World Health Organization Integrated Care for Older People (ICOPE) and the Integrated Care of Older Patients with Frailty in Primary Care (ICOOP_Frail) Study in Korea
Article information
Abstract
The World Health Organization (WHO) recently endorsed the proposal for a Decade of Healthy Ageing (2020–2030). The WHO defines “healthy aging” as “the process of developing and maintaining the functional ability that enables wellbeing in older age.” Among the strategies for the Decade of Healthy Ageing, the WHO has suggested enhancing intrinsic capacity, promoting functional ability, and implementing the Integrated Care for Older People (ICOPE) package. The WHO has defined steps for ICOPE evaluation and scale-up and is performing a prospective study in 2–3 countries (low and middle income, high income) to test its feasibility in 2021–2022 and a multinational randomized study to validate its clinical efficacy and effectiveness in 2022–2024. Intrinsic capacity and frailty represent two faces of the same coin, with one indicating the reserves of the individual and the other indicating the deficits that accumulate with age. The Integrated Care of Older Patients with Frailty in Primary Care (ICOOP_Frail) study is the first integrated care program for frailty or functional decline in primary care in Korea. The results suggest that the ICOOP_Frail study can be utilized as a reference for ICOPE studies in Korea or at least to provide important findings for the forthcoming ICOPE implementation study in Korea.
INTRODUCTION
On August 3, 2020, the World Health Assembly of the World Health Organization (WHO) endorsed the proposal for a Decade of Healthy Ageing (2020–2030). Thereafter, the proposal was submitted to the United Nations General Assembly, which proclaimed 2021–2030 as the United Nations (UN) Decade of Healthy Ageing on December 14, 2020.1) Following the UN decision, governments, international and regional organizations, civil society, the private sector, academia, and the media have been encouraged to actively support the Decade’s goals.1)
The WHO defines “healthy aging” as “the process of developing and maintaining the functional ability that enables wellbeing in older age.” Functional ability is the capability of people to do what they have reason to value. Being free of disease is not a requirement for healthy aging as many older adults have one or more health conditions that, when well-controlled, have little influence on their functional abilities.1) By its definition, functional ability includes a person’s capacity to:1) meet his or her basic needs; learn, grow, and make decisions; be mobile; build and maintain relationships; and contribute to society. Therefore, “functional ability” depends on the intrinsic capacity (IC) of the individual, relevant environmental characteristics, and the interaction between them.1)
The concept of IC was first introduced by the WHO in 2015 to create a multidimensional indicator related to an individual’s functional status, the follow-up of which over time may be useful to achieve healthy aging.2) IC comprises all the mental and physical capacities upon which a person relies and includes their ability to walk, think, see, hear, remember, etc. In addition, several factors, including diseases, injuries, and age-related changes, may influence the level of IC. The environment includes the home, community, and broader society and all the factors within them, such as the facilities, people and their relationships, attitudes and values of society members, health and social policies of the government, and the systems and services that support them.1)
As one of the strategies to implement the Decade of Healthy Ageing by enhancing IC, promoting functional ability, and minimizing care dependency, the WHO provided the Integrated Care for Older People (ICOPE) package in 2017. Evidence-based programs help key stakeholders in health and social care to understand, design, and implement a person-centered and coordinated model of care. The ICOPE program offers evidence-based tools and guidance specific to every level of care to maximize the IC and functional ability of older people.
Another concept associated with reduced IC is frailty. Frailty is related to functional deficits, and IC refers to functional reserve. Therefore, efforts to diagnose and manage frailty may help assess and prevent declines in IC. The authors recently started a randomized controlled trial of the Integrated Care of Older Patients with Frailty in Primary Care (ICOOP_Frail) to identify how the ICOOP_Frail could contribute to the WHO ICOPE by reviewing the associations between the two programs.
ICOPE GUIDELINES PUBLISHED BY THE WHO
The current ICOPE guidelines are organized into three modules.3)
Module I: Declines in IC, including mobility loss, malnutrition (vitality), visual impairment, hearing loss, cognitive impairment, and depressive symptoms.
Module II: Geriatric syndromes associated with care dependency, including urinary incontinence and risk of falls.
Module III: Caregiver support that includes interventions to support caregiving and prevents caregiver strain.
These guidelines cover evidence-based interventions to manage common declines in capacity in older age, including mobility, nutrition or vitality, vision, hearing, cognition, and mood, as well as important geriatric syndromes of urinary incontinence and risk of falls. These conditions were selected because they are strong independent predictors of mortality and care dependency in older age.4)
The general care pathways for those functional declines comprise the following five steps.3)
Step 1: Screen for declines in IC.
Step 2: Undertake a person-centered assessment in primary care.
Step 3: Define the goal of care and develop a personalized care plan.
Step 4: Ensure a referral pathway and monitor the care plan with links to specialized geriatric care.
Step 5: Engage communities and support caregivers.
IC and frailty represent the two faces of the same coin, with one indicating the reserves of the individual and the other the deficits that accumulate with aging.2)
Although both frailty and IC are dynamic entities, frailty is mainly used in cross-sectional assessments, while IC is applied in longitudinal approaches. However, instead of the frailty phenotype, a frailty index can be used in longitudinal approaches. The frailty index is related to physical, psychological, cognitive, sensory, and social functional declines, and the index is used not only to identify frail persons but also those at risk of frailty.5)
In addition, the frailty index and IC are based on the assumption that aging individuals can be adequately assessed and managed only if comprehensively evaluated and followed in a novel healthcare model based on service integration and multidisciplinarity.2)
Therefore, the integrated care of older patients with frailty or risk of frailty using the frailty index is as important for achieving healthy aging as reducing frailty level is for promoting it.6)
ICOPE IMPLEMENTATION PILOT PROGRAMS WORLDWIDE
The first phase of the ICOPE implementation pilot program started in France, Andorra, China, India, Italy, Kenya, Mexico, Qatar, and Vietnam to assess its feasibility and acceptability.3) In France, the ICOPE pilot program (the INSPIRE ICOPE-CARE program) was implemented in clinical practice in the Occitania region to promote healthy aging and maintain the autonomy of seniors based on the use of digital medicine.7)
The target population is independent seniors aged 60 years and over. The six domains of IC are systematically monitored using pre-established tools proposed by the WHO, which have been adopted in digital form to allow remote and large-scale monitoring.
Step 1 (screening) of the INSPIRE ICOPE-CARE program is performed every 4–6 months by professionals or the seniors themselves. If a deterioration in one or more domains of IC is identified, an alert is generated by an algorithm, which allows rapid intervention by health professionals. The operational implementation of the INSPIRE ICOPE-CARE program in Occitania is performed by the Territorial Teams of Aging and Prevention of Dependency network, which comprises 2,200 professionals in the medical, medico-social, and social sectors. The program aims to screen and monitor 200,000 older people in the Occitania region within 3–5 years and promote preventive actions. The French Presidential Plan Grand Age has largely implemented the WHO ICOPE program in France based on the experiences of the INSPIRE ICOPE-CARE program in Occitania.7)
Step 2 (person-centered assessment) and Step 3 (personalized care plan) of the INSPIRE ICOPE-CARE program are conducted by a general practitioner or if possible by a nurse trained in geriatrics. Experienced trained nurses of the Gerontopole perform geriatric evaluations of older people in their homes or public spaces close to their homes. These nurses with the support of a hospital geriatrician propose personalized care plans for the older people evaluated. This plan is then sent to the general practitioner to ensure its implementation and follow-up.7)
The WHO ICOPE’s Ready-Set-Go approaches to test and learn from the feasibility and acceptability of pilot studies, as well as studies to evaluate clinical effectiveness and efficacy are planned to be completed by 2024 (Table 1). From 2025, ICOPE will be rolled out within primary healthcare settings in a wider range of countries.3)
THE ICOOP_FRAIL STUDY
Since June 2020, we have been conducting the ICOOP_Frail randomized controlled trial of the National Evidence-based Healthcare Collaborating Agency in Korea. The study is underway in four primary care clinics, and two more clinics have recently joined. Nurses and doctors at the clinics apply the Korean Frailty Index for Primary Care (KFI_PC) to evaluate the functional decline and frailty of older adult patients visiting the clinics.8) The KFI_PC consists of 54 items in the following 10 domains: (1) cognitive status, including delirium or dementia; (2) mood; (3) communication, including vision, hearing, and speech; (4) mobility; (5) balance; (6) bowel function; (7) bladder function; (8) ability to perform activities of daily living; (9) nutrition; and (10) social resources. All items in the KFI_PC are already embedded in and displayed on a mobile notepad so that the nurses and doctors can easily evaluate the patient, determine the frailty index score, and assess risk factors for frailty, which are automatically displayed on the notepad. In the ICOOP_Frail study, patients with KFI_PC scores ≥0.25, which is defined as frail, are randomized into experimental or control groups (Fig. 1).
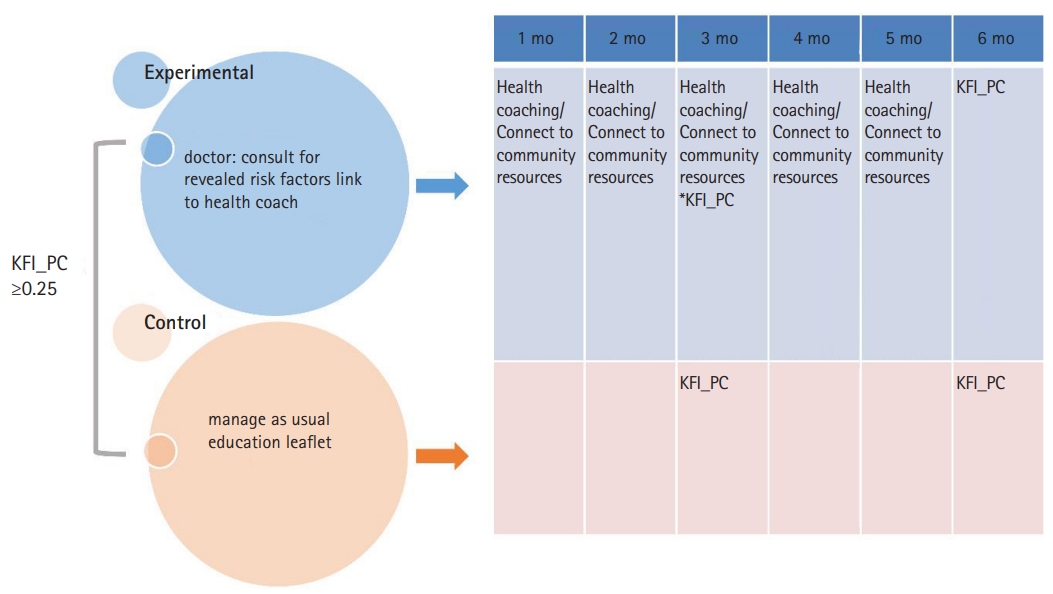
ICOOP_Frail study, patients with the Korean Frailty Index for Primary Care (KFI_PC) scores ≥0.25, which is defined as frail, are randomized into experimental or control groups.
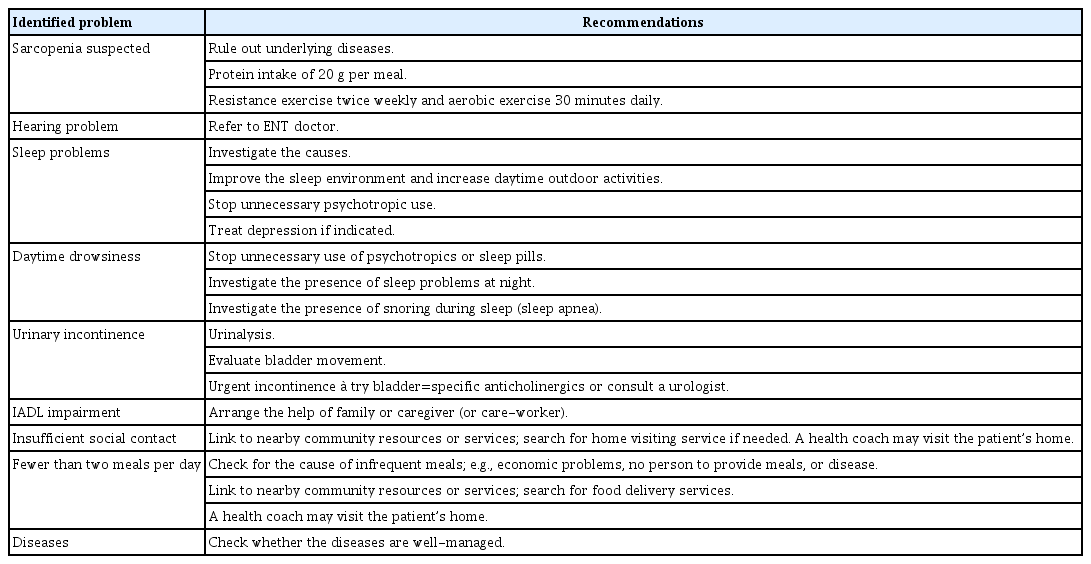
In the experimental group, primary care physicians explain functional declines or risk factors and educate patients about nutrition or exercise, adjust medication, and manage diseases based on the recommendations automatically displayed for the patient (Table 2). Within 1 month, a health coach contacts the patient via telephone to monitor the patient and encourage their consumption of a protein-rich balanced diet or/and practicing exercise, as well as connects the patient to community resources for social support, if needed. We surveyed the available community resources for social welfare services managed by community administration centers or senior welfare centers in advance to connect the participants to favored services. Unfortunately, all community services have been closed due to the coronavirus disease 2019 (COVID-19) pandemic. The health coaches involved in ICOOP_Frail are paramedical students studying gerontologic epidemiology at Kyung Hee University. In the future, volunteers or public health workers in the community will be welcome to serve as health coaches. The phone call for health coaching is repeated monthly for a total of 6 months. The KFI_PC is re-evaluated after 3 and 6 months. The primary outcome variables were defined as frailty index and the number of acute medical visits, while activities of daily living, health habits (exercise, diet), social activities, and gait ability were defined as the secondary outcomes.
WHO ICOPE AND ICOOP_FRAIL IN PRIMARY CARE
IC and frailty represent the two faces of the same coin. One indicates individual reserves, while the other indicates deficits that have accumulated with aging.2) Although both frailty and IC are dynamic entities, frailty is mainly evaluated in cross-sectional assessments, while IC is often used in longitudinal approaches. However, instead of the frailty phenotype, the frailty index can also be used in longitudinal approaches. The frailty index is related to declines in physical, psychological, cognitive, sensory, and social functions and can be used to identify not only frail persons but also those at risk of frailty.5) In addition, the frailty index and IC are based on the assumption that aging individuals can be adequately assessed and managed only if comprehensively evaluated and followed in a novel healthcare model based on service integration and multidisciplinarity.2) Therefore, the integrated care of older patients with frailty or risk of frailty based on the frailty index is as important for achieving healthy aging as reducing frailty is for promoting healthy aging.6)
The WHO has described steps to evaluate and scale-up ICOPE, including a prospective study in 2–3 countries (low and middle income, as well as high income) in 2021–2022 to test its feasibility and a multinational randomized study in 2022–2024 to validate its clinical efficacy and effectiveness. The managed care system in Korea has implemented a chronic disease management program in primary care9) and evaluated a technology-enhanced integrated care model for a frail older person in nursing home;10) however, the ICOOP_Frail study is the first integrated care program for frailty or functional decline in primary care in Korea.
Comparisons of the eight core items of WHO ICOPE and 53 items of the KFI_PC in ICOOP_Frail showed that all the eight core items of the ICOPE were well integrated into the KFI_PC (Table 3). In addition, WHO ICOPE and ICOOP_Frail both (1) are designed to be implemented in primary care at the community level, (2) are integrated programs that consider not only medical but also social and psychological aspects; (3) develop personalized care plans; and (4) aim to promote healthy aging (Table 4). Therefore, we suggest that the ICOOP_Frail study can be utilized as a reference study for ICOPE studies in Korea or may provide important findings for future studies on ICOPE implementation in Korea. However, ICOOP_Frail does not include the referral pathway and caregiver support addressed in ICOPE.

Eight core items of the WHO ICOPE and their corresponding items in the Korean Frailty Index for Primary Care (KFI_PC)
CONCLUSION
The WHO recently endorsed the proposal for a Decade of Healthy Aging (2020–2030). The WHO defines “healthy aging” as “the process of developing and maintaining the functional ability that enables wellbeing in older age.” Among the strategies to implement the Decade of Healthy Ageing, the WHO suggested the enhancement of intrinsic capacity and use of the ICOPE package program.
ICOOP_Frail is the first integrated care program for frailty or functional decline in primary care in Korea. Comparison of the eight core items of the WHO ICOPE to the 53 items of the KFI_PC revealed that all the eight core items were well integrated into the KFI_PC, upon which the ICOOP_Frail study was based.
We suggest that the ICOOP_Frail study can be utilized as a reference study for ICOPE studies in Korea or provide important findings for future ICOPE implementation studies in Korea.
Acknowledgements
This work was supported by National Research Foundation (NRF) grants, funded by the National Evidence-based Healthcare Collaborating Agency (Grant No. NECAIRB20-021-2; Research No. NA20-007). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding sources.
Notes
CONFLICT OF INTEREST
The researchers claim no conflicts of interest.
AUTHOR CONTRIBUTION
Conceptualization, CWW, HK; Supervision, CWW, HK; Writing-original draft, CWW; Writing-review & editing, EH, JP, JEB, SK, SBK, JR, JHC, SYJ, HJ, DL, YS, HS; CWW, EH, EJ, MK, HK.