The Mediating Role of Social Participation in Motoric Cognitive Risk and its Relation to Depression and Loneliness in Older Adults
Article information
Abstract
Background
Motoric cognitive risk syndrome (MCR) reduces the quality of life, independence, and social interaction in older adults. Social participation is a potentially modifiable factor that benefits cognitive and mental health. This study explored the mediating roles of social participation between MCR and depression and between MCR and loneliness.
Methods
We performed a secondary analysis of data from the 2015–2016 National Social Life, Health, and Aging Project. Slow gait speed and cognitive decline were used to assess MCR. Mediation analysis was applied to two models, both of which used MCR as an exposure and social participation as a mediator. The outcomes were depression and loneliness for each model, respectively.
Results
Among 1,697 older adults, 196 (11.6%) had MCR. The mediating role of social participation was statistically significant in both models. The indirect effect (β=0.267, p=0.001) of MCR on depression through social participation comprised 11.97% of the total effect (β=2.231, p<0.001). The indirect effect (β=0.098, p=0.001) of MCR on loneliness through social participation was 19.48% of the total effect (β=0.503, p<0.001).
Conclusion
Interventions to increase social participation may reduce depression and loneliness of older adults with MCR.
INTRODUCTION
Motoric cognitive risk syndrome (MCR) is characterized by cognitive impairment, slow gait speed, and age >65 years.1) MCR can increase the risk of adverse outcomes such as falls and dementia2) and may result in diminished quality of life, dependent daily living, and reduced social interaction.3) The prevalence of MCR is approximately 10% but varies by region and population.4,5) Older adults with MCR experience not only negative physical consequences but also mental health issues. A large cross-sectional study reported that anxiety-depressive disorder and depression were associated with MCR.6) Additionally, MCR has been linked to loneliness.7) MCR and mental health problems are related; therefore, it is vital to identify their contributing factors.
Depression is a common symptom in older adults with MCR.8) Untreated depression can progress to dementia.9) Moreover, social participation is related to depression in older adults. Poverty or a lack of social relations or integration can lead to depression.10) In contrast, older adults who participate in social activities frequently report fewer depressive feelings.11) An increase in depression among older adults is closely related to a decrease in social participation due to aging.12) These findings support the notion that social participation is essential for preventing depression. However, it remains unclear whether the relationship between social participation and depression is the same among older adults with MCR.
Social participation can be defined as individuals engaging in interactions within their community or society through social activities.13) Previous studies reported negative associations between age and social network size9) and between cognitive impairment and social participation.14) Similarly, social participation may be lacking in older adults with MCR.15) Moreover, a lack of social engagement negatively affects individuals with depression.16)
Loneliness is a common interpersonal experience in the subjective appraisal of the extent of social relationships.17,18) Loneliness negatively impacts physical and mental health, well-being, and mortality.19,20) In their analysis of 140,000 older adults from 30 countries, Chawla et al.21) reported a pooled prevalence of loneliness among older adults of 25.9%. Previous studies showed that older adults who frequently participate in social activities are less likely to feel lonely and that an increase in loneliness among older adults is closely related to a decrease in social participation due to aging.22,23)
MCR symptoms such as cognitive impairment, physical weakness, and decreased mental health create significant challenges for patients, families, healthcare professionals, and the government.24) Therefore, exploring the factors that may contribute to depression and loneliness in individuals with MCR is crucial. Understanding the complex associations between MCR, depression, and loneliness by examining the influence of social participation could inform the development of practical interventions to help slow or prevent the transition to dementia. To our knowledge, no previous studies have explored the relationship between MCR and depression or loneliness mediated by social participation. Therefore, this study investigated the mediating effect of social participation on the relationships among MCR, depression, and loneliness.
MATERIALS AND METHODS
1. Study Data and Participants
We retrieved data on 4,377 older adults from the 2015–2016 National Social Life, Health, and Aging Project (NSHAP) (round 3). The NSHAP collects health information on community-dwelling older American adults, including their physical health, cognitive function, social interaction, and emotions. This national survey provides information for developing policies and understanding the aging population. The inclusion criteria for this study were: age 65 years or older and no dementia. The protocol of this secondary data analysis study was approved by the Yonsei University Mirae Campus Institutional Review Board (No. 1041849-202211-SB-199-01) and written informed consent was exempted. Also, this study complied the ethical guidelines for authorship and publishing in the Annals of Geriatric Medicine and Research.25)
2. Study Variables
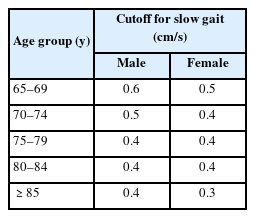
The independent variable (X) was MCR, which was assessed based on the Montreal Cognitive Assessment (MoCA) test score26) and gait speed (m/s). Table 1 presents the gait speed cutoff for defining slow gait in MCR.2) The participants were assigned a code of 1 if they had a MoCA score <26 points and exhibited slow gait speed (m/s), and a code of 0 if their MoCA score was >26 and they did not display slow gait speed. The NSHAP questionnaires include the Survey-Adapted Montreal Cognitive Assessment (MoCA-SA) for assessing cognitive function. The MoCA-SA score was transformed into the MoCA score, as described previously.27) The cutoff score for slow gait speed was set below the average speed score by 1 standard deviation by age and sex.2)
One dependent variable (Y1) was depression, which was measured using the Center for Epidemiological Studies Depression Scale (CESD-11). Each of the 11 items is scored on a 4-point scale (0, rarely or none of the time; 1, sometimes; 2, occasionally; and 3, most of the time). The total score ranges from 0 to 33 points.28) The sum of the scores was used as the dependent variable. Higher CESD-11 scores indicated more severe depressive symptoms.
The other dependent variable (Y2) was loneliness, which was assessed using the University of California Los Angeles Loneliness Scale, version 3 (UCLA). The loneliness variable consisted of three indicators (companion, isolated, and left out). The UCLA scores comprise a 20-item scale (0, never; 1, hardly ever; 2, sometimes; and 3, often).29) The total score ranges from 0 to 9 points. We used the sum of the scores as the loneliness variable.
The mediating variable (M) was social participation. The social participation variable consisted of three domains (attend, social, and volunteer) and was measured using the following three questions: “In the past 12 months, how often did you attend meetings of any organized group?” “In the past 12 months, how often did you get together socially with friends or relatives?” “In the past 12 months, how often have you volunteered to work for religious, charitable, political, health-related, or other organizations?” These were scored on a 7-point Likert scale (0 “never” to 6 “several times a week”). We used the total score of the three questions (ranging from 0 to 18 points) as the mediating variable, with a higher score indicating positive social participation.
3. Statistical Analyses
We performed descriptive analyses to explore the demographic characteristics. We used the independent t-test for continuous variables and the chi-squared test for categorical variables to examine the difference between two groups with and without MCR. Mediation analysis was used to investigate the role of social participation in mediating the relationship between MCR and depression. Baron and Kenny30) proposed a mediation analysis that applies a specific analytic procedure to adequately measure and test our hypotheses. This procedure consists of a three-step regression analysis (X for Y, X for M, and M for Y). However, there is a disadvantage in that the indirect effect is estimated to be low.31) In this study, we checked whether individual pathways were statistically significant in determining the indirect effects. Additionally, this method can only use Sobel's test to examine the significance of the indirect effects. The bootstrapping method has been proposed to replace Sobel's test because it relies on the assumption of a normal distribution.31,32) We also estimated the parameters using the maximum likelihood method with robust standard errors. Therefore, we applied path analysis to estimate the indirect and direct effects of MCR, social participation, and depression. The significance of the indirect and direct coefficients was examined using bootstrapping methods.33) The identification of the outliers in terms of low-speed gait for sensitivity analysis revealed no outliers in the dataset. We used SAS version 9.4 (SAS Institute, Cary, NC, USA) for data preprocessing and descriptive statistics and Mplus version 8 (Los Angeles, CA, USA) for mediation analysis.
RESULTS
The sample size for this study was 1,697 older adults after excluding those with missing values (n=423), those aged <64 years (n=2,116), and those with dementia according to the cutoff MoCA score of 17 points (n=141) (Fig. 1).
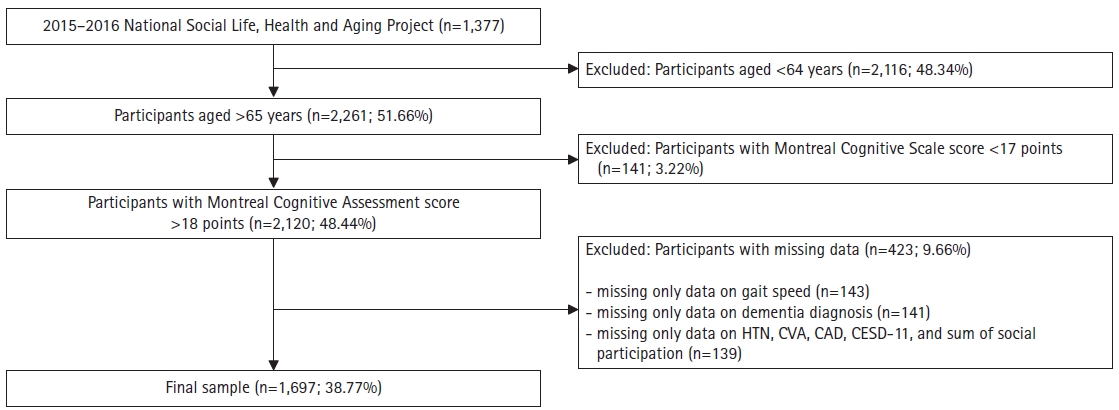
Participant flow diagram. CAD, coronary artery disease; CESD-11, Center for Epidemiologic Studies Depression Scale-11; CVA, cerebrovascular accident; HTN, hypertension.
Table 2 shows the demographic characteristics of the 1,697 participants. The MCR group comprised 196 (11.6%) participants, including 93 (47.4%) men and 103 (52.6%) women. The non-MCR group comprised 1,501 (88.4%) participants, including 695 (46.3%) men and 806 (53.7%) women. Women predominated in both groups. Additionally, 1,046 (61.6%) participants engaged in physical activity each week, 102 (52.0%) of whom were in the MCR group. The average age did not differ significantly between the MCR (74.27±6.39 years) and non-MCR (74.27±7.23 years) groups. However, we observed significant differences between the MCR and non-MCR groups in CESD-11 score (6.75±5.63 vs. 4.52±4.35), ULCA score (3.27±2.39 vs. 2.77±2.14), and gait speed (0.39±0.12 vs. 0.74±0.22 m/s).
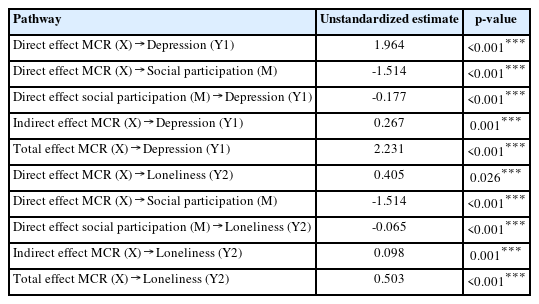
Table 3 and Fig. 2 present the results of the mediation analyses. MCR was significantly associated with depression (β=1.964; 95% confidence interval [CI], 1.151–2.777; p<0.001) and social participation (β=-1.514; 95% CI, -2.159–-0.869; p<0.001). Additionally, social participation and depression were significantly associated (β=0.177; 95% CI, -0.226–-0.128; p<0.001). The indirect and total effects of MCR on the occurrence of depression were 0.267 (95% CI, 0.130–0.404) and 2.231 (95% CI, 1.280–3.181), respectively (Fig. 2A). Therefore, the total effect of our first model of the mediation analysis between non-standardized coefficients consisted of 11.93% indirect effect and 88.03% direct effect. Both were significant (indirect effect, p=0.001; direct effect, p<0.001).
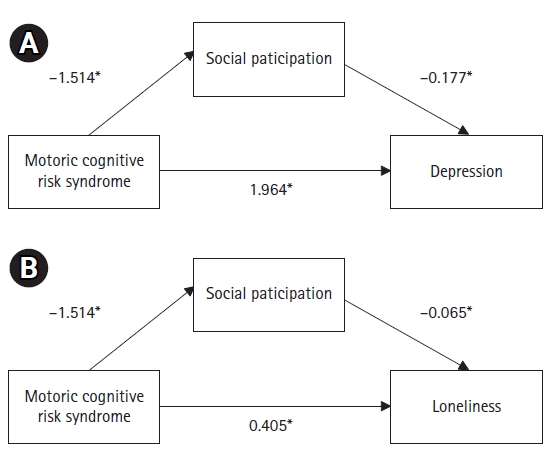
Mediation analysis models. (A) Mediating role of social participation between MCR and depression. (B) Mediating role of social participation between MCR and loneliness. Unstandardized coefficients were presented.
Our analysis showed that the MCR also was significantly associated with loneliness (β=0.405; 95% CI, 0.048–0.762; p=0.026) and social participation (β=-1.514; 95% CI, -2.159–-0.869; p<0.001). Social participation and loneliness were also significantly associated (β=-0.065; 95% CI, -0.089–-0.0.041; p<0.001). The indirect effect of MCR on loneliness was 0.098 (95% CI, 0.041–0.155), and the total effect was 0.503 (95% CI, 0.089–0.917) (Fig. 2B). Therefore, the total effect of the second model of the mediation analysis between MCR and loneliness by social participation was also significant (indirect effect, p=0.001; direct effect, p<0.001), which included both indirect (19.48%) and direct (80.52%) effects.
DISCUSSION
Our findings showed that social participation is mediated the relationship between MCR and two types of mental health indicators (depression and loneliness). MCR directly and indirectly influenced older adults with depression or loneliness by decreasing their social participation. This study aimed to clarify the adverse health outcomes of older adults with MCR whose social networks are reduced due to cognitive decline and reduced gait speed which is significantly impacts their mental health. The association between MCR and social participation was supported by previous studies reporting that MCR is related to emotional (tangible, affectionate feelings) and social support.34) Studies have also shown that social participation facilitates better health among older adults. Our study provides evidence supporting these findings.35) Moreover, we identified the mediating function of social participation between MCR and depression and loneliness.
This study has two major findings. The first was the direct effect of MCR on two types of mental health (i.e., depression and loneliness). These results suggest that declines in gait speed and cognitive function are associated with depression and loneliness. The associations identified in this study align with those of previous studies, supporting the association between MCR and mental health. A Canadian cross-sectional study reported an association between MCR, anxiety, and depression.6) A Chinese 4-year prospective study also reported that depression was related to MCR and required special consideration to reduce dementia following the development of MCR.1) Regarding the association between MCR and loneliness, a Chinese longitudinal study focusing on female older adults demonstrated an association between loneliness and the development of MCR.36) Therefore, the association between MCR and depression/loneliness found in this study can direct clinicians to pay attention to the symptoms of MCR, which may be perceived as a natural aging process.
The second finding is the mediating effect of social participation on the relationship between MCR and mental health (i.e., depression and loneliness). These mediating effects can be explained by the associations of the two sub-factors of MCR (i.e., slow gait speed and cognitive decline) with social participation and the association between social participation and mental health. A study in Singapore including older adults demonstrated that slow gait speed is associated with potential social isolation owing to reduced physical activity and infrequent contact with others.37) Similarly, an aging study conducted on older adults in China suggested that maintaining normal gait speed was associated with higher engagement in social activities and participation, which promoted physical health and walking speed.38) A meta-analysis examining cognitive decline revealed a consistent relationship between social activities and participation.39)
Social participation is associated with mental health outcomes. A Taiwanese longitudinal study over 18 years that explored the trajectory of social activity participation and depression symptoms in older adults showed that continuous participation or the initiation of social activity in old age was significantly related to the reduction of symptoms of depression.11) Previous research has indicated that greater social participation is correlated with reduced loneliness.40) Therefore, our findings regarding the indirect effects of social participation on MCR and mental health align with existing mechanisms and highlight the importance of social participation as a crucial factor related to the mental well-being of older adults with MCR.
Our study has several limitations. We measured social participation using three items: (1) participation in organized group activities, (2) social meetings with family and relatives, and (3) volunteering. This operationalized definition aligns with the concept of social participation in the Occupational Therapy Practice Framework 4, in which social participation is defined as activities that encompass social interaction with family, friends, and community members and promote social interdependence.41) However, we did not assess engagement in leisure activities, a commonly used measure of social participation, as the NSHAP data do not include items related to leisure activities. Second, our study used a cross-sectional design that could not establish causality. Thus, longitudinal studies to examine the causal effect of MCR on each factor (i.e., depression and loneliness) are needed, in addition to developing approaches for the early detection and intervention of MCR.
In conclusion, our study investigated the mediating effect of social participation on the relationship between MCR and depression and MCR with loneliness. The findings revealed the indirect association of social participation as a mediator. Our results showed that increased social participation among older adults with MCR may reduce depression and loneliness. Based on these results, further research is warranted to examine the effectiveness of social participation interventions in decreasing depression and loneliness among older adults with MCR.
Notes
CONFLICT OF INTEREST
The researchers claim no conflicts of interest.
FUNDING
This study was supported by the Ministry of Education of the Republic of Korea and the National Research Foundation of Korea (Grant No. NRF-2021S1A3A2A02096338).
This research was supported by the BK21 FOUR (Fostering Outstanding Universities for Research) funded by the Ministry of Education (MOE) of the Republic of Korea and National Research Foundation of Korea (NRF) (Big data specialized education and research team for cognitive health and social integration of community-dwelling older adults).
AUTHOR CONTRIBUTIONS
Conceptualization, JHP1, JHJ, SB; Data curation, JHP1, JHJ, SB; Methodology, SB, SY, IH; Project administration, JHP1, SB, SP; Supervision, SP, IH, JHP2; Writing-original draft, JHP1, JHJ, SB, SY, AK; Writing-review & editing, JHP1, SP, IH, JHP2.