Mortality-Related Risk Factors in Geriatric Patients with Hip Fracture
Article information
Abstract
Background
Mortality rates after hip fractures increase by up to 30% with age. This study investigated the contribution of various parameters to prognosis and mortality.
Methods
Our study prospectively examined patients with hip fracture aged 65 years and over who applied to the Atatürk University Medical Faculty Hospital Orthopedics Service in 2020–2021.
Results
The 120 patients included in the study had a mean age of 79.71±7.27 years, and 51.7% were female. Twenty patients (16.7%) died within the first 30 days after a hip fracture. They had a significantly lower median Lawton–Brody instrumental activities of daily living (IADL) scale score (p=0.045) and a higher rate of malnutrition according to the Mini Nutritional Assessment (MNA) score (p=0.016). Additionally, these patients with 30-day mortality had a significantly lower rate of surgical treatment (p=0.027) and a longer time from injury to surgery (p=0.014). The time to surgery was a significant independent risk factor for 30-day mortality, with each 1-hour delay increasing the odds of mortality by 1.066 (odds ratio [OR]=1.066; 95% confidence interval [CI], 1.001–1.013; p=0.013). In addition, the presence of malnutrition was another independent risk factor that increased the odds of mortality by 4.166 times (OR=4.166; 95% CI, 1.285–13.427; p=0.017).
Conclusion
We recommend placing more importance on supportive treatment in patients presenting with hip fractures, especially in those with malnutrition; performing surgical intervention as early as possible; and more closely following up with patients with the aforementioned risk factors.
INTRODUCTION
Improved healthcare and living standards have increased the average life expectancy.1) As the human lifespan lengthens, older adults are increasing in both number and proportion of the total population. According to the Turkish Statistical Institute’s (TurkStat) “Statistics of Older Adults 2021” bulletin, the population aged 65 years and over in Turkey rose by 24% over 5 years, from 6,651,503 in 2016 to 8,245,124 in 2021, and the proportion of older adults within the total population rose from 8.3% in 2016 to 9.7% in 2021.2,3) Aging leads to many physiological changes in the human body. Among these, reduced muscle mass and strength, loss of bone mass, and nervous system effects result in a decline in neuromuscular function, which leads to impairments in proprioception, balance, and coordination and increases the risk of falls.4)
Comorbidities and polypharmacy increase with age and negatively affect the musculoskeletal and nervous systems. In addition, older adults are more likely than younger adults to experience fractures after low-energy trauma due to osteoporosis, which is more common in postmenopausal women. These fractures are mostly observed in the upper and lower extremities; however, hip fractures also occur and are concerning. Fractures adversely impact daily life and result in death in many cases.3,5)
Among studies on the incidence of hip fractures and prevalence of osteoporosis in Turkey, the FRACTURK study in 2011 reported that the incidence of hip fractures increased with age. The annual number of new hip fractures is estimated to reach 60,000 by 2035.5) A study in Korea between 2002 and 2011 reported an annual incidence of hip fractures of 4.3%,6) while a retrospective study in Spain showed that the incidence of hip fractures increased markedly in persons aged 85 and older.7)
Older adults have a prolonged recovery period after a hip fracture and difficulty returning to their activities of daily living. During recovery, patients are usually bedridden and dependent on family members or nursing home workers.8) Despite medical advances, the mortality rate of hip fractures remains high in geriatric populations, with reported 1- and 3-year mortality rates of 30% and up to 40%, respectively.9-12) Considering the growing geriatric population and high incidence of hip fractures and mortality, this issue will become increasingly important. This study investigated the risk factors associated with the prognosis of hip fractures in geriatric patients, who are a known risk group for mortality.
MATERIALS AND METHODS
The inclusion criteria for this prospective, observational study were as follows: individuals >65 years of age who were admitted to the orthopedic ward due to a hip fracture between April 1, 2020 and August 30, 2021, who volunteered to participate in the study, and who signed the informed consent form.
The exclusion criteria were individuals ages <65 and older who had refused to participate in the study and who did not sign the informed consent form.
This study evaluated demographic and clinical characteristics such as age, sex, marital status, education level, chronic diseases, the presence of osteoporosis before the fracture, and the use of osteoporosis medication. Osteoporosis and fractures were specified in the questionnaire, and all participants indicated whether they were currently undergoing treatment or had been diagnosed with the disease.
The Acute Physiology and Chronic Health Evaluation II (APACHE-II),13) Charlson Comorbidity Index (CCI), American Society of Anesthesiologists (ASA)14) classification, Lawton–Brody instrumental activities of daily living (IADL) scale,15) Barthel Index,16) Edmonton Frail Scale (EFS),17,18) and Mini Nutritional Assessment (MNA)19,20) scores were calculated at the time of admission. The MNA consists of six global assessment items covering the level of independence, medications used, mobility, mental status, skin changes, and the presence of acute stressors during the previous 3 months. The MNA yields a score between 0 and 14. Scores of 12–14 indicate normal nutritional status (being well-nourished), 8–11 indicate malnutrition risk, and 0–7 indicate malnourishment.19) The Barthel Index, reported in 1967, consists of 10 question groups.16) The validity and safety of the Turkish version were reported in 2000 by Kucukdeveci et al.21) The 10 question groups include nutrition, moving from wheelchair to bed and vice versa, personal care, using the toilet, walking on a smooth surface, using a wheelchair, going up and down stairs, dressing, undressing, urine and stool continence, and washing. The total score is 100, in which 0–20 points indicate full dependence, 21–61 points indicate severe dependence, 62–90 points indicate moderate dependence, 91–99 points indicate slight dependence, and 100 points indicate complete independence. The Lawton–Brody IADL was developed by Lawton and Brody15) in 1969. It consists of eight questions, including using the telephone, managing money, cooking, cleaning the house, washing laundry, and using a transportation vehicle. The maximum possible score is 24 points, with scores of 0–8, 9–16, and 17–24 points defined as dependent, semi-dependent, and independent, respectively. The EFS is a simple and easily administered scale consisting of 11 questions that provide information about cognition, general health status, dependence, social support, medication, nutrition, depression, incontinence, and physical performance.17) Each question is scored between 0 and 2. Total scores of 0–5, 6–7, 8–9, 10–11, and 12–17 indicate no frailty, vulnerability, mild frailty, moderate frailty, and severe frailty, respectively.
To assess geriatric syndromes, the number of falls in the previous year, the presence of dementia, and whether delirium occurred after a hip fracture were determined. White blood cell, neutrophil, and lymphocyte counts; mean platelet volume (MPV); hematocrit; hemoglobin; blood urea nitrogen (BUN); and creatinine, sodium, potassium, calcium, phosphorus, alanine aminotransferase (ALT), aspartate aminotransferase (AST), albumin, and C-reactive protein (CRP) levels at the time of admission to the emergency department were recorded. The length of stay in the emergency department; whether the patient underwent surgery, and if so, how many hours later; the anesthesia method; any postoperative complications; and the length of stay in the orthopedic ward were also noted.
The 30-day survival data of the patients were retrieved from the Death Reporting System of the Republic of Turkey Ministry of Health, General Directorate of Public Health, using patient citizenship numbers.
Statistics
Statistical analyses were performed using the IBM SPSS Statistics for Windows, version 21.0 program (IBM, Armonk, NY, USA). Descriptive statistics are presented as medians and ranges, or numbers and percentages. Data were compared between surviving and non-surviving patients.
A receiver operating characteristic curve analysis was performed to evaluate the relationship between the variables and mortality. The area under the curve was calculated, and the cutoff points were determined using the Youden index (J=sensitivity+specificity–1). The chi-square test was used to compare categorical data between the surviving and non-surviving groups, while continuous data with non-normal distributions were compared using the nonparametric Kruskal–Wallis and Mann–Whitney U tests. A Kaplan–Meier analysis was performed to identify the risk factors associated with survival time. Significant risk factors in the Kaplan–Meier analysis were included in a Cox regression model to identify independent risk factors. Results were calculated with 95% confidence intervals (CIs), and p<0.05 was considered statistically significant.
This study was performed after obtaining approval from the Clinical Research Ethics Committee of Erzurum Regional Training and Research Hospital (No. 2020/07-87, dated April 6, 2020). Also, this study complied the ethical guidelines for authorship and publishing in the Annals of Geriatric Medicine and Research.22)
RESULTS
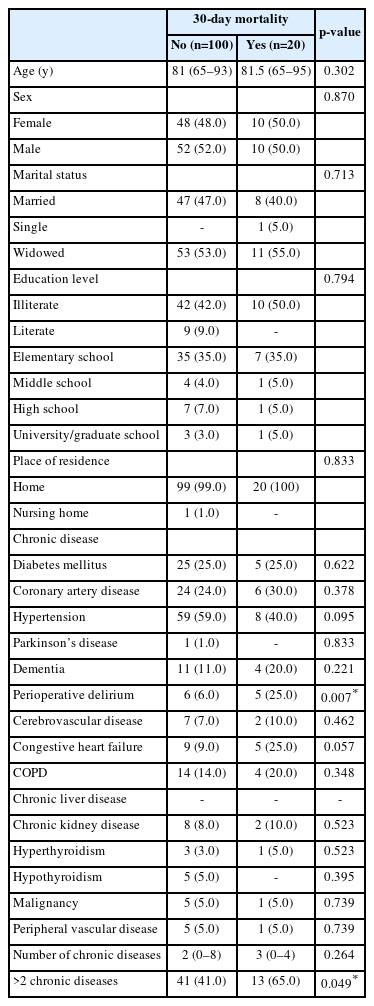
The 120 patients included in the study had a mean age of 79.71±7.27 years, and 51.7% were female. Twenty patients (16.7%) died within the first 30 days after the hip fracture. Table 1 shows a comparison of demographic characteristics and comorbidities according to 30-day mortality.
The presence and treatment of osteoporosis and the number of falls in the previous year were compared according to 30-day mortality (Table 2). Having had two or more falls causing injury within the last year was significantly more common among patients who died within 30 days of the hip fracture (p=0.011).
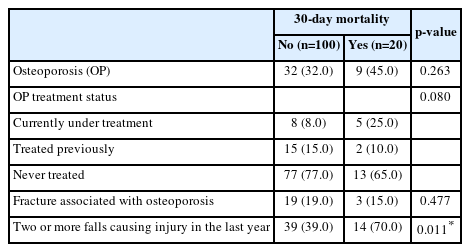
Comparison of the frequency of osteoporosis, treatment for osteoporosis, and falls in the last year according to 30-day mortality
Table 3 shows the comparison of the assessment scores and laboratory findings at admission according to the 30-day mortality. Patients who died within 30 days of a hip fracture had a significantly lower median Lawton–Brody IADL scale score (p=0.045) and a higher rate of malnutrition according to the MNA score (p=0.016).
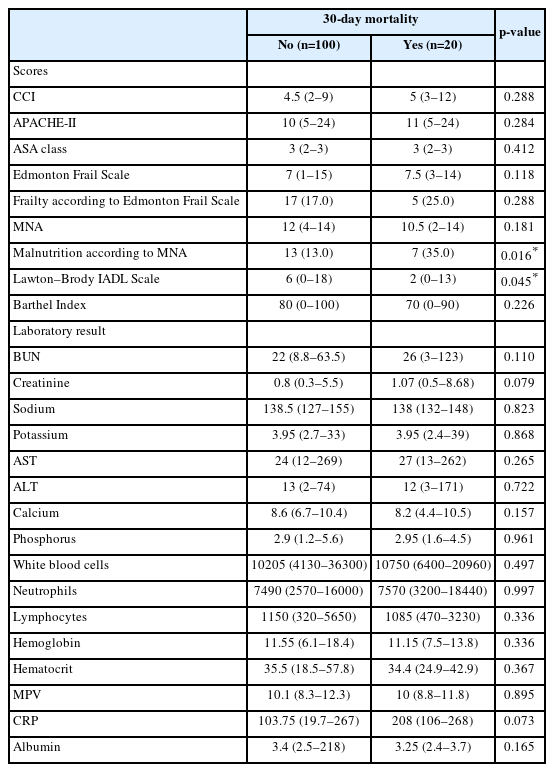
Comparison of assessment scores and laboratory findings at hospital admission according to 30-day mortality
Comparisons between patients with and without 30-day mortality in terms of length of hospital stay, surgical treatment, and complications are shown in Table 4. Patients with 30-day mortality had a significantly lower rate of surgical treatment (p=0.027) and a longer time from injury to surgery (p=0.014).

Comparison of patient length of stay, surgery presence and timing, and complications according to 30-day mortality
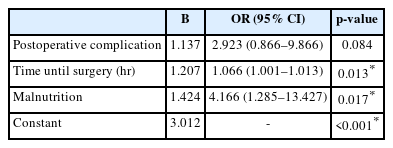
The last line of logistic regression analysis, including 30-day mortality risk factors in older patients with hip fractures, is shown in Table 5. Among the factors directly associated with mortality risk, we created a logistic regression model that included surgery, time until surgery, presence of postoperative complications, presence of perioperative delirium, Lawton–Brody IADL scores, presence of malnutrition according to the MNA, and presence of two or more falls causing injury in the previous year. Time to surgery was a significant independent risk factor for 30-day mortality, with each 1-hour delay increasing the odds of mortality by 1.066 (odds ratio [OR]=1.066; 95% CI, 1.001–1.013; p=0.013). The presence of malnutrition was another independent risk factor that increased the odds of mortality by 4.166-fold (OR=4.166; 95% CI, 1.285–13.427; p=0.017).
DISCUSSION
In our study of geriatric patients, 16.7% died within 30 days of experiencing a hip fracture. Moreover, the odds of mortality increased by 1.066-fold with each hour of delay in surgery and by 4.166-fold in patients with malnutrition.
Turhan et al.23) reported a 1-year mortality rate of 21.73% in their study of 138 geriatric patients in Turkey who underwent surgery for hip fractures, while Guzon-Illescas et al.24) reported a 1-year mortality rate of 33% in their study of 3,992 patients with hip fractures. Kim et al.25) reported 1- and 5-year mortality rates after hip fractures of 20.9% and 67.2%, respectively. In our study, 20 patients died (16.7%) within the first 30 days, which was attributed to mortality associated with hip fractures and possible complications.
The positive relationship between mortality rate and age reported in recent studies is noteworthy. In their meta-analysis of 54 studies, including 22,817 cases from 2008 to 2018, Cui et al.26) reported 1-year mortality rates of 2.65% in patients aged 50–54 years and 28.91% in those aged 95–99 years. A retrospective study of 1,004 patients by Cher et al.27) showed that older age was an independent risk factor for 30-day mortality. Contrary to the literature, in the present study, mortality did not increase with age. This difference could be attributed to the small sample size.
Although the incidence of hip fractures is higher in women, the mortality rate is higher in men. In a retrospective study including 32,175 patients in Norway, Riska et al.28) compared mortality rates between male and female patients with similar comorbidities. They reported estimated 1-year mortality risks of 44% for women and 53% for men among patients with a CCI of ≥2. A retrospective study by Prodovic et al.,29) which included 597 cases, showed a 25% higher cumulative quarterly mortality rate in men. Similarly, mortality was higher among the men in our study, although the difference was not statistically significant.
Malnutrition in older adults can be associated with various factors, such as a shift to catabolic metabolism and low oral intake secondary to comorbidities, and may contribute to higher mortality after hip fractures. In this meta-analysis of 19 studies, including 34,363 cases, Li et al.30) reported higher mortality among patients classified as malnourished or at risk of malnutrition according to the MNA. Another meta-analysis of 44 studies and 26,281 patients by Malafarina et al. showed higher mortality rates in malnourished patients.9) Previous studies on nutritional evaluation reported a correlation between serum albumin levels and postoperative survival.31-36) Three of these studies observed a correlation between serum albumin levels and total lymphocyte count, nutrition, and postoperative survival.33,34,36) In addition, a recent review reported a relationship between weight loss and serum albumin levels.37) However, serum albumin levels and total lymphocyte counts can be affected by existing inflammatory processes and underlying diseases. Similar to our study, a retrospective study of 236 older patients, which included 226 patients evaluated using the MNA, reported 1-year mortality rates of 27% overall and 46% in patients with malnutrition.38) Finally, in their study, including 88 patients, Guimieiro et al.39) reported a relationship between MNA score and 6-month mortality. Similar to these studies, we observed that malnutrition was an independent factor associated with an increased risk of mortality after a hip fracture.
Surgery for patients with hip fractures may be delayed depending on their medical condition or organizational challenges at health institutions. A meta-analysis of 28 studies that investigated the effect of surgical delay on mortality after hip fracture reported a higher mortality rate among patients operated on after 48 hours or more.40) Similarly, Leer-Salvasen et al.41) reported higher mortality among patients who underwent surgery after 48 hours or more. In a prospective study by Lizaur-Utrilla et al.42) with 1,234 patients, waiting did not affect mortality in medically unstable patients, whereas surgical delay in stable patients increased 1-year mortality. Our results showed that surgical delay was an independent risk factor for 30-day mortality, with each 1-hour delay increasing the odds of 30-day mortality by 1.066-fold.
Delirium is an organic brain pathology that frequently occurs in older patients owing to surgery, trauma, and stress.43) As it may be an indicator of mortality and stress, several studies have reported on this topic. A meta-analysis of 21 studies and 6,288 cases by Bai et al.44) showed that perioperative delirium is a risk factor for increased short- and long-term mortality. A retrospective study by Mitchel et al.45) that included 27,888 patients showed that the incidence of perioperative delirium increased the risk of 1-year mortality. Another study involving 463 patients reported higher 1-year mortality.46) Our results support the literature, as patients with perioperative delirium were significantly more likely to die within 30 days of a hip fracture.
Comorbidities increase with age and adversely affect healing. Additionally, mortality increases with the number of comorbidities. A retrospective study of 1,004 patients by Cher et al.27) evaluated comorbidity status according to the CCI and reported a positive association between mortality and the number of comorbidities. Another retrospective study of 3,992 patients by Guzon-Illescas et al.24) showed that the presence of stage 4–5 chronic kidney disease, diabetes mellitus, chronic obstructive pulmonary disease, dementia, congestive heart failure, vision and hearing problems, and urinary incontinence increased the risk of mortality. In another retrospective study that included 19,682 patients with hip fractures, the presence of congestive heart failure, diabetes mellitus, and malignancy increased 30-day mortality.47) As expected, we observed a higher mortality rate among patients with three or more comorbidities, which is consistent with the literature.
In a study including 802 cases of hip fractures that occurred between 2008 and 2018, the presence of postoperative complications increased the risk of 1-year mortality.48) Similarly, Gurger49) and Barbosa et al.50) showed that postoperative complications were associated with higher 1-year mortality. Although we did not individually evaluate the postoperative complications in our study, we observed that frail patients had higher mortality rates in the presence of complications.
Consistent with our findings, Drevet et al.51) also demonstrated the importance of activities of daily living in preventing the negative consequences of such trauma in their prospective study on the effects of IADL performance on mortality in 113 patients.
Few studies have investigated the effects of hip fractures on mortality in older patients. The strength of our study was its prospective design. The limitations of this study were that it was conducted in a single center and included a small number of patients. Another limiting factor was that patients with advanced dementia were not included. Moreover, patient mobilization status was not assessed during the postoperative period. Finally, no distinction was made based on the type of hip fracture.
In conclusion, to reduce high mortality rates, patients with hip fractures should undergo a detailed geriatric evaluation before surgery, and their medical problems should be stabilized as early as possible. Thus, planning surgery immediately for patients with indications for surgery and closely following patients with malnutrition is important to reduce mortality after hip fracture.
Notes
CONFLICT OF INTEREST
The researchers claim no conflicts of interest.
FUNDING
None.
AUTHOR CONTRIBUTIONS
Conceptualization, RG, PTT, OK, KT, DNB, SS; Data curation, RG, PTT, CS, MT; Investigation and Methodology, OK; Writing-original draft, RG, PTT, OK, KT, DNB, SS; Writing-review & editing, SS.