Mycobacterium abscessus Skin Infection Associated with Shaving Activity in a 75-year-old Man
Article information
Abstract
Mycobacterium abscessus comprises rapidly growing mycobacteria, and the clinical manifestations of M. abscessus skin infection include papule, nodule, ulcer, scar and mixed form. The cutaneous infections have been reported due to minor trauma, cosmetic therapy, acupuncture and disseminated infection. A 75-year-old man presented with pruritic diffuse various sized erythematous papuloplaques and pustules on the neck and chest for 2 months. The cutaneous lesions were spread around the wound of the shaving on the neck. The histopathologic findings were consistent with abscess showing infiltrations of neutrophils and lymphocytes in the dermis and negative findings were observed on immunohistochemical stain including acid-fast bacilli stain. One month later, mycobacterial culture result showed positive findings, and the pathogen was identified by reverse-transcriptase polymerase chain reaction with hybridization. The patient was treated with combination of clarithromycin and ethambutol for 5 months and there is no evidence of recurrence after 6 months of follow-up. Herein, we report a case of M. abscessus cutaneous infection through minor trauma caused by shaving in the elderly.
INTRODUCTION
Recent decades have seen a significant increase in the number of nontuberculous mycobacteria (NTM) infections worldwide.1) Although the epidemiology of NTM infection remains unknown, NTM infections are more likely to occur in elderly populations.2) The mean age of NTM patients is between 50–70 years and advanced age is a poor prognostic factor.3)
Mycobacterium abscessus, one of the subspecies of NTM, is an important pathogen due to its increasing prevalence and treatment difficulties due to the potential for multidrug-resistance.1) We report a case of the successful treatment using the combination of clarithromycin and ethambutol of an M. abscessus skin infection of a wound caused by shaving in a patient.
CASE REPORT
A 75-year-old man presented with pruritic, diffuse, variously-sized erythematous papuloplaques and pustules on his neck and chest that had been present for 2 months. The initial lesion was a wound that developed while shaving the hairs on the lateral side of his neck using a wet razor; however, the lesions were spread to his chest in the form of erythematous papuloplaques and pustules (Fig. 1A). He was taking medications for hypertension, renal insufficiency, and stroke. There were nonspecific findings in his family history.
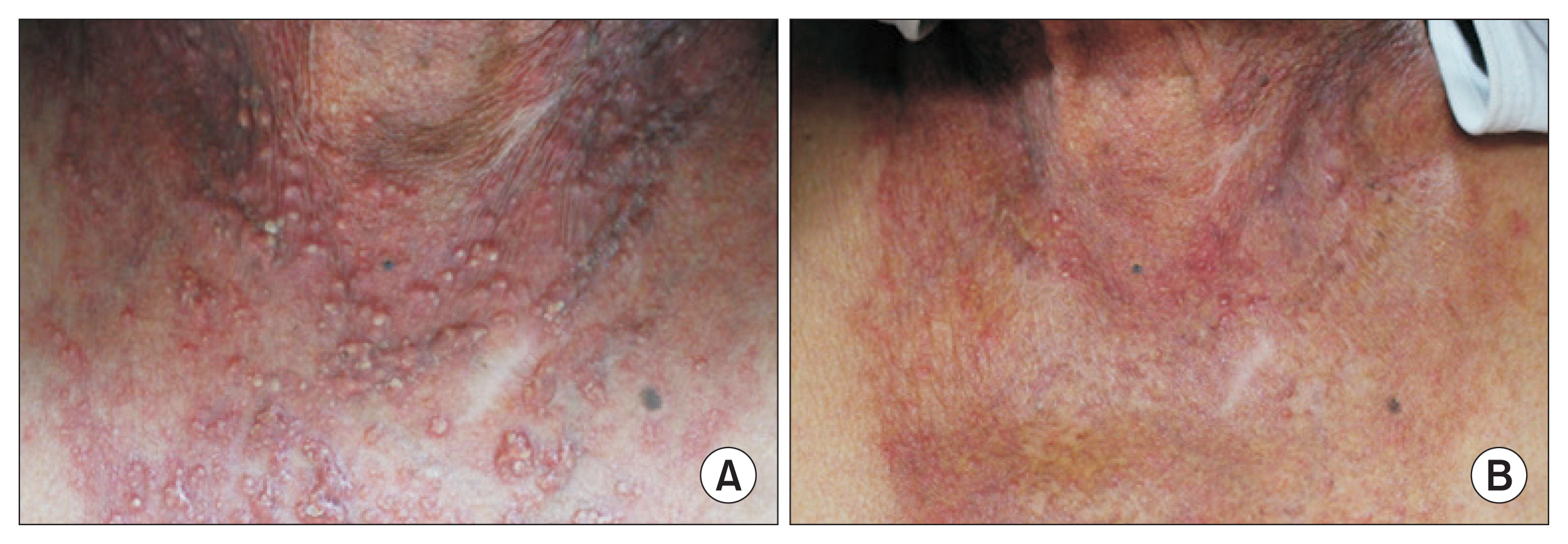
(A) Diffuse erythematous papuloplaques and pustules on the chest. (B) The lesions were almost cleared after 3 months of treatment with combination of clarithromycin 1,000 mg/day and ethambutol 800 mg/day.
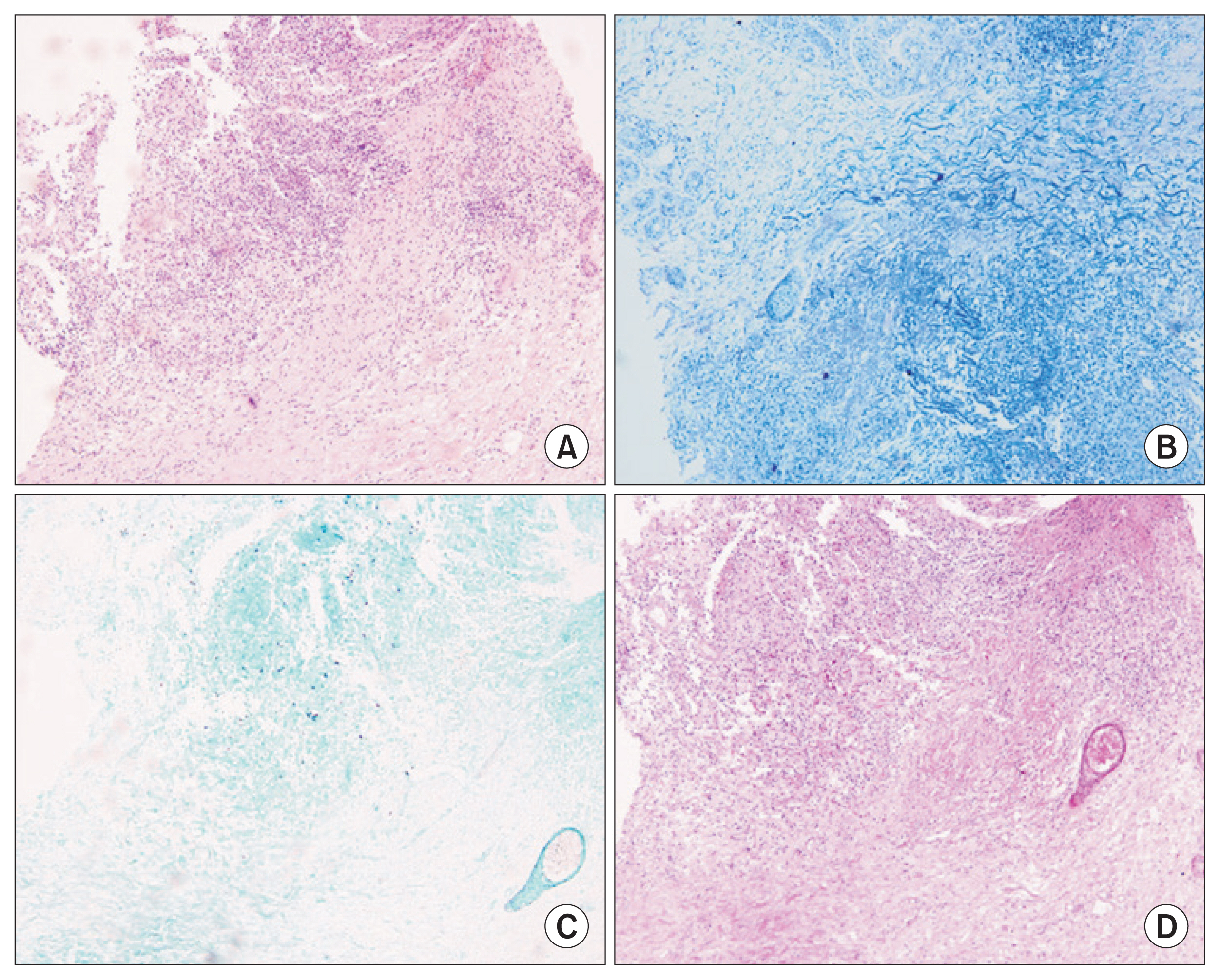
Potassium hydroxide tests of the pustules were negative. Therefore, a biopsy was performed of the chest lesion and Gomori methenamine silver (GMS) staining; periodic acid-Schiff (PAS) staining; acid-fast staining; and bacterial, fungal, and mycobacterial cultures were performed using the biopsied specimen. No abnormalities were observed in complete blood cell count and routine chemistry. The histopathologic findings revealed neutrophil and lymphocytic infiltrations, which were consistent with an abscess (Fig. 2A), but the GMS, PAS, acid-fast bacilli (AFB), immunohistochemical staining (Fig. 2B–D), and bacterial and fungal culture findings were negative. Itraconazole 200 mg/day and isoconazole cream were used for treatment of a suspected deep fungal infection for 1 month, but there was no improvement. On the 32nd day of mycobacterial culture, NTM were observed and the subspecies was confirmed as M. abscessus by reverse-transcriptase polymerase chain reaction (RT-PCR) with hybridization. We treated the patient with a combination of clarithromycin 1,000 mg/day and ethambutol 800 mg/day for 5 months, and there has been no evidence of recurrence after 6 months of follow-up (Fig. 1B). The patient gave full permissions for the publication of this paper and use of photographs.
DISCUSSION
M. abscessus, along with M. chelonae and M. fortuitum, are rapidly-growing mycobacteria ubiquitous in the soil and water.2) M. abscessus can cause infections in all human organs, but most commonly causes skin and soft tissue infections.4) Although the incidence of NTM infection has increased in recent decades, it is unclear whether this increase is due to actual infections or due to technological advances identifying the exact pathogens.5) Nevertheless, the elderly are more susceptible to NTM infection and have an increased morbidity.3)
The cutaneous infection routes include direct contact with contaminated materials through trauma or secondary infection in patients with disseminated disease.6) The appearance of skin lesions varies among papules, nodules, ulcers, scarring, and mixed forms, and the infection may appear as papules and pustules in some serious cases. The primary cutaneous infections are present on exposed areas that are vulnerable to injury and lesions usually occur locally; however, multiple lesions may occur when the pathogens are spread through the lymphatic system.7) The histologic findings may show lymphocytic infiltration around the blood vessels of the dermis and granuloma caused by eosinophils, plasma cells, and giant cells with no neutrophil component in the deep dermis. Additionally, neutrophilic abscess with mild granulomatous reaction may also be observed. In severe cases of inflammation, neutrophil deposition and edema may be seen throughout the dermis. Generally, systemic symptoms, such as fever and myalgia, are rare.1)
M. abscessus can be diagnosed by Ziehl-Neelsen staining, culture in Lowenstein-Jensen or Ogawa medium, and PCR. Ziehl-Neelsen staining and culture may show false-positive results. PCR is a method used to precisely identify strains by analyzing the results obtained by amplifying the 16S rRNA, hsp65, and rpoB genes, which differ in each NTM species. Recently, the sensitivity has been increased by methods such as polymerase chain reaction-rectification fragment length polymorphism.1,7) Identification of the exact strain in the infection is important because they may have different antibiotic sensitivities.7)
M. abscessus tends to be resistant to many antibiotics, making its treatment difficult. Therefore, if M. abscessus is identified, antibiotic susceptibility testing should be performed. A study of antibiotic susceptibility of M. abscessus in Korea revealed it to be most sensitive to amikacin (99%) and cefoxitin (99%), followed by imipenem (55%) and tobramycin (36%) among the parenteral antibiotics. Among oral antibiotics, M. abscessus was most susceptible to clarithromycin (91%), moxifloxacin (73%), ciprofloxacin (57%), and doxycycline (7%).8)
There is no exact guideline for the treatment of M. abscessus infection. Clarithromycin monotherapy can generally be used for local infection but should be used with caution because of the potential for antibiotic resistance. Combination therapy with clarithromycin and parenteral antibiotics such as amikacin or cefoxitin is recommended for severe cases.5) In addition, antibiotics should be used for 4 months for mild infections and for 6 months for severe infections.9) Patients with disseminated infections often have poor immunity, so surgical debridement of necrotizing tissue or drainage may be better than antibiotic combination therapy alone.9)
We experienced a case of primary cutaneous infection caused by M. abscessus in an elderly patient with comorbidities and a history of minor trauma from a razor blade. The lesion might be similar to other diseases such as deep fungal infection and lupus vulgaris. We confirmed the NTM infection and NTM strain using skin biopsy, mycobacterial culture, and RT-PCR with hybridization. Although we could not perform drug sensitivity testing, he was well treated with the combination of clarithromycin and ethambutol.
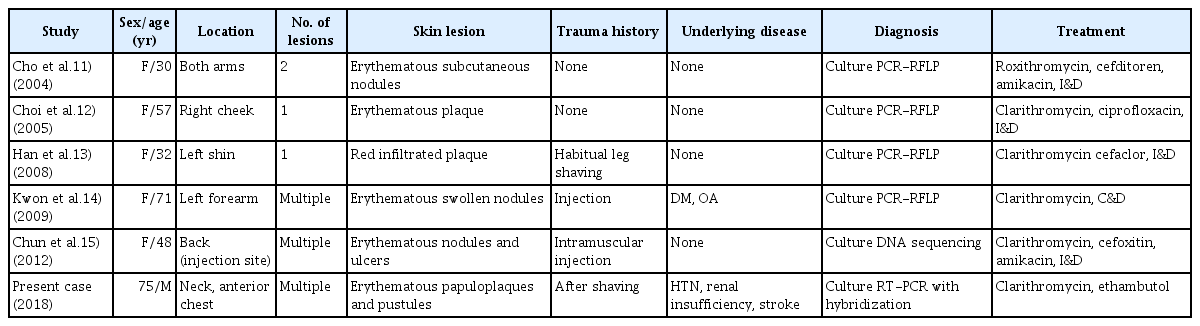
The incidence of NTM skin infections in older adults has been increasing recently. This increase may be due to decreased T cell and cytokine activities with aging, which are important for the pathogenesis of NTM infection.10) Some cases of M. abscessus skin infection have been reported in Korea (Table 1), however, to our knowledge, there have been no other reported cases of M. abscessus infection presenting with multiple and diffuse lesions after shaving in the elderly. Decreased immunity in the elderly could be related to the appearance of multiple and widespread lesions. Papules or pustules at the shaving site among those who shave daily may be easily mistaken for folliculitis. When the lesions do not respond to treatment for folliculitis, it is important to perform the necessary tests to identify pathogens such as NTM.
Notes
The researchers claim no conflicts of interest.