A Comparison of Memory Beliefs, Cognitive Activity, and Depression Among Healthy Older Adults, Amnestic Mild Cognitive Impairment, and Patient with Alzheimer’s Disease
Article information
Abstract
Background
Amnestic mild cognitive impairment (aMCI) is highly likely to progress to dementia of the Alzheimer type (DAT). One of the most frequently reported symptoms in aMCI and DAT patients is memory impairment. This study compared the levels of beliefs about memory efficacy and control, cognitive activity, and depression among healthy older adults (OA), patients with aMCI, and patients with DAT.
Methods
This study included 21 OA (11 males, 10 females), 16 aMCI patients (6 males, 10 females), and 18 DAT patients (10 males, 8 females). The memory efficacy questionnaire, memory control questionnaire, cognitive activity questionnaire, depression questionnaire, and Seoul Verbal Learning Test were administered to all subjects.
Results
DAT patients showed significantly lower scores on the recognition test than did the OA and aMCI patients, and no difference in these scores was observed between the OA and aMCI patients. Regarding the memory efficacy, memory control, and cognitive activity questionnaires, DAT and aMCI patients showed significantly lower scores than did OA. However, there were no differences in these scores between aMCI and DAT patients.
Conclusion
The results of this study suggest that aMCI patients experienced impairment in memory beliefs and memory control in the same way as DAT patients did. These results suggest that the early application of cognitive rehabilitation therapy for patients with aMCI may be effective in preventing or alleviating memory deterioration.
INTRODUCTION
As we are entering the era of an aging society, the incidence and prevalence of chronic diseases in the older population are increasing. One of the most notable diseases is dementia.1) In recent years, mild cognitive impairment (MCI), which is considered a prodromal stage of dementia, has received much attention. MCI refers to a cognitive decline greater than expected for an individual’s age and education level that does not meet the criteria for dementia and in which daily functioning is maintained.2,3) Among MCI subtypes, amnestic MCI (aMCI) is characterized by memory decline and is highly likely to progress to dementia of the Alzheimer’s type (DAT).2,3)
Even older people who do not have dementia or aMCI often complain of memory problems. The factors affecting memory performance in older individuals include age, sex, education level, social resources, personal experience, religious activity, memory beliefs, memory control, cognitive activity, and depression.4–12)
These aforementioned variables affecting memory have been studied extensively. However, fewer studies have assessed variables related to psychological factors such as metamemory. In addition, only a few studies have investigated memory efficacy and memory control, which are considered a part of metamemory, as independent variables.13,14) Therefore, the aim of this study was to compare the differences in factors affecting memory performance—such as memory beliefs (memory efficacy and memory control), the psychological factor; level of cognitive activity, the activity factor; and level of depression, the emotional factor—in healthy older adults (OA), patients with aMCI, and patients with DAT.
MATERIALS AND METHODS
Twenty-one OA (11 males, 10 females) from the elderly welfare center in the Incheon area and 16 aMCI (6 males, 10 females) and 18 DAT (10 males and 8 females; 12 and 6 with Clinical Dementia Ratings [CDRs] of 1 and 0.5, respectively) patients from the Incheon St. Mary’s Hospital, Catholic University of Korea, Neurology and Dementia Clinic Center participated in the study. The study was approved by the Institutional Review Board of the Incheon St. Mary’s Hospital (OC13OISI0083). Written informed consent was obtained from all participants. The clinical diagnosis of probable Alzheimer’s disease was made according to the National Institute of Neurological and Communicative Diseases and Stroke/Alzheimer’s Disease and Related Disorders Association (NINCDS-ADRDA) criteria and a Hachinski ischemic score of less than 3 points.15) Patients with brain-related disorders that may affect cognition, such as cerebrovascular disease, were excluded based on brain magnetic resonance imaging findings. Patients with metabolic disturbances such as thyroid dysfunction, hyperglycemia (>125 mg/dL), hypoglycemia (<50 mg/dL), and liver or renal dysfunction were also excluded. The memory efficacy questionnaire and memory control questionnaire were used to evaluate memory beliefs.16,17) Specifically, a modified version of the questionnaire developed by Berry et al.11), which included ten questions that were translated and modified to suit older individuals in Korea, was used to evaluate memory efficacy.18) Similarly, a modified version of the questionnaire developed by Lachman (1995) that is suitable for older Korean individuals was used to evaluate memory control.19) To assess the level of cognitive activity and depression, the cognitive activity level questionnaire and the Korean version of the depression short form scale, respectively, were used.20–22) To assess the overall level of cognitive function, the Korean Mini-Mental State Examination (K-MMSE) was administered, and the level of dementia was assessed by the CDR.23,24) The Seoul Verbal Learning Test (SVLT), which is the most frequently used measure of memory performance, was used to evaluate verbal memory.25)
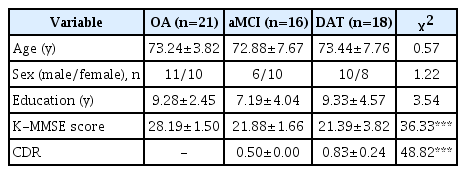
All statistical analyses were performed using SPSS, version 16.0 (SPSS Inc., Chicago, IL, USA). The Kruskal–Wallis test, a nonparametric test, was used to compare the three groups. In addition, we used the Mann-Whitney test to compare the differences among the three groups. The results of the Kruskal–Wallis tests showed no significant difference in age, education, and gender. There were differences in K-MMSE total scores among the three groups (χ2=36.331, df=2, p<0.0005). The results of the Mann–Whitney tests revealed a significantly higher score in the OA group than in the aMCI and DAT patients; however, the scores of the aMCI and DAT groups did not differ significantly (OA>aMCI=DAT). The CDR scores also differed significantly among the three groups (χ2=48.825, df=2, p<0.0005). The Mann–Whitney tests showed significantly lower scores in the OA than in the aMCI and DAT groups, while the score in the DAT group was significantly higher than that in the aMCI group (OA>aMCI>DAT).
RESULTS
There were no significant differences in age, education, and gender among the three groups; however, the K-MMSE and CDR scores differed significantly (Table 1). The K-MMSE total score was significantly higher in the OA group than in the aMCI and DAT groups, but there was no significant difference in scored between the aMCI and DAT groups (OA>aMCI=DAT). The OA group showed the highest CDR scores, followed by the aMCI and DAT groups (OA>aMCI>DAT).
On the immediate recall of the SVLT, DAT patients showed the worst performance, followed by aMCI patients, who showed a poorer performance than OA. DAT and aMCI patients showed lower performance scores than OA on the delayed recall test, but no difference between DAT and aMCI patients was observed. In contrast, DAT patients showed significantly lower performance scores than OA and aMCI patients on the recognition test, and no difference was observed between OA and aMCI patients. These results suggest that the deterioration of memory in the case of aMCI may mainly be due to deficits in coding (registration) and retrieval capability. There was no difference in depression scores among the three groups. For memory efficacy, memory control, and cognitive activity level, the scores of DAT and aMCI patients were significantly lower than those of OA. However, there was no difference between aMCI and DAT patients. The level of cognitive activity in daily life was also significantly lower in aMCI and DAT patients than in OA (Table 2).
DISCUSSION
Previous studies on metamemory as a psychological factor affecting memory performance were performed mostly in healthy individuals rather than patient populations. In contrast, our study investigated memory efficacy and memory control, which are considered a part of metamemory, in patients with aMCI and DAT. Memory efficacy refers to an individual’s thoughts about his or her memory ability. Memory control can be defined as an individual’s thoughts about his or her ability to control memory. In previous studies on memory beliefs, older people reported lower levels of memory efficacy and memory control than did adolescents and middle-aged adults.11,12,26–29) Moreover, aging is associated with a decline in one’s ability to control cognitive function and memory function. While several studies have reported that memory performance is partly related to memory beliefs, other studies have shown a relatively weaker relationship between memory performance and beliefs than expected.30–32)
The results of this study showed that memory efficacy and memory control were significantly poorer in patients with aMCI and DAT than in OA, suggesting that aMCI patients yet to be diagnosed with dementia already experience impairments in memory efficacy and memory control, similar to DAT patients. Based on the results of our study as well as previous reports suggesting that non-pharmacological interventions may help alleviate symptoms in Alzheimer’s patients, cognitive rehabilitation therapy related to the maintenance and improvement of memory efficacy and memory control from the aMCI stage rather than from early-stage Alzheimer’s disease may help to relieve patient symptoms.33–35)
A number of studies have reported a statistically significant relationship between the level of cognitive activity and memory performance.36,37) In the present study, the cognitive activity of patients diagnosed with aMCI and DAT was significantly lower than that of OA. Previous studies showed that cognitive activity and memory performance maintain a static relationship in OA. In aMCI and DAT patients with memory impairment, low cognitive activity in daily life may also have some impact on memory impairment. Therefore, it may be helpful to increase cognitive activity, and interventions from the aMCI stage may be more effective.
In conclusion, it is important to precisely determine the factors (psychological/cognitive activity/emotional) that affect memory deterioration in patients with aMCI and DAT. Interventions such as timely non-pharmacological treatment to delay or stop the deteriorating factors may contribute to the maintenance and improvement of patients’ symptoms. Finally, the limitations of this study include the inability to study various factors related to non-pharmacological treatment, the modest number of subjects, and the lack of any evaluation of a cognitive rehabilitation treatment program.
ACKNOWLEDGMENTS
This study was supported by the Brain Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science and ICT of Korea (NRF-2015M3C7A1064832).
Notes
The researchers claim no conflicts of interest.