|
 |
- Search
| Ann Geriatr Med Res > Volume 27(2); 2023 > Article |
|
Abstract
Background
Various functions are involved in prefrailty. However, no studies have examined more relevant functions. Therefore, this study examined the domains of the Kihon Checklist (KCL) associated with prefrailty by comparing them to robustness measures, using the KCL to comprehensively assess life-related functions in community-dwelling older adults.
Methods
The 194 (mean age, 75±6 years) participants were community-dwelling older adults. Their robustness and preferences were assessed using the Japanese Cardiovascular Health Study criteria. Comprehensive life-related functions were assessed using the KCL, and each physical function was measured.
Results
The main KCL characteristics associated with robustness and prefrailty were physical function (odds ratio [OR]=1.83; 95% confidence interval [CI], 1.17–2.88), nutritional status (OR=8.16; 95% CI, 2.96–22.48), and depressed mood (OR=3.46; 95% CI, 1.76–6.79). In particular, older adults had difficulty moving, including climbing stairs and getting up from a chair, which suggested a strong fear of falling. The participants also reported psychological characteristics such as low life fulfillment, a low sense of self-usefulness, and a strong sense of boredom.
Conclusions
Prefrail individuals were characterized by poor physical function and nutritional status, as well as depressive mood. Prefrailty may be prevented or improved by approaches to improve physical function and fear of falling in addition to psychological interventions that encourage activity and a sense of self-usefulness.
Frailty, a risk factor in older adults requiring long-term care,1) is defined as a biological syndrome characterized by a decline in physiological reserves with age.2) Frailty is characterized by reversibility; therefore, early detection and intervention in frail older adults may help restore their vigor.3)
The Cardiovascular Health Study (CHS) criteria are widely used in Europe and the United States.4,5) Japan uses a revised version of the CHS (J-CHS), which comprises five questions. Scores of ≥3 and 1–2 indicated frailty or prefrailty, respectively. A Japanese study of community-dwelling older adults reported a 56.9% prevalence of prefrailty as assessed by the J-CHS; that is, more than half of the population falls under this category.6) Prefrail people are at a higher risk of facing impairments in activities of daily living (ADL) and instrumental activities of daily living (IADL) compared to robust people.7) Additionally, the risk of needing long-term care after 2 years is significantly higher than that in healthy adults.8) Thus, prefrailty in older adults is a significant risk factor that merits as much attention as frailty. Although most studies have focused on high-risk frailty, literature on the various aspects of prefrailty is scarce. To avoid the need for long-term care and extend healthy life expectancy in older adults, interventions must begin from the prefrailty stage to reduce the overall cost of healthcare and shorten the intervention time.
In Japan, the Kihon Checklist (KCL) is widely used to determine the need for long-term care prevention.9) The KCL comprehensively and multidimensionally assesses function in older adults.10) Using this tool, it is easy to ascertain which functions are deteriorating, and which must be targeted for prevention and intervention. As mentioned above, only a limited number of studies have evaluated prefrailty in community-dwelling older adults, and only one study has examined the association between prefrailty and the KCL.11) Furthermore, after the revision of the J-CHS in 2020, no studies have assessed this association according to the revised criteria. Therefore, this study examined and characterized the association between prefrailty, as determined by the revised J-CHS, and comprehensive functioning, as assessed by the KCL. Identifying the KCL domains associated with prefrailty will contribute to focused rehabilitation interventions for improvement from prefrailty to robustness.
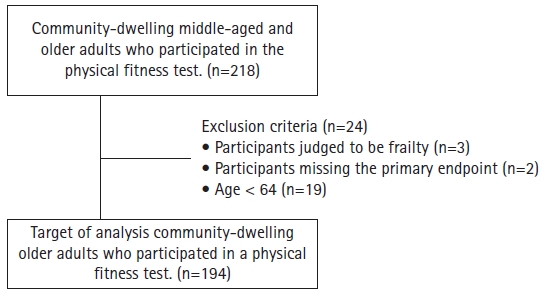
This cross-sectional study included community participants who underwent a physical fitness assessment. Participants were recruited through calls from health promotion class staff and posters. The participants were community-dwelling middle-aged and older adults who visited the measurement site independently. Those who were determined to be frail according to the J-CHS, showed deficiency in the primary endpoints, and were aged ≤64 years were excluded from the study. All participants in the physical fitness evaluation sessions were fully informed of the content and purpose of the study, and their consent and cooperation were obtained after gaining their understanding. Voluntary participation in the study was explained to the participants, and the physical fitness measurements were performed even if they refused to participate without any disadvantages or consequences. The study protocol was approved by the Ethical Review Committee of Nishikyushu University (No. 21VBC35). Also this study complied the ethical guidelines for authorship and publishing in the Annals of Geriatric Medicine and Research.12)
The J-CHS assesses five items: weight loss, muscle weakness, fatigue, decreased walking speed, and decreased physical activity. For weight loss, participants were asked whether they had an unintentional weight loss of ≥2 kg over a 6-month period, with one point added for “yes” responses. Grip strength was measured using a Smedley-type digital grip strength meter (T.K.K. 5401; Takei Scientific Instruments, Niigata, Japan); points were added for grip strengths of <28 and <18 kg in males and females, respectively. Fatigue was assessed by asking the participant whether they had felt tired for any reason in the last 2 weeks; a point was added if the answer was “yes.” To determine the walking speed component, the participants were asked to walk at a normal pace along an 11-m walking path. Their walking speed was calculated for the middle 5 m. A point was added if the walking speed was <1.0 m/s. Physical activity was assessed by two questions: (1) whether the respondents engaged in light exercise or gymnastics and (2) whether they engaged in regular exercise or sports. Points were added if the respondent answered “not even once a week” to either question. Prefrailty was ascertained when one or two of the five items were scored.13)
The KCL is recommended for determining the need for preventive care services and certifying the need for long-term care.14) The KCL is used to assess functions closely related to daily life from multiple perspectives.9) The questionnaire was developed by the Ministry of Health, Labor, and Welfare in Japan and has been used in various countries because of its usefulness.15,16) It contains 25 questions addressing seven life-related domains: IADLs (questions #1–5), physical function (questions #6–10), nutritional status (questions #11–12), oral function (questions #13–15), social isolation (questions #16–17), cognitive function (questions #18–20), and depressive mood (questions #21–25). Each question consists of a “yes” and “no” two-case system, with one point awarded for each applicable answer. The total score for each of these functions was used as a representative value to provide a comprehensive assessment of the functions of older adults. The KCL items are listed in Supplementary Table S1.
Grip strength was measured using a Smedley-type digital grip strength meter (T.K.K. 5401). While standing, the participants were asked to extend their elbow joint, and the proximal interphalangeal joint of the index finger was adjusted to 90°. During the measurements, the examiner ensured that the upper limbs did not touch the lower limbs or trunk. All measurements were taken twice, alternately on the left and right sides, and the total of the left and right sides divided by the body weight was used as the grip strength.
Knee extension strength was measured using a Locomo Scan-II (Model 20691; ALCARE, Tokyo, Japan) lower-limb muscle strength-measuring device with a training function. Locomo Scan was developed based on a training method for quadriceps exercises.17) Muscle force measurement data were sampled at 100 m/s, with minimum and maximum measurements of 1 and 1,500 N, respectively. Since the Locomo Scan uses the quadriceps setting exercise method of measurement, this method may induce less pain compared to the conventional method using a hand-held dynamometer.18) All participants performed isometric knee extension exercises in a long sitting position, and the pressure applied on the Locomo Scan was recorded. The measurements were taken twice, alternately on the left and right sides, with the sum of the left and right sides divided by the body weight used as the knee extensor muscle strength.
The 30-second chair stand test (CS-30) was performed using a chair with a seat height of 40 cm and a digital stopwatch. With their upper limbs crossed in front of their chest, the participants were asked to stand up and sit down repeatedly as fast as possible for 30 seconds, and the number of repetitions was recorded.19) Because the CS-30 is challenging for older adults, only one measurement was taken, taking fatigue into consideration.
Timed up and go (TUG) tests were performed using a digital stopwatch. The participants were instructed to get up from the chair, go to a landmark located 3 m in front of them, and sit down again. The time required for a series of movements was measured. Measurements were taken once for leftward rotation and once for rightward rotation, and the fastest value was used.
The maximum walking speed was measured using a digital stopwatch. The participants were asked to walk 11 m on level ground as quickly as possible. The time required to cover the middle 5 m distance was recorded. The test was performed twice, and the fastest walking speed was used for analysis.
To assess cognitive function, a face-to-face evaluation was conducted using the Mini-Mental State Examination (MMSE). The MMSE is reported to have intra-rater reliability and is widely used worldwide.20) The exam consists of 11 items, in which a higher score on a 30-point scale indicates higher cognitive function and a score ≤23 indicates cognitive impairment.21)
To confirm the characteristics of those participants indicated as prefrail, the sex distribution was compared using the chi-square test; age, height, weight, body mass index (BMI), and physical function were compared using Student t-test; and cognitive function and KCL were compared using the Mann–Whitney U test. Next, a binomial logistic regression analysis was conducted to examine the KCL domains associated with robustness and prefrailty, with robustness and prefrailty as dependent variables and each function of the KCL as an independent variable. Sex and age, which were considered covariates, were adjusted for in Model 2. In addition, the characteristics were analyzed in detail by comparing the percentage of respondents falling under the sub-items of each of the KCL that showed significant associations in the binomial logistic analysis between robustness and prefrailty. For effect size, the t-test was confirmed by Cohen's d, Mann–Whitney U test by r, chi-square test by φ coefficient, and Fisher exact probability test by Cramer's V. Furthermore, as the sample size could not be calculated a priori, power was determined as an a posteriori test. The statistical significance level was set at 5% (p<0.05). IBM SPSS Statistics for Windows, version 27.0 (IBM Corp., Armonk, NY, USA) was used for the analyses.
This study included 218 community-dwelling middle-aged and older adults who participated in community physical fitness sessions between 2019 and 2021. Of these, 24 participants were excluded: those determined to be frail by J-CHS (n=3), those with missing primary endpoints (n=2), and those aged <64 years (n=19). Therefore, the final analysis included 194 participants (mean age of 75±6 years, 74% female) (Fig. 1).
Of the participants, 72% (n=140) and 28% (n=54) were designated as robust and prefrail, respectively. We compared the demographic attributes, physical function, cognitive function, and KCL between these groups to identify the characteristics of participants deemed prefrail. Regarding physical function, robust participants had better grip strength (p=0.002), CS-30 (p=0.007), TUG (p=0.001), and maximum walking speed (p<0.001) than prefrail adults. In addition, robust participants had significantly higher MMSE scores than the prefrail participants (p=0.016). Similarly, in the KCL, the points for physical function (p<0.001), nutritional status (p<0.001), oral function (p=0.005), and depressive mood (p<0.001) were significantly higher in robust adults compared to those who were prefrail. We observed no significant differences in other demographic attributes, physical function, or KCL scores (Table 1).
The KCL domains significantly associated with robustness and prefrailty in this study were physical function (p=0.003; odds ratio [OR]=1.94; 95% confidence interval [CI], 1.26–2.99), nutritional status (p<0.001; OR=7.47; 95% CI, 2.77–20.14), and depressive mood (p<0.001; OR=3.57; 95% CI, 1.84–6.93). After adjusting for gender and age as covariates, the KCL domains of physical function (p=0.009; OR=1.83; 95% CI, 1.17–2.88), nutritional status (p<0.001; OR=8.16; 95% CI, 2.96–22.48), and depressive mood (p<0.001; OR=3.46; 95% CI, 1.76–6.79) were significantly associated with robustness and prefrailty. The same items also showed significant associations in Model 2; the model χ2 test was significant (p<0.001), and the p-value for the Hosmer–Lemeshow test was 0.767. No independent variables had a variance inflation factor (VIF) ≥5 (Table 2, Fig. 2).
We compared the percentages of respondents who fell into the subitems of the KCL domains that showed significant associations with robustness and prefrailty. The results showed significant differences for the following physical functions: “Do you normally climb stairs without using a handrail or wall for support?” (p<0.001), “Do you normally stand up from a chair without any aids?” (p=0.007), and “Do you have a fear of falling while walking?” (p=0.008). We also observed a significant difference in the nutritional status-related question, “Have you lost 2 kg or more in the past 6 months?” (p<0.001). Finally, regarding depressed mood, we observed significant differences for the questions “In the last 2 weeks, did you feel unfulfilled in your daily life?” (p=0.012), “In the last 2 weeks, have you felt difficulty in doing what you could do easily before?” (p<0.001), “In the last 2 weeks, have you ever felt helpless?” (p=0.019), and “In the last 2 weeks, have you ever felt tired for no reason?” (p<0.001) (Table 3).
This study examined the KCL domains associated with robustness and prefrailty. Our results showed associations with physical function, nutritional status, and depressed mood. In particular, prefrail participants showed difficulty climbing stairs and getting up from a chair, and a strong fear of falling. Furthermore, these participants also expressed low life fulfillment, a low sense of self-usefulness, and a strong sense of boredom.
Moreover, 28% of the current study participants belonged to the prefrail category, a rate considerably lower than those previously reported among community-dwelling older adults (42%–45%).22,23) This difference may have occurred because the study participants were already actively engaged in rehabilitation interventions (exercise classes and home exercise programs) to prevent long-term care and to extend their healthy life expectancies. The physical and cognitive functions of the participants in the analysis exceeded the cutoff values for those at risk of important adverse events such as falls.24-26)
We compared the attributes, physical function, cognitive function, and KCL to determine the characteristics of prefrail adults. The results revealed significant differences in grip strength, CS-30, TUG, maximum walking speed, MMSE, and four KCL domains (physical function, nutritional status, oral function, and depressed mood). The J-CHS evaluation items included decreased grip strength and gait speed.13) Therefore, the findings of the current study in terms of significant differences between robust and prefrail individuals in grip strength and maximal walking speed are reasonable. In addition, the differences in KCL physical function likely occurred because prefrailty is mainly associated with a decline in physical function.27,28) Nutritional status is considered a key contributor to the frailty cycle.29) Additionally, poor oral function worsens nutritional status.30) The results of the current study further corroborate these findings and show that prefrail patients tend to have poorer oral function and nutritional status. Furthermore, depressive mood is also reportedly associated with frailty prevalence and progression31); similar characteristics were shown by the prefrail participants in the present study. These results confirm the possibility that the KCL can be used to identify prefrailty.9,32,33)
The results of the binomial logistic regression analysis with robustness and prefrailty as dependent variables showed that physical function, nutritional status, and depressed mood were significantly associated with robustness and prefrailty in Model 2, which was adjusted for sex and age. A previous study examining the characteristics of prefrailty in community-dwelling older adults, as determined by the pre-revised J-CHS using the KCL, reported that physical functioning and depressed mood were characteristics of prefrailty, similar to the results of the present study.11) Physical function in the KCL consists of five items: activities related to mobility such as stair climbing, standing up, walking, history of falls, and fear of falling.34) Frailty is also associated with mobility impairments.35) The present study focused on prefrailty; the relationship between mobility impairment and prefrailty suggests the need to address mobility from the prefrailty stage. In addition, prefrailty in community-dwelling older adults is a major risk factor for falls,36) which further supports the results of the current study and the need to address the risk of falls even in the prefrailty stage. In addition, several studies have reported a relationship between nutritional status and reduced physical function,37,38) consistent with the findings of the current study that worsening nutritional status was associated with decreased physical function and increased fatigue. In addition, a significant relationship was noted between depressive mood and reduced physical functioning. The association between frailty and depression in community-dwelling older adults has been reported39); these individuals are approximately four times more likely to develop frailty,40) which may be attributed to depression leading to reduced activity41) and social frailty.42) Therefore, additional psychological interventions are required during the prefrailty stage.
We also compared the percentages of respondents falling under the sub-items of the KCL associated with prefrailty and robustness. The results revealed that prefrail individuals had greater difficulty climbing stairs and standing than walking. Interestingly, although we observed no significant difference in the history of falls, the fear of falling differed significantly (p=0.008). Older age and a strong fear of falling can be important factors in accelerating frailty by limiting physical activity.43) These characteristics indicate the need to enhance physical activity, focusing specifically on stair climbing and standing movements, to improve mobility-related movement from the prefrailty period. Our results also highlighted the need for an approach to prevent decreased activity due to the fear of falling. Regarding nutritional status, the only significant difference was in the question, “Have you lost 2 kg or more in the last 6 months?” This difference may be related to J-CHS, which contains many similar questions.13) Regarding depressive mood, the results showed that although the participants felt that their lives were relatively enjoyable, they experienced a lack of fulfillment, hesitancy to engage in activities, a low sense of self-usefulness, and a strong sense of fatigue. As individuals with prefrailty have a significant decline in physical function, not unexpectedly, a larger percentage of these individuals answered “yes” to the question “In the last 2 weeks, have you felt difficulty in doing what you could do easily before?” These findings indicate that prefrail older adults have a lower sense of fulfillment in daily life, which was supported by a previous study reporting that mobility was related to feelings of fulfillment in life in older adults.44) This study is limited due to its cross-sectional design, which prevented the identification of causal relationships; however, the results demonstrated that community-dwelling older adults with prefrailty may have a reduced sense of fulfillment in their lives due to impaired mobility. Our results suggest that prefrail older adults need to maintain activity levels and improve their sense of fulfillment in their lives while receiving environmental adjustment and social support in addition to interventions for physical function. Furthermore, decreased self-usefulness is a predictor of disability and mortality,45) and volunteer work and employment activities effectively improve the sense of self-usefulness.46) Thus, rehabilitation interventions aim to increase a sense of self-usefulness. The strength of this study is that it evaluated the functions associated with prefrailty using the KCL, which allowed for the identification of detailed segmented characteristics. This was also the first study to examine the association between the revised J-CHS and KCL.
This study has several limitations. First, the small sample size limits the generalizability of the results. It may also be necessary to collect more frail participants and classify them into three groups (robustness, prefrailty, and frailty). Second, the study population comprised older adults who routinely engaged in long-term care prevention and health promotion. Future studies should include a wider range of participants with longer follow-up periods. Third, because this was a cross-sectional study, it was not possible to establish causal relationships. Therefore, future longitudinal studies should be conducted. Finally, similar items were found in the revised J-CHS, with which prefrailty and robustness were determined in this study, and in the KCL questions. Future studies are needed to verify whether similar results to the present study can be obtained if prefrailty and robustness are determined using other assessment methods that do not have items similar to the KCL.
In conclusion, the results of this study revealed that physical functioning and depressed mood were associated with prefrailty among community-dwelling older adults, as determined by the revised CHS criteria. Furthermore, a detailed analysis of the sub-items showed particular difficulty in climbing stairs and getting up from a chair and a strong fear of falling. In addition to a lack of sense of fulfillment in their lives, the participants also demonstrated an aversion to activities and a low sense of self-usefulness. Furthermore, the results suggested that psychological approaches to reduce the fear of falling, encourage activity, and enhance self-usefulness may be important for improving prefrailty to robustness, in addition to physical function alone. Additional studies are needed to examine whether a multidimensional approach to fear of falling and a psychological approach to depressed mood, can improve physical function and prefrailty.
ACKNOWLEDGMENTS
AUTHOR CONTRIBUTIONS
Conceptualization, TK, HOt, TT; Data curation, TK, HOt, MH, AK, TT; Formal analysis, TK, SS, MM; Investigation, TK, HOt, MH, AK, TT; Methodology, TK, MH, MM; Project administration, SS, MM; Supervision, HOt, TT; Validation, HOk, KF, AS, GH; Writing-original draft, TK; Writing-review & editing, HOk, KF, AS, GH.
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via https://doi.org/10.4235/agmr.23.0019.
Fig. 2.
Logistic regression analysis forest plot (chi-square test <0.001, Hosmer-Lemeshow test 0.767, judgmental success rate 80.9%, covariate of sex and age). IADL, instrumental activities of daily living; OR, odds ratio.

Table 1.
Participants characteristics
| Overall (n=194) | Robustness (n=140) | Prefrailty (n=54) | p-value | Effect size |
95% CI |
Power | ||
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Sex, female | 140 (74) | 107 (76) | 43 (80) | 0.633c) | 0.34 | -0.10 | 0.17 | 0.07 |
| Age (y) | 75±6 | 74±6 | 77±7 | 0.003a) | -0.48 | -0.79 | -0.16 | 0.85 |
| Height (cm) | 153.7±6.9 | 154.1±6.8 | 152.5±7.0 | 0.135a) | 0.24 | -0.08 | 0.56 | 0.32 |
| Weight (kg) | 54.1±8.8 | 54.6±8.6 | 52.9±9.2 | 0.234a) | 0.19 | -0.13 | 0.51 | 0.22 |
| BMI (kg/m2) | 22.9±3.1 | 22.9±3.1 | 22.7±3.3 | 0.605a) | 0.08 | -0.23 | 0.40 | 0.08 |
| Grip (kg/kg) | 0.93±0.20 | 0.95±0.19 | 0.85±0.21 | 0.002a) | 0.51 | 0.19 | 0.83 | 0.89 |
| Knee extension strength (N/kg) | 12.97±3.95 | 13.21±3.82 | 12.33±4.22 | 0.169a) | 0.22 | -0.10 | 0.54 | 0.28 |
| CS-30 (stands) | 22±7 | 23±7 | 20±7 | 0.007a) | 0.44 | 0.12 | 0.76 | 0.78 |
| TUG (s) | 5.7±1.4 | 5.4±0.9 | 6.5±2.0 | 0.001a) | -0.78 | -1.12 | -0.47 | 1.00 |
| Maximum walking speed (m/s) | 1.9±0.4 | 2.0±0.4 | 1.7±0.3 | <0.001a) | 0.68 | 0.36 | 1.00 | 0.99 |
| MMSE | 29 (28–30) | 30 (28–30) | 29 (27–30) | 0.016b) | 0.17 | 0.54 | ||
| J-CHS total points | 0 (0–1) | 0 (0–0) | 1 (1–1) | <0.001b) | 0.99 | 1.00 | ||
| KCLd) | ||||||||
| IADL | 0 (0–0) | 0 (0–0) | 0 (0–0) | 0.981b) | 0.00 | 0.06 | ||
| Physical function | 0 (0–1) | 0 (0–1) | 1 (0–1) | <0.001b) | 0.32 | 0.99 | ||
| Nutritional status | 0 (0–0) | 0 (0–0) | 0 (0–1) | <0.001b) | 0.28 | 0.98 | ||
| Oral function | 0 (0–1) | 0 (0–1) | 1 (0–1) | 0.005b) | 0.20 | 0.84 | ||
| Social isolation | 0 (0–0) | 0 (0–0) | 0 (0–0) | 0.296b) | 0.08 | 0.23 | ||
| Cognitive function | 0 (0–1) | 0 (0–1) | 0 (0–1) | 0.856b) | 0.01 | 0.05 | ||
| Depressive mood | 0 (0–1) | 0 (0–0) | 1 (0–1) | <0.001b) | 0.39 | 1.00 | ||
| Total points | 2 (1–3) | 1 (1–3) | 3 (2–6) | <0.001b) | 0.38 | 0.64 | ||
Values are presented as number (%) or mean±standard deviation or median (1st quartile–3rd quartile).
BMI, body mass index; CS-30, 30-seconds chair stand test; TUG, Timed up and go test; MMSE, Mini-Mental State Examination; J-CHS, Japanese version of the Cardiovascular Health Study; KCL, Kihon Checklist; IADL, instrumental activities of daily living; CI, confidence interval.
Table 2.
KCL associated with robustness and prefrailty (binomial logistic regression analysis)
Table 3.
Characteristics of life-related domains associated with robust and prefrailty
| Domain | KCL questions | Answer | Robust (n=140) | Prefrailty (n=54) | p-value | Effect size |
95% CI |
Power | |
|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||||
| Physical function | 6. Do you normally climb stairs without using handrail or wall for support? | No | 14 (9) | 19 (35) | <0.001a) | 0.30 | 0.13 | 0.45 | 0.98 |
| 7. Do you normally stand up from a chair without any aids? | No | 6 (4) | 9 (16) | 0.007b) | 0.21 | 0.04 | 0.35 | 0.83 | |
| 8. Do you normally walk continuously for 15 minutes? | No | 1 (1) | 1 (2) | 0.480b) | 0.05 | 0.01 | 0.19 | 0.11 | |
| 9. Have you experienced a fall in the past year? | Yes | 13 (9) | 9(17) | 0.146a) | 0.10 | -0.01 | 0.27 | 0.29 | |
| 10. Do you have a fear of falling while walking? | Yes | 15 (11) | 14 (26) | 0.008a) | 0.19 | 0.04 | 0.35 | 0.75 | |
| Nutritional status | 11. Have you lost 2 kg or more in the past 6 months? | Yes | 1 (1) | 13 (24) | <0.001b) | 0.41 | 0.26 | 0.53 | 1.00 |
| 12. Height: cm, weight: kg, BMI: kg/m2 If BMI is <18.5, this item is scored | Yes | 10 (7) | 4 (7) | 1.000b) | 0.01 | 0.00 | 0.17 | 0.05 | |
| Depressive mood | 21. In the last 2 weeks have you felt a lack of fulfillment in your daily life? | Yes | 4 (3) | 7 (13) | 0.012b) | 0.20 | 0.04 | 0.34 | 0.80 |
| 22. In the last 2 weeks have you felt a lack of joy when doing the things youused to enjoy? | Yes | 3 (2) | 4 (7) | 0.096b) | 0.13 | 0.01 | 0.28 | 0.44 | |
| 23. In the last 2 weeks have you felt difficulty in doing what you could do easily before? | Yes | 15 (11) | 21 (37) | <0.001a) | 0.31 | 0.16 | 0.46 | 0.99 | |
| 24. In the last 2 weeks have you felt helpless? | Yes | 2 (1) | 5 (9) | 0.019b) | 0.19 | 0.03 | 0.33 | 0.75 | |
| 25. In the last 2 weeks have you felt tired without a reason? | Yes | 1 (1) | 13 (24) | <0.001b) | 0.41 | 0.27 | 0.53 | 1.00 | |
REFERENCES
1. Yamada M, Arai H. Predictive value of frailty scores for healthy life expectancy in community-dwelling older Japanese adults. J Am Med Dir Assoc 2015;16:1002.

2. Alvarez-Bustos A, Carnicero-Carreno JA, Sanchez-Sanchez JL, Garcia-Garcia FJ, Alonso-Bouzon C, Rodriguez-Manas L. Associations between frailty trajectories and frailty status and adverse outcomes in community-dwelling older adults. J Cachexia Sarcopenia Muscle 2022;13:230–9.



3. Hoogendijk EO, Dent E. Trajectories, transitions, and trends in frailty among older adults: a review. Ann Geriatr Med Res 2022;26:289–95.




4. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001;56:M146–56.


5. Satake S, Shimada H, Yamada M, Kim H, Yoshida H, Gondo Y, et al. Prevalence of frailty among community-dwellers and outpatients in Japan as defined by the Japanese version of the Cardiovascular Health Study criteria. Geriatr Gerontol Int 2017;17:2629–34.



6. Shimada H, Makizako H, Doi T, Yoshida D, Tsutsumimoto K, Anan Y, et al. Combined prevalence of frailty and mild cognitive impairment in a population of elderly Japanese people. J Am Med Dir Assoc 2013;14:518–24.


7. Malmstrom TK, Miller DK, Morley JE. A comparison of four frailty models. J Am Geriatr Soc 2014;62:721–6.




8. Makizako H, Shimada H, Doi T, Tsutsumimoto K, Suzuki T. Impact of physical frailty on disability in community-dwelling older adults: a prospective cohort study. BMJ Open 2015;5:e008462.



9. Koyama S, Otobe Y, Suzuki M, Kimura Y, Ishiyama D, Kojima I, et al. Relationship between the Kihon Checklist and all-cause hospitalization among community-dwelling older adults. Geriatr Gerontol Int 2022;22:132–7.



10. Nanri H, Yoshida T, Watanabe Y, Fujita H, Kimura M, Yamada Y, et al. The association between habitual green tea consumption and comprehensive frailty as assessed by Kihon Checklist indexes among an older Japanese population. Nutrients 2021;13:4149.



11. Matsushita E, Okada K, Ito Y, Satake S, Shiraishi N, Hirose T, et al. Characteristics of physical prefrailty among Japanese healthy older adults. Geriatr Gerontol Int 2017;17:1568–74.



12. Noh JH, Jung HW, Ga H, Lim JY. Ethical guidelines for publishing in the Annals of Geriatric Medicine and Research. Ann Geriatr Med Res 2022;26:1–3.




13. Satake S, Arai H. The revised Japanese version of the Cardiovascular Health Study criteria (revised J-CHS criteria). Geriatr Gerontol Int 2020;20:992–3.



14. Ito K, Kawai H, Tsuruta H, Obuchi S. Predicting incidence of long-term care insurance certification in Japan with the Kihon Checklist for frailty screening tool: analysis of local government survey data. BMC Geriatr 2021;21:22.




15. Assantachai P, Muangpaisan W, Intalapaporn S, Jongsawadipatana A, Arai H. Kihon Checklist: Thai version. Geriatr Gerontol Int 2021;21:749–52.



16. Sentandreu-Mano T, Cezon-Serrano N, Cebria I Iranzo MA, Tortosa-Chulia MA, Tomas JM, Salom Terradez JR, et al. Kihon Checklist to assess frailty in older adults: some evidence on the internal consistency and validity of the Spanish version. Geriatr Gerontol Int 2021;21:262–7.



17. Kondo Y, Yoshida Y, Iioka T, Kataoka H, Sakamoto J, Hirase T, et al. Short-term effects of isometric quadriceps muscle exercise with auditory and visual feedback on pain, physical function, and performance after total knee arthroplasty: a randomized controlled trial. J Knee Surg 2022;35:922–31.


18. Anwer S, Alghadir A. Effect of isometric quadriceps exercise on muscle strength, pain, and function in patients with knee osteoarthritis: a randomized controlled study. J Phys Ther Sci 2014;26:745–8.



19. Jones CJ, Rikli RE, Beam WC. A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Res Q Exerc Sport 1999;70:113–9.


20. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189–98.

21. Holsinger T, Deveau J, Boustani M, Williams JW Jr. Does this patient have dementia? JAMA 2007;297:2391–404.


22. Fan L, Hou XY, Liu Y, Chen S, Wang Q, Du W. Catastrophic health expenditure associated with frailty in community-dwelling Chinese older adults: a prospective cohort analysis. Front Public Health 2021;9:718910.



23. Martinez-Arnau FM, Prieto-Contreras L, Perez-Ros P. Factors associated with fear of falling among frail older adults. Geriatr Nurs 2021;42:1035–41.


24. Raji MA, Kuo YF, Snih SA, Markides KS, Peek MK, Ottenbacher KJ. Cognitive status, muscle strength, and subsequent disability in older Mexican Americans. J Am Geriatr Soc 2005;53:1462–8.


25. Menant JC, Schoene D, Sarofim M, Lord SR. Single and dual task tests of gait speed are equivalent in the prediction of falls in older people: a systematic review and meta-analysis. Ageing Res Rev 2014;16:83–104.


26. Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther 2000;80:896–903.



27. Zhang Z, Fan Z, Zhang J. Correlation between frail status and lower extremity function in elderly inpatients with hypertension. Nutr Hosp 2022;39:39–45.

28. Pegorari MS, Tavares DM. Frailty-associated factors among Brazilian community-dwelling elderly people: longitudinal study. Sao Paulo Med J 2019;137:463–70.


29. Nishida T, Yamabe K, Honda S. The influence of dysphagia on nutritional and frailty status among community-dwelling older adults. Nutrients 2021;13:512.



30. Kugimiya Y, Motokawa K, Yamamoto K, Hayakawa M, Mikami Y, Iwasaki M, et al. Relationship between the rate of a decreased oral function and the nutrient intake in community-dwelling older persons: an examination using oral function-related items in a questionnaire for latter-stage elderly people. Nihon Ronen Igakkai Zasshi 2021;58:91–100.


31. Muszalik M, Kotarba A, Borowiak E, Puto G, Cybulski M; Kȩdziora-Kornatowska K. Socio-demographic, clinical and psychological profile of frailty patients living in the home environment and nursing homes: a cross-sectional study. Front Psychiatry 2021;12:736804.



32. Liu J, Fujii Y, Fujii K, Seol J, Kim M, Tateoka K, et al. Pre-frailty associated with traffic crashes in Japanese community-dwelling older drivers. Traffic Inj Prev 2022;23:73–8.


33. Noguchi T, Murata C, Hayashi T, Watanabe R, Saito M, Kojima M, et al. Association between community-level social capital and frailty onset among older adults: a multilevel longitudinal study from the Japan Gerontological Evaluation Study (JAGES). J Epidemiol Community Health 2022;76:182–9.


34. Kitamura M, Goto T, Fujiwara S, Shirayama Y. Did “Kayoinoba” prevent the decline of mental and physical functions and frailty for the home-based elderly during the COVID-19 pandemic? Int J Environ Res Public Health 2021;18:9502.



35. Cobden J, de Noronha M, Kingsley M. Prevalence of frailty and mobility disability in older people living in retirement villages. Australas J Ageing 2022;41:222–8.



36. Umegaki H, Makino T, Uemura K, Shimada H, Cheng XW, Dodge H, et al. Falls in community-dwelling prefrail older adults. Health Soc Care Community 2020;28:110–5.



37. Sezgin D, O’Donovan M, Woo J, Bandeen-Roche K, Liotta G, Fairhall N, et al. Early identification of frailty: developing an international delphi consensus on pre-frailty. Arch Gerontol Geriatr 2022;99:104586.


38. Sella-Weiss O. Association between swallowing function, malnutrition and frailty in community dwelling older people. Clin Nutr ESPEN 2021;45:476–85.


39. Imaoka M, Nakao H, Nakamura M, Tazaki F, Hida M, Omizu T, et al. Associations between depressive symptoms and geriatric syndromes in community-dwelling older adults in Japan: a cross-sectional study. Prev Med Rep 2021;22:101353.



40. Soysal P, Veronese N, Thompson T, Kahl KG, Fernandes BS, Prina AM, et al. Relationship between depression and frailty in older adults: a systematic review and meta-analysis. Ageing Res Rev 2017;36:78–87.


41. Amitani M, Asakawa A, Amitani H, Inui A. Control of food intake and muscle wasting in cachexia. Int J Biochem Cell Biol 2013;45:2179–85.


42. Kodama A, Kume Y, Lee S, Makizako H, Shimada H, Takahashi T, et al. Impact of COVID-19 pandemic exacerbation of depressive symptoms for social frailty from the ORANGE registry. Int J Environ Res Public Health 2022;19:986.



43. Su Q, Gao Y, Zhang J, Tang J, Song M, Song J, et al. Prevalence of fear of falling and its association with physical function and fall history among senior citizens living in rural areas of China. Front Public Health 2021;9:766959.



44. Qazi SL, Koivumaa-Honkanen H, Rikkonen T, Sund R, Kroger H, Isanejad M, et al. Physical capacity, subjective health, and life satisfaction in older women: a 10-year follow-up study. BMC Geriatr 2021;21:658.




- TOOLS