The Effect of Neuromuscular Blockade Reversal Agents on Postoperative Pulmonary Complications in Patients undergoing Femur Fracture Repair Surgery: A Retrospective Observational Study
Article information
Abstract
Background
Femoral fracture repair surgery under general anesthesia is associated with postoperative pulmonary complications (PPCs). However, information on PPCs caused by residual neuromuscular blockade following perioperative use of neuromuscular blockers is limited. This study aimed to identify the differences in the incidence of PPCs according to the type of neuromuscular blockade reversal agent used in femoral fracture repair surgery, as well as the risk factors for PPCs.
Methods
We retrospectively analyzed the electronic medical records of 604 patients aged >18 years who underwent general anesthesia for femoral fracture repair surgery at a single university hospital between March 2017 and March 2022. Patients in whom sugammadex or anticholinesterase was used to reverse the neuromuscular block were subjected to propensity score matching. Multivariate logistic regression analysis was performed to identify risk factors for PPCs.
Results
Among the 604 patients, 108 were matched in each group. The incidence rates of PPCs overall and in the anticholinesterase and sugammadex groups were 7.0%, 8.3%, and 5.6%, respectively, with no significant differences between the groups. Older age, higher ASA (American Society of Anesthesiologists) physical status, and lower preoperative oxygen saturation were risk factors, whereas emergency surgery was a preventive factor.
Conclusions
Our results demonstrated that the incidence of PPC did not differ significantly between sugammadex and anticholinesterase in patients undergoing femur fracture repair under general anesthesia. Identifying the risk factors and confirming complete recovery from neuromuscular blockade might be more important.
INTRODUCTION
Femur fracture repair surgeries have an increased risk of postoperative pulmonary complications (PPCs), which occur in 4.1%–40% of cases, depending on the definition of PPCs.1,2) Although the overall mortality rates when surgery is performed under general or spinal anesthesia are similar, spinal anesthesia is preferred, given the stability of respiratory function postoperatively.3,4) However, in situations where spinal anesthesia cannot be performed, such as coagulopathy, puncture site infection, or uncooperative patients, general anesthesia is a main anesthetic method used in femoral fracture surgery. Therefore, it is important to understand the incidence of PPCs and related risk factors during general anesthesia for femoral fracture surgery.5,6)
One of the most important elements of general anesthesia is the use of neuromuscular blockers. A neuromuscular blockade reduces intraoperative movement and facilitates surgery. However, residual neuromuscular blockade is a well-known risk factor for anesthesia-related PPCs.7) Two major drugs contribute to recovery from neuromuscular blockade: anticholinesterase, a competitive inhibitor, and sugammadex, a direct inhibitor. Traditionally, anticholinesterases competitively interfere with neuromuscular blockers. However, they have a ceiling effect that is ineffective above a specific dose, do not reverse deep neuromuscular blockade, and increase PPCs dose-dependently.8)
Sugammadex has also recently been used. It can directly reverse all stages of neuromuscular block, regardless of the depth of the neuromuscular block. However, it is only effective for a specific class of neuromuscular blockers.9) Various studies have compared these two drugs for residual neuromuscular block and PPCs, but not for femoral fracture repair surgery, which has a high incidence of PPCs.10,11) Therefore, the present study aimed to identify the differences in the incidence of PPCs according to the type of neuromuscular blockade reversal agent (anticholinesterase or sugammadex) (primary aim) and identify the risk factors for PPCs (secondary aim) in patients undergoing general anesthesia for femur fracture repair surgery.
MATERIALS AND METHODS
Study Design and Populations
This retrospective observational study was conducted in accordance with the 2013 revisions of the Declaration of Helsinki, was approved by the Institutional Review Board of Konyang University Hospital (No. KYUH 2022-04-005), and was registered with the Korea Clinical Research Information Service. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology reporting guidelines. The requirement for informed consent was waived due to the retrospective nature of the study. Also this study complied the ethical guidelines for authorship and publishing in the Annals of Geriatric Medicine and Research.12)
We retrospectively reviewed the medical records of patients aged >18 years who underwent femur fracture repair surgery under general anesthesia between March 2017 and March 2022 at our university hospital. We excluded patients in whom atracurium was used as a neuromuscular blocker, no neuromuscular block reversal agent was used, as well as those who underwent combined operations and with insufficient medical records.
Femoral fractures included the femoral neck, trochanter, shaft, and distal femur. The types of surgeries performed were closed reduction, open reduction, bipolar hemiarthroplasty, and total hip replacement.
Perioperative Management
The patients arrived in the operating room without premedication and were monitored using electrocardiography, noninvasive blood pressure, pulse oximetry, neuromuscular monitoring with acceleromyography or electromyography, and baseline body temperature. All medications used during anesthesia, including induction and maintenance agents for anesthesia, neuromuscular blocking agents, and hypotensive agents or vasopressors, were selected at the anesthesiologist’s discretion according to each patient’s condition.
Postoperatively, the neuromuscular blockade was reversed with an anticholinesterase or sugammadex at the anesthesiologist’s discretion. After emergence from anesthesia, the patients were transferred to the intensive care unit (ICU) or post-anesthetic care unit, depending on their condition. Patients transferred to the post-anesthetic care unit stayed there for at least 40 minutes. Postoperative management was performed for all patients according to the protocol at our institution.
Definition and Variables
The investigation was conducted for up to 7 days postoperatively, according to the following definitions. The investigator checked for the presence of complications based on the records of the included patients. Complications were diagnosed postoperatively according to the Korean Standard Classification of Diseases. PPCs were defined as a composite of respiratory diagnoses that shared common pathophysiological mechanisms, including atelectasis, pneumonia, acute respiratory distress syndrome, and pulmonary aspiration within 7 days postoperatively. Atelectasis was detected by computed tomography or chest radiography, and pneumonia was diagnosed using the US Centers for Disease Control and Prevention criteria. Acute respiratory distress syndrome was diagnosed using the Berlin consensus definition, and pulmonary aspiration was diagnosed with a clear clinical history and radiological evidence.13) The length of hospital stay was defined as the period from admission to discharge. Major adverse cardiac events included composites of myocardial infarction, stroke, heart transplantation, heart failure, other ischemic cardiovascular events, and death.14) Death was defined as in-hospital death.
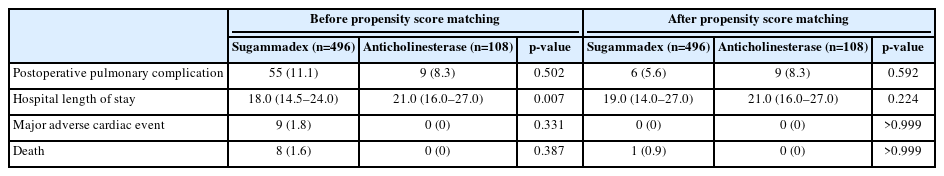
The following variables were collected from the electronic medical records: demographic data; preoperative status and history; preoperative laboratory findings; intraoperative data; and postoperative outcomes such as PPCs, length of hospital stay, major adverse cardiac events, and deaths (Tables 1, 2).
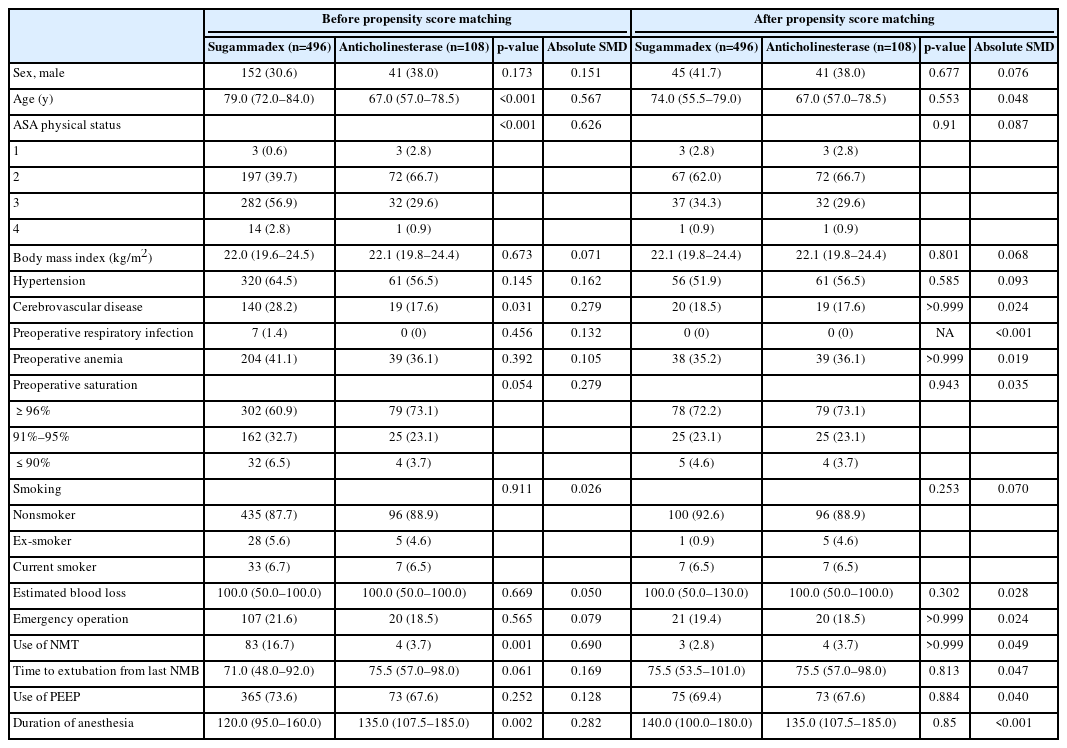
Perioperative data before and after propensity score matching between cholinesterase inhibitor and sugammadex
The primary outcome was the incidence of PPCs according to the type of neuromuscular blockade reversal agent used. The secondary outcome was the risk factor for PPCs in patients who underwent femur fracture repair surgery under general anesthesia.
Statistical Analyses
To determine the incidence of PPCs, we divided the groups according to the neuromuscular blockade reversal agent used (sugammadex or anticholinesterase). All demographic and perioperative data were compared between groups before and after propensity score matching. Propensity score matching was performed using the nearest-neighbor method with a 0.2 caliper width and a 1:1 ratio. The following variables were used: age, sex, American Society of Anesthesiologists physical status (ASA PS), comorbidities, hypertension history, cerebrovascular disease history, preoperative respiratory infection, preoperative anemia, preoperative peripheral capillary oxygen saturation (SpO2), smoking history, estimated blood loss, emergency operation, use of neuromuscular monitoring, time to extubation from the last neuromuscular blocking agent injection, use of positive end-expiratory pressure, and duration of anesthesia.
An absolute standardized mean difference (SMD) <0.1 indicated that both groups were well-balanced.15) Student t-test or Mann–Whitney U test was used for continuous variables after assessing the data distribution using the Kolmogorov–Smirnov test. The χ2 test for trends (linear-by-linear association) or Fisher exact test was used to analyze categorical variables. In these analyses, a two-sided p<0.05 was considered significant.
To identify variables associated with PPCs, univariate and multivariate logistic regression analyses were conducted using unmatched and matched data, respectively. The patients were divided into groups based on the occurrence of PPCs. Multivariate logistic regression analysis using backward selection included the variables with p<0.2 between the two groups (PPCs and no PPCs) in the univariate analysis to identify the independent risk factors of PPCs. The analysis was performed using unmatched and matched data. All statistical analyses were performed using IBM SPSS Statistics for Windows, version 27.0 (IBM Corp, Armonk, NY, USA) and R 3.4.4 (www.r-project.org).
RESULTS
Among 637 patients aged >18 years who underwent femoral fracture repair surgery under general anesthesia, 33 were excluded because of the use of atracurium, requirement for intubation after surgery, or incomplete data. Thus, the analysis included 604 patients (108 in the anticholinesterase group and 496 in the sugammadex group). After propensity score matching, 108 patients in each group were matched (Fig. 1) and all covariates were balanced (Fig. 2). Perioperative data before and after propensity score matching are shown in Table 1. The absolute SMD values of all variables were <0.1 after propensity score matching.
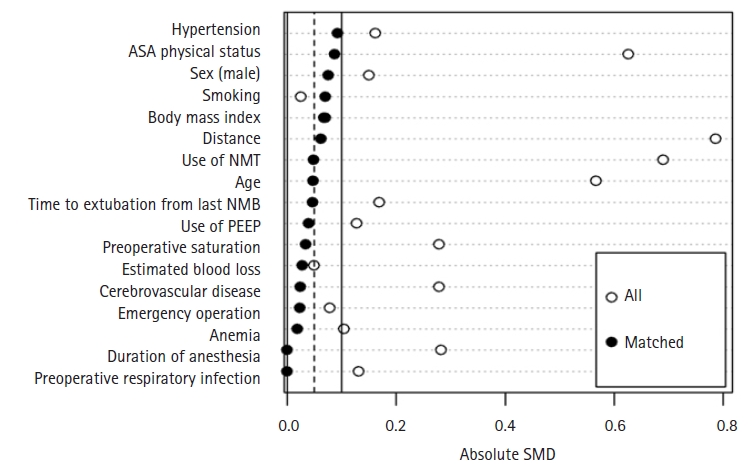
Love plot of absolute standardized mean difference (SMD) before and after propensity score matching. ASA, American Society of Anesthesiologists; NMT, neuromuscular monitoring; NMB, neuromuscular blockade; PEEP, positive end-expiratory pressure.
The postoperative outcomes are presented in Table 2. The overall incidence rates of PPCs before and after matching were 10.6% and 7.0%, respectively. The incidence rates of PPCs in the matched data were 8.3% and 5.6% in the anticholinesterase and sugammadex groups, respectively, with no significant difference between the groups. The median (interquartile range) length of hospital stay was 21 (16–27) days and 19 (14–27) days in the anticholinesterase and sugammadex groups, respectively. Neither group experienced major adverse cardiac events in matched data. One patient died in the sugammadex group.
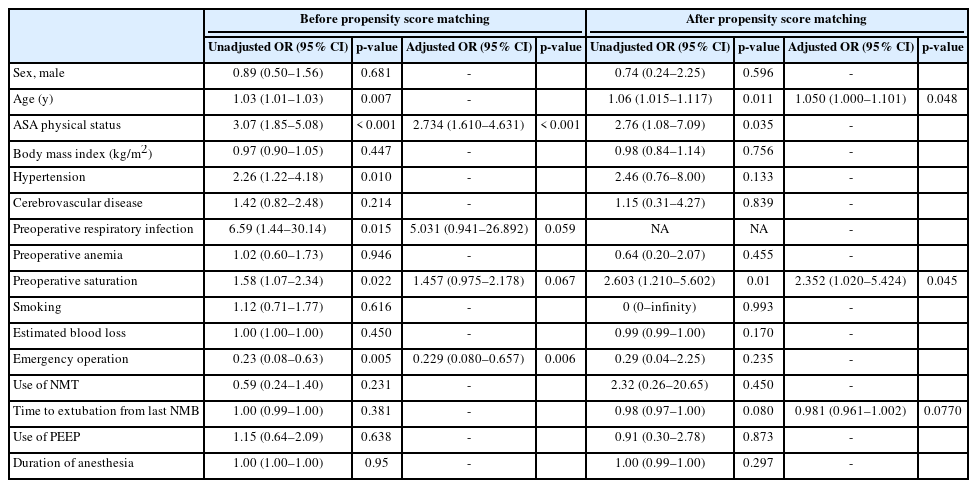
The perioperative data and results of the regression analysis according to the occurrence of PPCs before and after propensity score matching are presented in Table 3 (univariate analysis) and Table 4 (odds ratio [OR] of univariate and multivariate analyses). In the unmatched data, the variables with p<0.2 were age, ASA PS, history of hypertension, preoperative saturation, smoking, and emergency operation. In the matched data, the variables with p<0.2 were age, ASA PS, preoperative saturation, estimated blood loss, and time to extubation from the last neuromuscular blocker.

Perioperative data before and after propensity score matching according to the occurrence of postoperative pulmonary complications
In the unmatched data, a higher ASA PS grade was an independent risk factor for PPCs in femur fractures (adjusted OR=2.734; 95% confidence interval [CI], 1.61–4.631; p<0.001), and emergency surgery was a preventive factor (adjusted OR=0.229; 95% CI, 0.080–0.657; p<0.006). In the matched data, age (adjusted OR=1.050; 95% CI, 1.000–1.101; p=0.048) and preoperative saturation (adjusted OR=2.352; 95% CI, 1.020–5.424; p=0.045) were independent risk factors for PPCs (Table 4).
DISCUSSION
Femur fractures, whose risk factors are old age and osteoporosis, can be corrected surgically. The postoperative complications include acute respiratory distress syndrome, fat embolism, and pneumonia caused by prolonged bed rest.16,17) These complications are reduced through early mobilization, thereby reducing related morbidity and mortality by decreasing the ICU and hospital lengths of stay.18,19) Various surgeries have shown differences in the incidence of PPCs according to the type of neuromuscular blockade reversal agent used.10,11) However, we observed no difference in the incidence of PPCs between sugammadex and anticholinesterase in femur fracture surgery under general anesthesia.
General anesthesia is an important method used in femur fracture repair surgeries when regional anesthesia cannot be administered. Neuromuscular blockers are essential drugs used during general anesthesia. They facilitate surgery by preventing intraoperative movement. However, they may increase the risk of PPCs due to residual neuromuscular block, which may affect postoperative management. In femur fractures, a representative long bone fracture, immobility caused by the fracture increases the risk of pulmonary embolism due to deep vein thrombosis. It can cause fatal pulmonary complications such as fat embolism syndrome.20) In particular, a high proportion of older patients experience femur fractures, and the incidence of residual neuromuscular block in older adults is approximately twice that in younger patients.21)
The previously reported incidence rates of PPCs were 31% in several types of surgeries and 40% in patients with femur fractures.2,10,11) However, the incidence in our study was 7%, which is slightly different from that in previous studies. This difference might be due to the retrospective nature of the study; additionally, underestimation was possible due to insufficient reporting and poor investigation compared to prospective studies. Additionally, unlike previous studies on PPCs in femur fracture surgeries that only included older adults, this study included all adults. The incidence might be lower in all adults than in older people.22,23) In our data, the incidence was 12% in patients aged >65 years.
The use of sugammadex reduces PPCs in older patients undergoing femur fracture repair surgery under general anesthesia.24) In our study, the incidence of PPCs did not significantly differ between both types of reversal agents used in our study. However, the lower incidence with sugammadex is consistent with the results of other studies.10,11) The reasons why the incidence of PPCs did not differ significantly between the reversal agents in our study are as follows. First, femoral fracture repair surgery is associated with a high risk of PPCs owing to the high proportion of older people and the risk of embolism. Second, the tendency to preferentially consider sugammadex for high-risk patients or those expected to have PPCs upon emergence from anesthesia could have affected the results. In addition, although our retrospective findings confirmed the relevance of PPCs related to the type of neuromuscular block reversal agent, a causal relationship could not be confirmed, and the results may have been affected by various uncontrolled influencing factors.
Some variables identified as risk factors in this study, including higher ASA PS, higher age, and lower preoperative saturation, were also representative risk factors for PPCs in previous studies.25-27) In particular, the latter two are meaningful components of the Assess Respiratory Risk in Surgical Patients in Catalonia (ARISCAT) score, the only validated method for scoring PPCs risk factors. Therefore, efforts to identify risk factors using various methods, such as prospective or large-scale studies, are necessary.25)
In addition, unlike previous studies, we identified emergency surgery as a preventive factor.25,26) In our hospital, we aim to perform femur fracture surgeries as emergency surgeries for patients with no specific contraindications. This is probably related to the fact that performing surgery as soon as possible reduces mortality; thus, a quick operation may have affected PPCs.17) Moreover, it is easier to perform emergency surgery in patients without comorbidities than for those with multiple comorbidities owing to cooperation with other departments. However, as the time from injury to surgery was not recorded in this study, it was difficult to confirm this correlation.
The limitations of this study are as follows. First, as this was a retrospective study, it included many uncontrolled factors, which made it difficult to confirm a causal relationship. For PPCs in which preoperative lung status and medical history are important, the results of this study may have been influenced by several factors. However, as it is difficult to conduct a well-controlled prospective study because most patients with femoral fractures are in poor condition or are older individuals, we considered it sufficient to confirm its relevance. Second, as this was a single-center study, group bias was possible. A multicenter or big data study is required to confirm the overall effects of PPCs in patients with femoral fractures undergoing general anesthesia. Finally, the surgical site is an important risk factor for PPC. We included all types of femoral fracture repair surgeries performed in our hospital and did not analyze them by type. However, based on previous studies evaluating the risk factors of PPC, a more detailed classification of surgical types, such as closed reduction, open reduction, bipolar hemiarthroplasty, and total hip replacement, would not have significantly affected our results.25,28)
In conclusion, we observed no significant difference in PPCs according to the type of neuromuscular block reversal agent used in patients undergoing femoral fracture repair surgery under general anesthesia. However, the relationship between PPCs and the neuromuscular blockade reversal agents remains unclear. It is important to thoroughly determine the patient’s condition before surgery and to properly evaluate the patient’s risk according to the risk factors identified in this study.
Notes
CONFLICT OF INTEREST
The researchers claim no conflicts of interest.
FUNDING
None.
AUTHOR CONTRIBUTIONS
Conceptualization, TYS; Data curation, SAC, JHK, CKC; Investigation, SAC, TYS, CKC; Methodology, SAC, TYS; Supervision, TYS; Writing–original draft, SAC, SSL; Writing–review & editing, SAC, TYS.