Association between Support after Dementia Diagnosis and Subsequent Decrease in Social Participation
Article information
Dear Editor,
We are writing this letter to accelerate research and discussion on the nature of post-diagnostic support for dementia. Accurate diagnosis of dementia provides a gateway to care and support for people living with dementia and their relatives.1) The reasons for recommending early diagnosis is that cognitive rehabilitation in the milder stages of dementia was suggested to be effective in preventing further impairment.2) National plans focused on early diagnosis of dementia have been initiated in many countries.3) However, the stigma and anxiety associated with diagnosis of dementia without care and support may reduce social participation.4) Also, post-diagnostic support is supposed to moderate the negative impact, but little is known about the delivery and effectiveness of the support. Therefore, we have analyzed the association between post-diagnosis support and subsequent changes in social participation using data from an online survey.
In this survey conducted in December 2021, the respondents were family caregivers of people living at home with early phase dementia and were recruited from a commercial panel.5) Family caregivers of those diagnosed with dementia or mild cognitive impairment for more than three months prior to the survey were included. The outcome variable was the number of categories of social participation that decreased after diagnosis (range 0–3) measured retrospectively. Social participation was categorized into three groups based on Levasseur et al.’s taxonomy6): (1) activities with others around but not including a specific activity with them; (2) activities in collaboration with others to reach a common goal; and (3) activities helping others or contributing to the community. For example, walking, shopping, and eating out were examples of the first group; visiting friends' homes, peer meetings, and group exercises were examples of the second group; and doing volunteer work and involving in community organization activities would be categorized in the third group. In addition, social participation was stratified as people living with dementia alone (unaccompanied) and those with living with family members (accompanied). As an independent variable, the respondents were asked to choose the sources of support they consulted immediately after the diagnosis of dementia. The sources of support included the informal sector (family members/relatives, friends, other people living with dementia), the medical sector (primary care physician, memory clinic, medical center for dementia), and the long-term care sector (care manager, long-term care facility, community general support center). These sources were multiple-response items, and participants selecting each item were compared with those who did not. Adult day service users (n=171) were excluded from the analysis because it was not a social participation that was focused in this study.
Finally, 355 respondents were included in the analysis. The mean age of care recipients was 77.2±12.0 years and the mean score of the Dementia Assessment Sheet for Community-based Integrated Care System 8-item (DASC-8)7) was 12.8±2.7. Majority of them (n=309; 87.0%) lived with their family members and 197 participants (55.5%) had a level of care need certification. For the respondents of family caregivers, the mean age was 50.0±12.9 years. Of the respondents, 161 (45.4%) were children of the participants, 63 (17.7%) were spouses, 120 (59.7%) lived with the participants.
Primary care doctors were the most common post-diagnosis source of support (35.8%), followed by family members/relatives (20.0%) and care managers (15.2%). Moreover, 93 participants (14.6%) did not receive any support. After diagnosis, unaccompanied social participation decreased by 0.95±1.11, while accompanied social participation decreased by 0.78±1.06.
Fig. 1 presents a summary of linear regression analyses with the source of support as the independent variable, the decreased number of social participations as the dependent variable, and age, sex, DASC-8 score, living arrangement, and care needs level as the adjusted variables. Positive regression coefficients indicate a greater decrease in social participation. Support from the informal sector tended to be associated with a decrease in social participation, while support from the medical sector resulted in an opposite trend. In particular, support from friends was significantly associated with greater decrease in social participation (unaccompanied: β=0.561, p=0.015). Support from memory clinic (accompanied: β=-0.417, p=0.038) and dementia medical centers was associated with a smaller decrease (unaccompanied: β=-0.406, p=0.096). Support from care managers was associated with decreased social participation (unaccompanied: β=0.346, p=0.057). Absence of support was not significantly associated with changes in social participation.
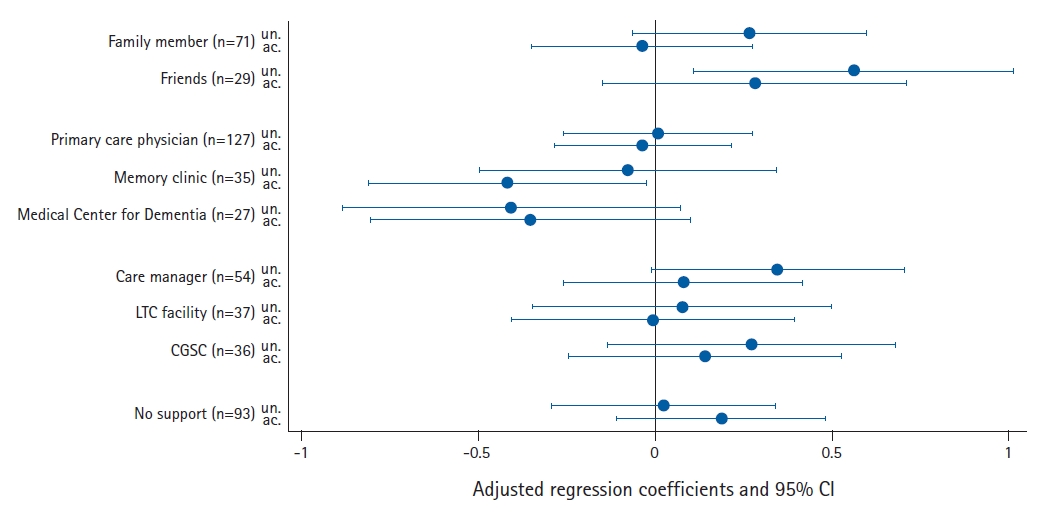
Decreased number of social participations after dementia diagnosis by source of support. LTC, long-term care; CGSC, community general support center; un., unaccompanied; ac., accompanied; CI, confidence interval. Adjusted for age, sex, ling arrangement, months from diagnosis, DASC8 (Dementia Assessment Sheet for Community-based Integrated Care System 8-item) score, care needs level.
Although the present survey is limited by its retrospective nature and small sample size, the implications of the findings are important. The study suggested that social participation decrease depends on the source of support rather than its presence or absence of support. Support from the medical sector, especially memory clinic and Medical Centers for Dementia, had a protective effect against a decline in social participation. It is specified that Medical Centers for Dementia are to be staffed by professionals, including mental health social workers,8) and a previous study reported that 72.6% of the centers offered post-consultation support and 21.5% offered peer support.9) This study suggested the importance of assigning personnel to provide post-diagnostic support to medical institutions that play a central role in dementia in the community.
The association between support from friends and decreased social participation might be due to negative or overprotective attitudes toward social participation of people with dementia. Stigma and misinformation on dementia among the general public have been extensively reported.10) Although support from care managers was common, it was associated with a decrease in social participation. Participants supported by care managers may have already had problems related to social participation and sought support for access to long-term care insurance services.11) In addition, unaccompanied social participation tended to be affected more by support than accompanied participation.
Future research should investigate the kind of support received by people diagnosed with dementia. The present survey did not identify the detailed nature of this support. Even if unintentional, an overprotectiveness implies restrictions on the activities of people with dementia. Improving the quality of post-diagnostic support will contribute to a better living with dementia.
Notes
CONFLICT OF INTEREST
The authors claim no conflicts of interest.
FUNDING
None.
AUTHOR CONTRIBUTIONS
Conceptualization: STsuda, STakehara, TY, SH; Formal analysis: HM, STsuda; Funding acquisition: SH; Supervision: SH, STsuda; Writing-original draft: HM; Writing-review & editing: HM, STsuda, STakehara, TY, SH.
