Psychosocial Determinants of Knee Osteoarthritis Progression: Results from the Promoting Independence in Our Seniors with Arthritis Study
Article information
Abstract
Background
Knee osteoarthritis (OA) is a common cause of physical disability among older adults. While established risk factors for knee OA include age and increased body weight, few studies have examined psychosocial risk factors or progression of knee OA.
Methods
The Promoting Independence in our Seniors with Arthritis study recruited participants aged 65 years and over from orthopedic outpatients and community engagement events. Participants were invited to annual visits during which knee OA symptoms were assessed with the Knee Injury and Osteoarthritis Outcome Score (KOOS), social network using the 6-item Lubben Social Network Scale and anxiety and depression using the Hospital Anxiety and Depression scale. Knee OA worsening was defined by a 5% reduction in mean KOOS scores at the last visit compared to the first visit.
Results
Data were available from 148 participants, mean age 66.2±6.5 years and 74.1% female, of whom 28 (18.9%) experienced OA worsening over a median follow-up period of 29 months. Univariate analyses revealed that age, sex, height, grip strength, and social network were associated with OA worsening. Social network remained statistically significantly associated with OA worsening after adjustment for age and sex difference (odds ratio=0.924; 95% confidence interval, 0.857–0.997). The relationship between social network and OA worsening were attenuated by both depression and handgrip strength at baseline.
Conclusion
Psychological status and muscle strength may be modifiable risk factors for social network which may in turn prevent knee OA worsening and should be targeted in future intervention studies.
INTRODUCTION
The pathophysiology of osteoarthritis (OA) has evolved from a disease of cartilage destruction to a systemic disease that affects the entire joint via mechanical, inflammatory, and metabolic factors, leading to a common final pathway of joint destruction.1) The prevalence of knee OA increased from 164 million cases to 364 million between 1990 and 2020, making OA a leading cause of morbidity among older adults, subsequently imposing a great cost to society as whole.2)
Psychological distress is common among older adults with depression, affecting an estimated 13% of the older population,3) whereas anxiety affects up to 10.2%.4) This is especially relevant in the post-coronavirus disease 2019 environment, in which 20.9% of the older cohort reportedly suffers from anxiety.5) Patients with arthritis have increased odds ratios of developing psychological sequelae.6) Furthermore, physical therapy prevents depressive symptoms in older adults with knee OA and subsyndromal depressive symptoms.7)
However, few studies have addressed the psychological and social determinants of knee OA and the factors that determine the worsening of knee OA symptoms. Our study attempted to address these gaps by evaluating the psychosocial factors associated with the worsening of OA in a prospective cohort followed up over a 4-year period.
MATERIALS AND METHODS
Data were utilized from the Promoting Independence in Seniors with Arthritis (PISA) longitudinal study comprising community-dwelling adults aged >65 years with and without knee pain recruited from the orthopedic clinic of the Universiti Malaya Medical Centre (UMMC) and a local hospital catchment area through public engagement events and word-of-mouth advertising. All participants provided written informed consent on recruitment before their first assessment. Individuals who did not provide informed consent were excluded. The UMMC Medical Research Ethics Committee provided ethical approval for this study (MECID No. 20147-390). This study complied the ethical guidelines for authorship and publishing in the Annals of Geriatric Medicine and Research.8)
Data Collection
Data were collected and managed using the REDCap electronic data capture tool hosted at the Universiti Malaya.9,10) During the first visit, the patients’ basic demographic data, including age, sex, marital status, and medical history, were recorded. Other parameters and new medical conditions were recorded during every annual visit, including physical and physiological measurements of height, weight, lying and standing blood pressure, muscle strength, and gait and balance. Additionally, psychosocial assessments, including the evaluation of anxiety, depression, life satisfaction, social networks, and social participation, were obtained. Knee OA symptom severity was measured using the Knee Injury and Osteoarthritis Outcome Score (KOOS).
Physical Performance
Muscle strength was determined using handgrip strength measured with a Jamar grip strength dynamometer (Sammons Preston, Bolingbrook, IL, USA). Handgrip strength was first measured in the dominant hand and then in the non-dominant hand. Each patient was asked to sit on a chair with the forearm resting comfortably on the armrest of the chair. The arm was flexed at 90° at the elbow and each patient was asked to squeeze the dynamometer as hard as possible when ready. The readings were recorded three times, and the average of the readings was calculated. This process was repeated for the non-dominant hand.
In the Timed-Up-and-Go test, each patient was asked to sit on a chair. Before starting the test, a marker was placed three meters from the chair. Each patient was then asked to stand up, walk in a straight line toward the mark, make a U-turn, walk back to the chair, and sit down as quickly as possible. The time required to complete this task was recorded using a stopwatch. The participants were asked to walk at their normal pace and speed with shoes on and use regular walking aids if required. A completion time of >13.5 seconds indicates impaired lower limb function.11)
Functional reach was measured with each participant standing close to the wall but not touching it. A tape measure was fixed to the wall at the level of the shoulder of the outstretched arm, parallel to the floor. The distance was measured from the fingertip of the middle finger. The participants were then asked to reach forward as far as they could without losing balance or taking steps forward. The functional reach was calculated as the difference between the final and initial measurements and was measured in centimeters.
Life Satisfaction
The Life Satisfaction Checklist was first designed by Fugl-Meyer in 1985 to assess post-stroke patients. It consists of seven items rated on a 6-point Likert scale.12) Individual satisfaction with life was assessed using an extended 9-item version of the Life Satisfaction Questionnaire (LiSAT-9). The answers were scored on a Likert scale of 1 to 6, indicating “very dissatisfying,” “dissatisfying,” “rather dissatisfying,” “rather satisfying,” “satisfying,” and “very satisfying,” respectively. The components included the participants’ perception of life, vocational situation, finance, leisure, social contact, sexual life, self-care ability, family life, and partner relationships. A higher score denotes greater satisfaction.
Activities of Daily Living
The Lawton Instrumental Activity of Daily Living (IADL) was first published in 1969.13) Lawton eight components to assess IADL were assessed at every visit in the present study. These eight were using a telephone, shopping, preparing food, housekeeping, doing laundry, using transportation, taking medications, and handling finances. Those who could not handle the task were assigned a score of zero, with higher scores indicating better functional capacity. Katz’s index of independence in activity of daily living (ADL) was first proposed in 1963. It consists of six questions regarding bathing, dressing, toileting, transferring, maintaining continence, and feeding. A higher score indicates a higher level of independence.14)
Social Participation and Network
Social participation was assessed using Keele Assessment of Participation (KAP), comprising seven questions assessing the respondent’s ability to move around in the house, move outside the house, perform self-care, look after the home, look after belongings, meet and speak to other people, and manage finances. Four additional questions were only triggered by positive responses to having dependents, participating in paid or voluntary work, or courses for training or education. The scores assigned were zero for all of the time, one for most of the time, two for some of the time, three for sometimes, and four for never. Lower scores indicate better participation, and total scores range from 0–36. The KAP was first published in 2005.15)
The Lubben Social Network Scale is a six-item self-reported questionnaire that measures social engagement with friends and family.16) The scale consists of three questions related to relationships with family and three questions related to friends. Responses are scored from zero for none to five points for nine or more people, wherein a higher scores indicates a better social network.
Measurement of Anxiety and Depression
Anxiety and depression were assessed using the Hospital Anxiety and Depression Scale. The responses were scored according to the frequency the individual experienced each symptom, with three points assigned for “Yes, definitely,” two for “Yes, sometimes,” one for “No, not much,” and zero for “No, not at all.” Higher scores indicate greater levels of anxiety and depression. The assessed components include sleep quality, a feeling of fright or panic, misery and sadness, anxiety at leaving the house, apathy, palpitations or “butterflies” in the stomach, appetite, scared feelings, feeling life is not worth living, anhedonia, restlessness, irritability, slowing down, and worry. All odd-numbered questions pertain to depression, whereas even-numbered questions pertain to anxiety.17,18)
Knee Osteoarthritis Injury and Outcome Score
At each review, the KOOS questionnaire was administered. The KOOS was chosen as the outcome variable because it is a freely available validated measure,19) comparable to the Western Ontario and McMaster Universities Arthritis Index (WOMAC).20) The KOOS consists of five subscales: symptoms, pain, ADL, function, sports and recreational activities, and quality of life. Responses were first assigned values from zero to four, indicating “never” to “always,” respectively. Domain scores were obtained by summing the scores of individual items. The percentage score was calculated by dividing the sum score by the maximum possible total score and multiplying it by 100%. The mean KOOS score was then calculated as the sum of the percentage scores for each domain divided by the number of domains. A higher percentage score indicated a lower severity of knee OA. The KOOS-symptoms section contained seven questions, the KOOS-pain section contained nine questions, the KOOS-ADL section had 17 questions, the KOOS-sports section had five questions, and the KOOS-quality of life section had four questions. The KOOS was published in 1998, based on the WOMAC, and is self-administered.19)
Participants were included if they completed the KOOS during at least two visits. For all participants, the KOOS scores from the first and last visit were considered the baseline and follow-up scores, respectively. The presence of worsening OA was determined using an arbitrary cutoff of 5%, considering slight fluctuations in scores between visits.
Statistical Analysis
Data were analyzed using IBM SPSS Statistics for Windows, version 28.0 (IBM Corp., Armonk, NY, USA). Summary statistics are presented in comparison tables containing the means and standard deviations for continuous variables and frequencies and percentages for categorical variables. We performed statistical comparisons using the Student independent t-test for continuous data and the chi-square test for categorical data. Considering the limited number of patients who experienced worsening knee OA, adjustments were made only for social networks in both anxiety and depression, using logistic regression analysis to determine potential mediating effects.
RESULTS
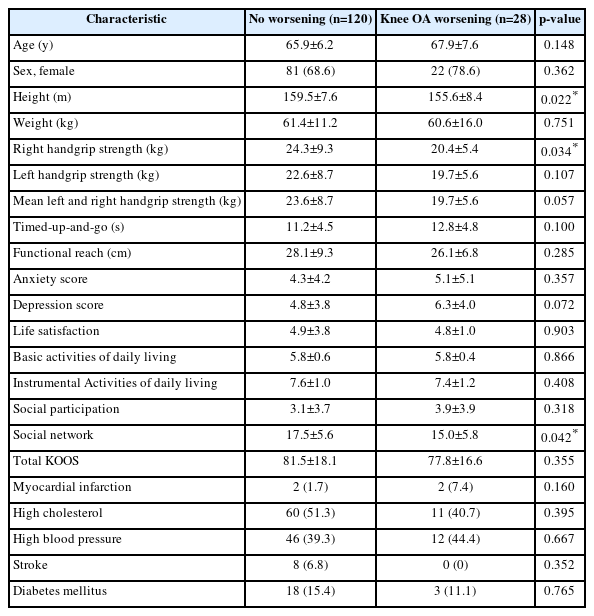
The PISA study recruited a total of 230 patients between 2015 and 2019. The maximum, mean, and median follow-up periods were 48 months, 29.23 months, and 21 months, respectively. Among the 230 participants, 157 completed two visits, 119 completed three visits, and 100 participants attended all four assessments. Of the 148 participants who underwent at least two KOOS measurements, 28 (18.9%) demonstrated knee OA worsening. The basic characteristics of the participants according to worsening symptoms, are summarized in Table 1. Patients with worsening knee OA had significantly lower standing height, right handgrip strength, and Lubben Social Network Scale scores than those without worsening OA. No other basic characteristics differed significantly between patients who demonstrated worsening knee OA symptoms as measured by the KOOS.
We evaluated the factors that predicted the worsening of knee OA using binary logistic regression. Table 2 shows the unadjusted odds ratios for age, sex, height, right handgrip strength, depression, and social network scale. We defined statistically significant factors as those with 95% confidence intervals that did not exceed unity. Univariate analysis revealed a significant association between worsening knee OA and social networking. While the association between depression and worsening knee OA was not statistically significant, when depression was included in the multivariate analysis, the association between social networks and the worsening of knee OA was attenuated. This indicated that depression mediated the effects of social networks on the worsening of knee OA (Table 2). A similar analysis repeated for anxiety (Table 3) showed that the effects of social networks on the worsening of knee OA were mediated by anxiety.
DISCUSSION
Our findings suggest that worsening knee OA is associated with a reduced social network at baseline. However, the relationship between worsening knee OA and social networks was accounted for by depression and anxiety at baseline. A temporal relationship may exist between social networks and knee OA progression, as the worsening of knee OA is a longitudinal measure.
The progression of knee OA has traditionally been assessed radiographically using the Kellgren–Lawrence classification. However, these changes did not correlate with symptoms, indicating that structural changes, rather than radio-opacity, do not necessarily correspond to symptoms.21) Magnetic resonance imaging (MRI) has been suggested as a preferable imaging modality for assessing the severity of knee OA; however, this method is resource-intensive and limited in terms of accessibility, and disagreement remains regarding the clinical significance of certain MRI findings.22) Hence, we used a functional measure, the KOOS, to determine the progression of knee OA in our study.
The relationship between lower standing height and an increased risk of worsening OA has not been previously reported. However, genome-wide sequencing has identified multiple loci associated with knee OA23); some of the identified loci are associated with height, although the direction of the association remains unclear.24) The relationship between height and knee OA is confounded by differences in age and sex and probably by female predominance and occupational association with knee OA.25)
Worsening knee OA symptoms were significantly associated with weaker right handgrip strength. Handgrip strength has not previously been evaluated in the limited studies addressing the progression of OA despite findings that physical therapy is beneficial to patients with knee OA.26) The OA presence may precede the development of muscle wasting or sarcopenia. However, factors predisposing patients to reduced handgrip strength, such as depression and noncommunicable disorders, may also predispose patients to worsening knee OA.
Previous studies have established the association between knee OA and social isolation.27) The present study additionally identified an association between OA worsening and reduced social network, as measured using Lubben six-item Social Network Scale. The relationship between OA worsening and social networks was accounted for by differences in depression and anxiety, suggesting that the deterioration in knee OA symptoms is mediated by psychological issues. Low social support is associated with depression.28) This association has also been observed in the Netherlands29) and Malaysia.30) Previous studies have also reported an association between lower social support and grip strength.32) Social networking also mediates the effects of negative life events on the development of depression in older adults.33) Yamashita et al.34) found that the combination of social networks and financial incentives promoted physical activity more than financial incentives alone. Moreover, the positive association of smaller social networks with metabolic syndrome could be partially explained by physical inactivity.35) Even online social networking shows this effect independent of physical meetings.36)
Fonseca-Rodrigues et al.37) reported a positive correlation between pain measured using the WOMAC, anxiety, and depression in their cross-sectional study. They also found that arthritis led to depressive symptoms.6) However, the presence of depression at baseline was not associated with the progression of knee OA, suggesting that depression is a consequence of knee OA rather than a contributory factor to its progression. These findings highlight the importance of evaluating these relationships in longitudinal studies. Nevertheless, depression also mediated the relationship between social networking and OA worsening, indicating that depression may be a potentially modifiable risk factor for the deleterious effects of social networks and the worsening of OA. However, this requires further evaluation in subsequent interventional studies.
Among the limitations of this study, the arbitrary cutoff of a 5% reduction in KOOS adopted to define the worsening of knee OA symptoms may not represent a clinically significant difference and requires further evaluation. While the high dropout rates recorded in this study were comparable to those of similar studies, such as the Framingham Osteoarthritis Study, in which only 60.4% of participants underwent a follow-up assessment,38) the sample size within this project was limited by a large-scale funding cut that occurred 1 year after study commencement, leading to the cessation of recruitment in favor of serial follow-up with the intention of employing the findings on recruitment and follow-up rates as a pilot cohort for future OA studies. As a result, our ability to statistically adjust for confounders was limited by the low absolute number of individuals with worsening OA. Additionally, knee radiographs were unavailable to all participants due to radiation protection and consent issues, as X-rays were taken based on clinical indications. Handgrip strength measurements were obtained in favor of quadriceps strength owing to the unavailability of specialist equipment at our center, and acquiring it was time-consuming.39) The use of mean rather than maximum handgrip strength accounted for fatiguability.
Nevertheless, the role of psychosocial determinants of health in determining the progression of knee OA evaluated in this study will contribute to future larger prospective and intervention studies. Whether social networks can be modified through psychological and physical interventions, and if this, in turn, will retard the progression of knee OA, must be established.
In conclusion, social network in individuals aged ≥65 years was associated with the subsequent worsening of knee OA, as determined using the KOOS. However, this was accounted for by differences in depression scores, suggesting that psychological interventions may be indicated for the improvement of social networks in older adults, which, in turn, could lead to the prevention of OA progression by enhancing social networks. Interventions to enhance social networks should be considered as part of the non-pharmacological management of patients complaining of worsening knee OA symptoms. Our findings will optimize power calculations and design of future larger prospective studies.
Acknowledgements
The authors would like the acknowledge the hard work of our research assistants Dr Amir Syafwat, Dr Lynell Tong, Dr Yu Deying, and Dr Gerald Loh. We would also like to acknowledge the cooperation and patience of the subjects who willingly and voluntarily participated in the PISA cohort.
Notes
CONFLICT OF INTEREST
The researchers claim no conflicts of interest.
FUNDING
This study was made possible the University Malaya Grand Challenge Fund (Grant No. GC002A-14HTM).
AUTHOR CONTRIBUTIONS
Conceptualization, MPT; Data curation, TGJ, MPT; Funding acquisition, MPT; Investigation and Methodology, SCHL, JLMY, TYW; Supervision, KSH, TGJ, SM; Writing_original draft, TGJ, MPT; Writing_review & editing, KSH, TGJ, SM.