Prevalence of Adrenal Insufficiency in Korean Patients undergoing Total Knee Arthroplasty
Article information
Abstract
Background
This study investigated the prevalence of adrenal insufficiency among patients admitted for total knee arthroplasty (TKA) due to osteoarthritis and identified factors contributing to adrenal insufficiency.
Methods
We divided the patients into two groups based on the results of preoperative standard-dose short synchronous stimulation tests: group 1 (adrenal insufficiency) and group 2 (normal adrenal function). We also assessed the prevalence of adrenal insufficiency and compared the numbers of patients who received oral steroids, the frequency of previous steroid injection use, and the frequency of systemic symptoms of steroid depletion such as fatigue and loss of appetite between the two groups. Multiple regression analysis was performed to identify factors related to adrenal insufficiency.
Results
The prevalence of adrenal insufficiency was 60.0% (120/200). Group 1 had higher numbers of previous steroid injections (12.8±10.2 vs. 6.8±7.9) and patients taking oral steroids (18/120 vs. 3/80) (p<0.001 and p=0.011, respectively). The frequency of systemic symptoms of steroid depletion, such as fatigue and loss of appetite, was also higher in group 1 (94/120 vs. 42/80, p<0.001). Recent steroid injections and loss of appetite were associated with adrenal insufficiency (p=0.002 and p=0.009, respectively).
Conclusion
The results of this study revealed a high prevalence of adrenal insufficiency in Korean patients hospitalized for TKA due to end-stage osteoarthritis. Recent steroid injections were causally related to the development of adrenal insufficiency. Therefore, adrenal function should be assessed preoperatively to prevent postoperative complications related to adrenal insufficiency.
INTRODUCTION
The prevalence of adrenal insufficiency is approximately 250–400 per million, while that of secondary adrenal insufficiency is 150–280 per million.1,2) Individuals with advanced osteoarthritis may be at risk of developing adrenal insufficiency because of repeated oral steroid administration or intra-articular steroid injections.3,4) Individuals with adrenal insufficiency may be able to perform daily activities without showing any symptoms.5) However, once they are exposed to stressful situations, such as infection, trauma, or surgery, they may experience life-threatening adrenal crisis.6) The symptoms of adrenal crisis include weakness, nausea, vomiting, and abdominal pain. In surgical patients, it is often difficult to differentiate these symptoms from those of cerebrovascular accidents, ileus, and sepsis.7) However, untreated adrenal crisis can develop into coma and hypotension, with a high mortality rate.7,8) As symptoms of adrenal crisis are nonspecific, early diagnosis is difficult unless the underlying adrenal insufficiency is identified in advance.
In particular, older adult patients who undergo total knee arthroplasty (TKA) for severe osteoarthritis are more difficult to manage than other age groups in terms of the incidence rate, symptom ambiguity, and mortality rate.9,10) As a result, these patients may be misdiagnosed, and the optimal timing of treatment may be missed. To promptly diagnose adrenal crisis and provide timely and appropriate management, patients must be assessed for adrenal insufficiency before surgery and patients with insufficiency carefully monitored for adrenal crisis symptoms after surgery. However, because the prevalence of adrenal insufficiency is very low, the evaluation of adrenal function before surgery is not routinely performed in practice.
The present study investigated the prevalence of adrenal insufficiency among patients in Korea admitted for TKA who underwent assessment using a standard-dose short synacthen stimulation test and identified the contributing factors associated with adrenal insufficiency.
MATERIALS AND METHODS
Subjects
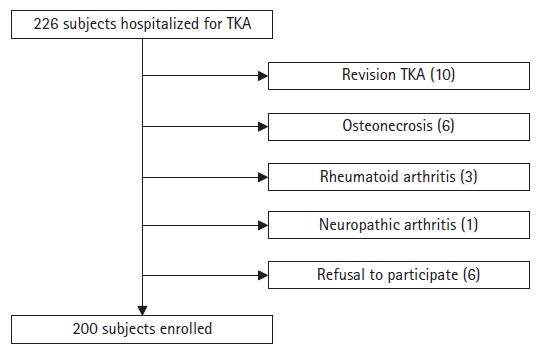
This prospective cross-sectional study was conducted from March to December 2022 after receiving the approval of the Institutional Review Board of our institution. We recruited all patients hospitalized for TKA for severe arthritis (Kellgren–Lawrence grade 3 or 4).11) We obtained informed consent from all patients before their study inclusion. The exclusion criteria were rheumatoid arthritis, osteonecrosis, neuropathic arthropathy, and revision total TKA. Patients who refused to participate were also excluded (Fig. 1).
Methods
We surveyed the patients for a history of steroid use as a treatment modality, such as spinal nerve block, intra-articular injection, autoimmune connective tissue diseases, asthma, chronic obstructive pulmonary disease, skin diseases, and a family history of autoimmune diseases. We determined the number of steroid injections in the past 3 months using a questionnaire. We reviewed the medical records of the relevant medical institutions for patients who had received so many steroid injections that they could not accurately recall the number of times they had received them. We also investigated the history of oral steroid administration and daily dose of oral steroids in the past 3 months.
Before hospitalization, we asked the patients about symptoms such as fatigue and loss of appetite that might appear during steroid depletion.12,13) Fatigue was defined as an average score of ≥4 on the 11-point rating scale in the brief fatigue inventory.14) We assessed appetite using visual analog scale (VAS) ratings (0–100 mm; 0 = no appetite at all, 100 = very good appetite).15,16) Loss of appetite was defined as a VAS score for appetite of ≤70.15) We also assessed whether the patients had been previously diagnosed with adrenal insufficiency. Patients who were taking hydrocortisone discontinued it 24 hours before the short synacthen stimulation test, and those taking prednisone or prednisolone switched to an equivalent dose of hydrocortisone 1–2 weeks before the stimulation test and discontinued it 24 hours before.
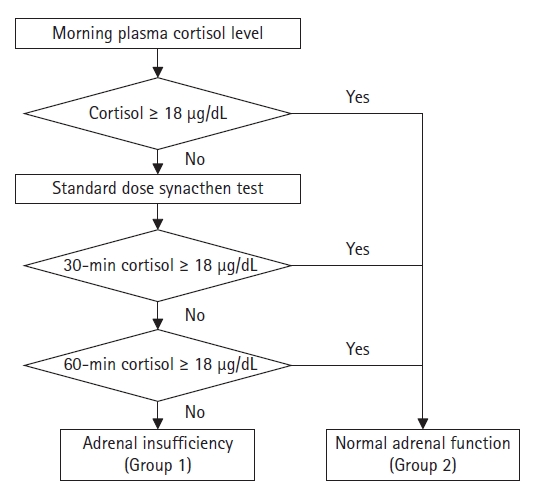
On the morning of the day of surgery, the patients underwent a standard-dose short synacthen stimulation test, in which 250 µg of synacthen was intravenously administered immediately after taking a blood sample to measure the basal blood cortisol concentration.17) We measured blood cortisol concentrations before and 30 and 60 minutes after synacthen administration. A normal basal blood cortisol concentration of ≥18 µg/dL was defined as normal adrenal function regardless of the results of the synacthen stimulation test. Adrenal insufficiency was defined as a blood cortisol concentration of <18 µg/dL at 30 and 60 minutes after synacthen administration. Patients diagnosed with adrenal insufficiency were classified into group 1, while those with normal adrenal function were included in group 2 (Fig. 2). An endocrinologist verified the diagnostic protocol for adrenal insufficiency.
Outcome Assessments
We also assessed the prevalence of adrenal insufficiency. We compared the proportions of patients who had received steroid injections within the past 3 months and the number of steroid injections between the two groups. Similarly, we also compared the proportions of subjects who had taken oral steroids daily in the last 3 months. The correlation between the prevalence of adrenal insufficiency and the American Society of Anesthesiologists (ASA) classification18) was analyzed. Finally, we compared the frequency of the manifestation of symptoms of steroid depletion between the two groups.
Statistical Analyses
All statistical analyses were performed using IBM SPSS Statistics for Windows, version 22.0 (IBM Corp., Armonk, NY, USA). Means and standard deviations are used to describe the data. Comparisons between the two groups were conducted using the Student t-test for continuous variables and the chi-square test for categorical variables. We performed a multiple logistic regression analysis to identify factors associated with adrenal insufficiency among the variables that showed statistically significant differences between the two groups. Statistical significance was set at p<0.05.
Ethical Statement
Primary approval was obtained from the Institutional Review Board of Kangwon National University Hospital (No. KNUH-2022-01-021-001). Informed consent was obtained from all the study participants. This study complied the ethical guidelines for authorship and publishing in the Annals of Geriatric Medicine and Research.19)
RESULTS
Among 226 recruited patients, 200 were enrolled in the study. Their demographics according to the groups are presented in Table 1. Forty-seven patients were male and 153 were female. The mean age was 72.8±6.9 years. The mean body mass index was 27.0±3.6 kg/m2. Of 200 patients, 120 (60.0%) were diagnosed with adrenal insufficiency. None of the patients had been previously diagnosed with adrenal insufficiency. One hundred and one patients underwent unilateral TKA, and 99 underwent simultaneous or sequential bilateral TKA. There was no significant difference in the prevalence of adrenal insufficiency according to the bilaterality of the joint arthroplasty (p=0.299). Two patients in group 2 had preoperative serum sodium levels <135 mmol/L (122 mmol/L and 132 mmol/L, respectively). No patients in group 1 had a preoperative serum sodium level <135 mmol/L. The distribution of ASA classifications did not differ significantly between the two groups (p=0.491). The basal plasma adrenocorticotropic hormone (ACTH) and basal and stimulated blood cortisol levels are shown in Table 2.
The mean numbers of steroid injections were 12.8±10.2 in group 1 and 6.8±7.9 in group 2 (p<0.001). In the past 3 months, 77.5% (93 of 120) patients in group 1 and 55.0% (44 of 80) patients in group 2 had received steroid injections, and 14.2% (17 of 120) patients in group 1 and 5.0% (4 of 80) patients in group 2 had taken oral steroids (p<0.001 and p=0.038, respectively) (Table 3). However, of the 62 patients with no history of injection or oral steroid use within 3 months before surgery, 26 (41.9%) were diagnosed with adrenal insufficiency.
The frequency of systemic symptoms of steroid depletion, such as fatigue and loss of appetite, was higher in group 1 (p<0.001) (Table 4). The results of the logistic regression analysis for the variables that differed significantly between the two groups are shown in Table 5.
DISCUSSION
The principal findings of this study were as follows: (1) the overall prevalence of adrenal insufficiency was 60.0% in patients hospitalized to undergo primary TKA for osteoarthritis, and (2) the frequency of steroid injections administered within 3 months before surgery and the loss of appetite, which is one of the symptoms of steroid depletion, were predictive factors of adrenal insufficiency.
Adrenal insufficiency is a rare disease affecting only 2–4 people per 10,000 people in the population.1,2) Individuals who have not experienced serious stress may continue their daily lives without any significant symptoms. Owing to its low incidence and lack of symptoms under normal circumstances, routine preoperative screening for adrenal function is typically not performed in patients undergoing orthopedic surgery. However, patients with adrenal insufficiency undergoing major surgeries, such as joint replacement, which can cause significant stress, are at risk for adrenal crisis. The probability of mortality is high without proper treatment. The results of the present study revealed a 60% prevalence of adrenal insufficiency, a rate much higher than previously reported. Moreover, none of the patients in this study had previously been diagnosed with adrenal insufficiency.
In this study, patients with adrenal insufficiency had significantly higher rates of injection and oral steroid use than the control group. Additionally, a history of steroid injections into the joint or spine was a predictive factor for adrenal insufficiency, whereas a history of oral steroid use was not. Of the 200 included patients, 21 had taken oral steroids, including 6 and 15 who were using hydrocortisone and prednisolone, respectively. The hydrocortisone doses were 10–15 mg/day, while those for prednisolone were ≥10 mg/day, exceeding the physiological dose. Most of these subjects had a history of using steroids for ≥3–4 weeks. Due to the diversity in steroid types, dosages, and durations of use, statistical analysis was not feasible. Previous studies have reported an increased risk of developing adrenal insufficiency in patients taking oral prednisolone at a dose of ≥5 mg/day or oral hydrocortisone at a dose of ≥15 mg for ≥3–4 weeks.20-22) In this study, the prevalence of adrenal insufficiency in patients using steroid inhalers did not differ significantly compared to that in patients not using inhalers. However, both steroid inhalers and ointments carry a risk of inducing adrenal insufficiency.23,24)
Temporary adrenal insufficiency caused by short-term steroid treatment is reversible, with recovery of adrenal function after steroid administration.25) Although this study specifically examined the prevalence of adrenal insufficiency at the time of surgery and did not investigate whether it was permanent or reversible, many patients experienced adrenal insufficiency during the perioperative period. Therefore, paying close attention to postoperative management is crucial in these cases. This study investigated medical conditions that could potentially cause adrenal insufficiency. However, the distribution of these conditions did not differ significantly between the two groups, making it difficult to identify a specific medical condition as the cause of adrenal insufficiency.
The risk of adrenal crisis in patients with adrenal insufficiency is approximately 10 in 100 patient years.26) The primary clinical features of adrenal crisis are hypotension and hypovolemia. However, the initial symptoms such as anorexia, nausea, vomiting, abdominal pain, fatigue, lethargy, fever, and altered consciousness are often nonspecific.6) While the prophylactic administration of steroids in patients with adrenal insufficiency can prevent adrenal crises, the postoperative administration of steroids to patients who have undergone artificial joint surgery may be avoided because of concerns about impaired wound healing and an increased risk of infection. Therefore, a strong conviction that these symptoms are due to an adrenal crisis is necessary to actively initiate steroid treatment. The misdiagnosis of patients with sepsis and subsequent delay in steroid administration can worsen their condition. Most cases of untreated adrenal crises result in death.8,27) Thus, prompt recognition and appropriate treatment of adrenal crises are essential for patient survival. During the study period, five patients with symptoms suggestive of adrenal crisis, including postoperative hypotension, mental changes, and respiratory failure, showed immediate improvement with steroid treatment. The tests for cerebrovascular accidents and pulmonary embolism yielded negative results.
The symptoms of adrenal insufficiency, such as fatigue and loss of appetite, may be nonspecific and may be overlooked in older adult patients with chronic arthropathy. However, the prevalence of these symptoms differed significantly between the two groups in this study. The results of the regression analysis further indicated that a loss of appetite was associated with adrenal insufficiency. Therefore, the surveillance of these symptoms may be helpful in screening for adrenal insufficiency.
This study has several limitations. First, the sample size was small. Considering the known prevalence of adrenal insufficiency, a larger sample size was required in this prospective study. However, a previous pilot study investigating the prevalence of adrenal insufficiency in subjects scheduled for TKA also observed a higher prevalence than previously reported. Secondly, this was a time-zero study. This study only investigated the prevalence of preoperative adrenal insufficiency without determining the effect of adrenal insufficiency on surgical outcomes. We did not provide prophylactic steroid supplementation to patients with adrenal insufficiency. Among patients with preoperative adrenal insufficiency, five exhibited symptoms of adrenal crisis shortly after surgery; however, their condition improved immediately after steroid supplementation. Third, synchronous stimulation testing results may yield false negative results or appear normal in cases of mild disease or with recent onset.28) In mild disease, sufficient adrenal functional cortex may exist to sustain adrenal reserve, enabling a suitable response to the standard dose of synacthen. Similarly, in cases with recent onset, sufficient time may not have elapsed for the adrenal gland to lose its complete function, allowing it to respond to synacthen stimulation. Finally, the number of steroid administrations, an important risk factor for adrenal insufficiency, was investigated based on the patients’ recall. While the oral medications taken by the patients at the time of admission were thoroughly examined, the medications they had previously taken orally and stopped before hospitalization may not have been completely investigated. Due to these limitations, it may be challenging to establish a definitive causal relationship between oral steroid use and the occurrence of adrenal insufficiency within the scope of this study. However, our results revealed adrenal insufficiency in most of the patients who did not receive steroid injections. Therefore, surgeons should be cautious when treating patients with end-stage osteoarthritis.
In conclusion, we observed a high prevalence of adrenal insufficiency in Korean patients hospitalized for TKA due to end-stage osteoarthritis. Recent steroid injections were causally related to the development of adrenal insufficiency. Therefore, adrenal function should be assessed preoperatively to prevent postoperative complications related to adrenal insufficiency.
Notes
CONFLICT OF INTEREST
The researchers claim no conflicts of interest.
FUNDING
This study was supported by the Research Grant from Institute of Medical Sciences, Kangwon National University 2022.
AUTHOR CONTRIBUTIONS
Conceptualization, SWB; Data curation, SWB, YSH; Investigation and Methodology, JHN; Writing_original draft, SWB, YSH, JHN; Writing_review & editing, SWB, YSH, JHN.