population and Housing Census conducted by Statistics Korea in 2015 (distributions of 43.5%, 33.8%, and 22.7% for adults aged 70–74, 75–79, and 80–84 years, respectively).12) Participants were recruited from diverse settings (local senior welfare centers, community health centers, apartments, housing complexes, and outpatient clinics) to minimize selection bias. All participants were ambulatory, with or without the use of walking aids. Follow-ups have been conducted at 2-year intervals. A questionnaire to evaluate functional constipation was included in a follow-up survey in 2018. Of the 1,292 participants aged 72–86 years who participated in the follow-up survey in 2018, 1,273 revisited the center after 2 years for the second follow-up survey in 2020.
Of the 1,273 participants, those without available prescription information (n=356) and those who were diagnosed with dementia or cerebrovascular disease (n=66) were excluded, and 851 subjects were enrolled in the analysis (Fig. 1).
The KFACS protocol was approved by the Institutional Review Board of the Clinical Research Ethics Committee of Kyung Hee University Medical Center (IRB No. 2015-12-103), and all participants provided written informed consent. Data anonymization was performed to protect participants’ privacy. This study was conducted in accordance with the consensus ethical principles derived from the Declaration of Helsinki.
This study complied the ethical guidelines for authorship and publishing in the Annals of Geriatric Medicine and Research.13)
Assessment of Functional Constipation
Functional constipation is a functional bowel disorder that presents with obvious low-frequency or incomplete defecation.4) Functional constipation was assessed based on the Rome IV criteria for functional constipation.
(1) Must include two or more of the following:
- Straining during more than one-fourth (25%) of defecations.
- Lumpy or hard stools (Bristol stool scale 1–2) in more than one-fourth (25%) of defecations.
- Sensation of incomplete evacuation in more than one-fourth (25%) of defecations.
- Sensation of anorectal obstruction or blockage in more than one-fourth (25%) of defecations.
- Manual maneuvers to facilitate more than one-fourth (25%) of defecation.
- Fewer than three spontaneous bowel movements per week.
(2) Loose stools are rarely present without the use of laxatives.
(3) Insufficient criteria for irritable bowel syndrome.
In addition, those who had experienced an onset of symptoms more than 6 months prior were included for functional constipation according to the ROME IV criteria.
Assessment of Cognitive Function
A neuropsychological test, the Consortium to Establish a Registry for Alzheimer's Disease Assessment Battery (CERAD-K), and the Korean version of the Frontal Assessment Battery (FAB) were used to evaluate comprehensive cognitive function. The CERAD-K is a standardized clinical and neuropsychological assessment battery for evaluating patients with Alzheimer’s.14) The CERAD-K initially consisted of eight tests—verbal fluency, modified Boston naming, Korean version of the Mini-Mental State Examination (MMSE-KC), word list memory, constructional praxis, word list recall, word list recognition, and constructional praxis recall; however, in this study, word list memory, word list recall, word list recognition, digit span (forward and backward), trail-making test (TMT) A, and MMSE-KC were included.14)
Word list memory is a test that assesses memory for new information learning. It is conducted by presenting 10 commonly used words at intervals of two seconds and reading the words aloud, followed by immediate recall of as many words as possible for 90 seconds. The maximum score was 30 points, with 10 points per session. The word list recall test evaluates the ability to recall the 10 words from the word list memory test. A maximum of 90 seconds was allowed, and the maximum score was 10. The word list recognition test measures recognition ability. The goal was to distinguish between the 10 words in the word list memory test and 10 new words. The maximum possible score was 10. TMT A assesses attention, ordering, executive function, time-space search, and mental motion velocity. Patients were asked to draw a line connecting numbers 1 to 25 in ascending order, and the time taken was recorded. Participants who did not complete this within 360 seconds were excluded. The digit span test assesses short-term memory, working memory, and attention by recalling the number sequence after hearing numbers forward and backward. Digit spans, forward and backward, were composed of seven digit questions and presented with two trials. One point was scored when each digit was correctly recalled, and the maximum score was 14 points for each digit span, forward and backward. The digit span total is the combined score of the forward and backward digit span.14)
The FAB assesses executive functions, such as planning, working memory, mental flexibility, and inhibition. It consists of similarities (conceptualization), lexical-verbal fluency (mental flexibility), motor series (programming), conflicting instructions (sensitivity to interference), Go–No Go (inhibitory control), and prehension behavior (environmental autonomy), with a maximum score of 18; higher scores indicate better frontal lobe function.15)
Other Measurements
Demographic information, including age, sex, independent living, marital status, years of education, medical aid, alcohol consumption, and smoking habits, was investigated through face-to-face interviews in 2018. Malnutrition was defined as a Mini Nutritional Assessment (MNA) score of <17.16) Physical activity was assessed using the metabolic equivalent of task minutes per week and kcal per week, calculated using the International Physical Activity Questionnaire.11) Polypharmacy implies the use of five or more prescribed medications. The Geriatric Depression Scale (GDS) short form was used to define depression, and scores >5 indicate depression. History of chronic diseases, including hypertension, type 2 diabetes mellitus, dyslipidemia, depressive disorder, dementia, cerebrovascular disease, other psychiatric disorders, renal disorders, thyroid disorders, and malignancies, was assessed in 2018 for analysis.
Statistical Analyses
Data are presented as mean±standard deviation or percentages. Continuous variables were compared using the independent t-test, and categorical variables were compared using the chi-squared test. Univariate regression analysis was used to identify associations between each characteristic and decline in word list recognition over 2 years. Analysis of covariance (ANCOVA) was used to identify associations between functional constipation and cognitive decline, adjusted for age, sex, years of education, low physical activity, polypharmacy, type 2 diabetes mellitus, depression, and baseline cognitive function test scores. All statistical analyses were performed using IBM SPSS Statistics for Windows, version 25 (IBM Corp., Armonk, NY, USA). The level of statistical significance was set at p<0.05.
RESULTS
General Characteristics of the Study Population
The baseline characteristics of the participants are presented in Table 1. Among the 851 participants, 8.9% (n=76) had functional constipation. The mean age of the functional constipation group (78.6±3.9 years) was higher than that of the non-constipation group (77.5±3.8 years). The functional constipation group was more likely to have a higher rate of low physical activity (15.8% vs. 8.8%), polypharmacy (61.8% vs. 45.5%), and depression (30.3% vs. 17.4%) at baseline than the non-constipation group.
The characteristics of the participants 2 years after baseline are shown in Supplementary Table S1. Depression prevalence 2 years after baseline was 149 (19.2%) in the non-constipation group and 24 (31.6%) in the constipation group (p=0.011). There was no statistically significant difference between the two groups in changes in depression over 2 years (p=0.674). (Supplementary Table S2).
Changes in Cognitive Functions over 2 Years according to Constipation at Baseline
Changes in word list recognition over 2 years in the functional constipation group (-0.55±0.23) were much higher than those in the non-constipation group (-0.07±0.05). No statistically significant differences were found in the other cognitive function tests (MMSE, word list memory, word list recall, digit span, FAB, and TMT) between the constipation and non-constipation groups (Table 2).
Univariate Regression Analysis of Characteristics for the Change in Word List Recognition over 2 Years
Table 3 shows the results of the univariate regression analysis of each baseline characteristic for the change in word list recognition test scores over 2 years. Age was only significantly associated with changes in word list recognition (p<0.05).
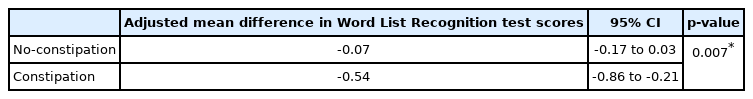
Adjusted Mean Changes in Word Recognition
As shown in Table 4, we evaluated the association between functional constipation and decline in word recognition test scores over 2 years after controlling for confounders using the ANCOVA test. The confounding variables were selected from the statistically significant variables (age, low physical activity, polypharmacy, and depression) for functional constipation (Table 1) and decline in word list recognition test scores in univariate regression analysis (Table 3), and variables (sex, years of education, type 2 diabetes mellitus, and polypharmacy) already known to be related to functional constipation and declines in cognitive function.17-19) The baseline measures of each cognitive function test in 2018 were also included as confounding variables.
In the ANCOVA, the word list recognition test scores declined more significantly in the constipation group (-0.53) than in the non-constipation group (-0.07) after adjusting for confounding factors (p=0.008).
DISCUSSION
Our study showed that functional constipation predicted a decline in word list recognition in community-dwelling older adults.
The proposed mechanism of the effect of constipation on cognitive decline is that constipation can indirectly affect cognitive status through irritability and aggression as well as pain and discomfort.20) Although antipsychotics may cause constipation and aggravate cognitive decline,21) participants in this cohort study were not affected by dementia or psychosis. The brain-gut axis hypothesis may be another mechanism. According to the brain-gut axis theory, the gut is connected to the brain through the gut-brain axis22); that is, the central nervous system communicates with the enteric nervous system, intestinal mucosa, and muscle layer through two-sided (afferent and efferent) pathways. Pathological changes in any component of the gut-brain axis may affect intestinal activity and lead to constipation. Some pathological studies have demonstrated that α-synuclein deposits can originate from the intestinal plexus and develop along the vagus nerve, eventually reaching the brain and resulting in the development of dementia.23) The last assumption is the dysfunction of the parietal lobe of the brain. The parietal lobe is suggested to be associated with constipation in children24) and is known to be related to short-term memory25) and recognition function.26) Therefore, parietal lobe dysfunction may be associated with constipation and its recognition. However, there are no studies on this connection yet; therefore, further investigation is needed. The initial and most prominent cognitive deficits associated with aging are usually amnestic rather than non-amnestic, and the finding that constipation is associated with a decline in word list recognition seems reasonable.
This study had some limitations. First, our study participants were ambulatory community-dwelling older adults. Hospitalized, institutionalized, or bedridden older adults were excluded; therefore, our results may not be generalizable to other population settings. Second, the detailed medication history of the participants was not investigated in this study. Medications such as antipsychotics can be associated with both constipation and cognitive impairment. However, we excluded those who had been taking narcotics and those with a history of dementia. In addition, the prevalence of psychiatric disorders did not differ between the two groups at baseline. Third, there is a possibility that organic constipation, such as colorectal cancer, was included because colonoscopy results were not collected in our study. However, those who had cancer within 5 years before baseline were excluded; therefore, the possibility of colorectal cancer was low.
Nevertheless, this study has several strengths. First, our study is based on a 2-year longitudinal prospective cohort-based study, which allows a more appropriate temporal relationship than previous cross-sectional studies. To the best of our knowledge, this is the first longitudinal study to show an association between functional constipation and cognitive function decline. Second, we used the KFACS data, which included a relatively large number of community-dwelling older adults aged 72–86 from 10 nationwide centers, including urban and rural areas.
In conclusion, functional constipation at baseline was associated with a decline in word list recognition 2 years later.
Notes
CONFLICT OF INTEREST
The researchers claim no conflicts of interest.
FUNDING
This study was funded by the Ministry of Health and Welfare, Republic of Korea (No. HI15C3153). This study was supported by a grant from the Korea Health Technology R&D Project through the Korean Health Industry Development Institute (KHIDI).
AUTHOR CONTRIBUTIONS
Conceptualization, CWW, SK; Data curation, HSJ, SK; Funding acquisition, CWW; Investigation, CWW, SK; Methodology, CWW, SK, HSJ; Writing-original draft, HSJ, SK; Writing-review and editing, all.
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via https://doi.org/10.4235/agmr.22.0092.
Characteristics of study subjects after 2 years according to functional constipation at baseline
Two-year change in depression between the constipation and no-constipation groups