An Uncommon Case of Weight Loss in a Nonagenarian
Article information
Abstract
Weight loss in older adults can be due to multiple causes. A systematic approach is required to pinpoint the etiology. Dysphagia is an important symptom associated with weight loss. In the absence of anatomical abnormalities, functional swallowing disorders such as achalasia can be mistaken for an aging esophagus or oropharynx. The incidence of achalasia in older adults is rare, with most cases presenting between 30 to 60 years of age. Here, we present an uncommon case of achalasia in a 93-year-old Chinese woman. A barium swallow and high-resolution manometry confirmed the diagnosis of achalasia. Botulinum toxin injection was administered. She did well, achieving weight gain and resolution of her symptoms. In conclusion, early recognition and appropriate management of uncommon causes of weight loss can greatly improve the quality of life of older adults.
INTRODUCTION
Weight loss is a well-defined geriatric syndrome.1) Its prevalence ranges from 15% to 20% among adults >65 years of age.2) There are multiple causes of weight loss; thus, it requires thorough evaluation.2,3) Dysphagia is an important symptom associated with weight loss and can be caused by various etiologies.4-6) Achalasia is a functional esophageal disorder that causes dysphagia. It can masquerade as an aging esophagus if not carefully evaluated. Achalasia is defined as esophageal aperistalsis and a lack of relaxation of the lower esophageal sphincter.7) Among the three types of achalasia, type 2 shows intermittent periods of pressurization. Achalasia is rare, with an incidence of 0.3–1.63 per 100,000 people per year in adults.8) It is generally observed in adults aged 30–60 years.9) We describe the assessment and management of a nonagenarian patient who presented with weight loss and dysphagia secondary to type 2 achalasia.
CASE REPORT
A 93-year-old Chinese woman who required assistance in basic activities of daily living (BADLs) at home without a walking aid and was dually continent presented to the Emergency Department with recurrent vomiting, dysphagia, and an 8-kg weight loss over 6 months. She was admitted to the geriatric inpatient ward. She reported difficulty in swallowing liquids and solids, often associated with a globus sensation. She denied reflux symptoms such as heartburn and acid regurgitation. Examination showed normal vital signs and no significant findings. Her medical history included mild dementia (mixed vascular and Alzheimer’s etiology) with a Mini-Mental State Examination score of 22/30, ischemic heart disease with a left ventricular ejection fraction of 55%, postural hypotension, knee osteoarthritis and osteoporosis, and a history of falls with traumatic subdural hemorrhage. Her chronic medications included aspirin (100 mg), omeprazole (20 mg), and cholecalciferol (1000 IU) every morning. However, owing to recurrent vomiting, she had been unable to take oral medications regularly for the past 6 months.
Blood investigations revealed hypernatremia with acute kidney injury—raised urea: 17.6 mmol/L (normal limits being 2.1–8.4 mmol/L); sodium, 149 mmol/L; and creatinine, 86 μmol/L, up from a baseline creatinine of 49 μmol/L. Full blood counts showed normal hemoglobin (14.8 g/dL), leukocyte count (10×103 U/L), and platelets (159×103 U/L). Thyroid function, liver function, troponin levels, pancreatic enzyme levels, and urinalysis results were normal. Electrocardiography and chest and abdominal radiographical findings were unremarkable. Brain computed tomography (CT) did not reveal any infarcts or new bleeding. CT of the thorax and abdomen with intravenous contrast did not reveal any masses along the esophagus or the gastroesophageal junction. Esophagogastroduodenoscopy revealed no anatomical abnormalities. Barium swallow showed tertiary contractions with mild hold-up of contrast in the middle and distal esophagus (Fig. 1). As the patient had a good functional status and a low burden of comorbidities, repeated discussions were held with her family regarding high-resolution esophageal manometry.7) The results of this investigation showed an increased median integrated relaxation pressure of 30.9 mmHg and a lack of normal peristaltic contractions of the esophagus in response to swallowing (Fig. 2). These findings are consistent with type 2 achalasia.

Barium swallow. A barium swallow done during the admission showed tertiary contractions with mild hold-up of contrast in the middle to distal esophagus.
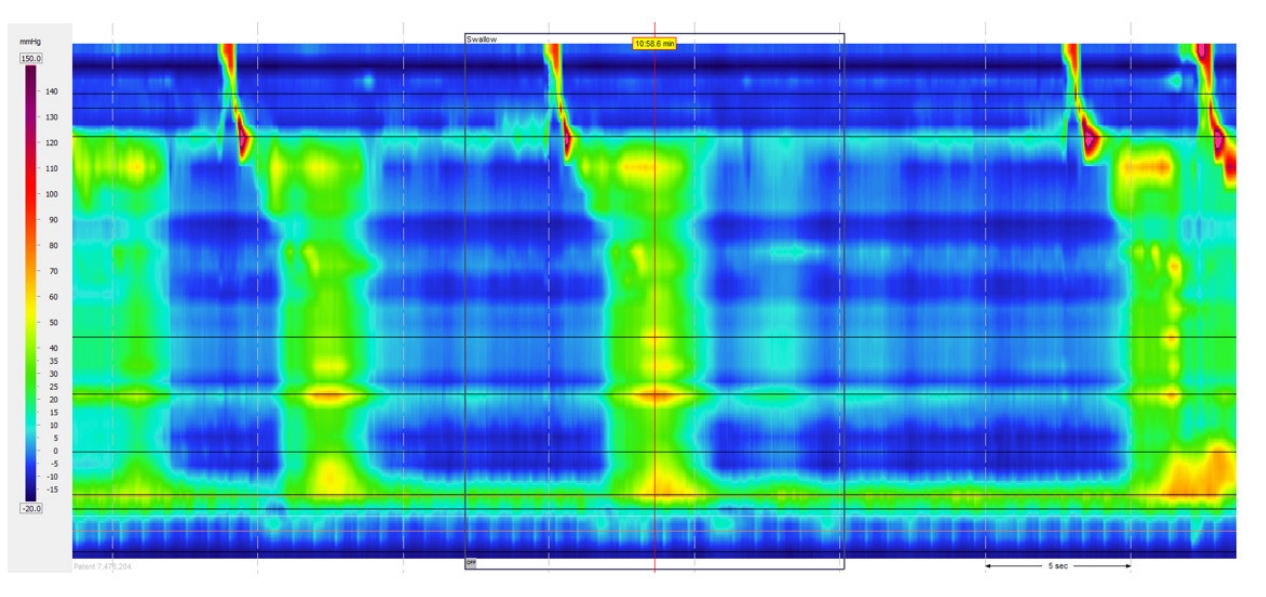
Type II achalasia (Chicago classification). Median integrated relaxation pressure was 30.9 mmHg (significant as more than 15 mmHg) and there was an absence of normal peristaltic contractions of the esophagus in response to swallows.
After establishing the diagnosis, a gastroenterologist was consulted. The suite of considered options included peroral endoscopic myotomy (POEM), pneumatic dilatation, laparoscopic Heller myotomy, botulinum injection into the gastroesophageal junction, and medical therapy via calcium channel blockers and nitrates.9) We also considered nasogastric tube feeding for nutritional support if prior management options were deemed unsuitable. After weighing the risks and benefits of the aforementioned treatments, surgical intervention was deemed too risky for this patient. Considering her history of significant postural hypotension and high risk of falls, treatment with calcium channel blockers and nitrates was also deemed unsuitable.
After a thorough discussion with the patient and family, botulinum injection was determined to be the most appropriate treatment, while emphasizing that its effect may wane after 6 month follow-up. As such, individuals may require repeated procedures, which increases the risk of esophageal fibrosis. The patient received botulinum injections and did not develop any complications during the procedure. Her dysphagia and vomiting resolved, and she could tolerate meals and liquid nutritional supplements well. The patient was discharged from the ward 1 week after the procedure. At a clinical review 3 months later, the patient remained symptom-free and was found to have gained 5 kg. She was scheduled for a subsequent outpatient gastroenterology review at 3–6 months after the procedure to observe symptom recurrence.
DISCUSSION
This case highlights a unique clinical presentation of dysphagia and weight loss resulting from a rare condition in a nonagenarian patient. Achalasia is generally diagnosed in middle-aged patients, i.e., between 30 and 60 years of age.9) Type 2 achalasia is most commonly associated with weight loss and is most responsive to botulinum treatment, as observed in our case.7,10) To add to the complexity of the diagnosis, an aging esophagus can also have laxity of the lower esophageal sphincter. Thus, without a high index of suspicion, the diagnosis of achalasia can be missed in older adults. In this case, wherein both endoscopy and contrast-enhanced CT scans did not reveal an obvious etiology, further targeted investigations helped identify achalasia as the cause. The management of this case required careful weighing of the risks and benefits of each treatment option to optimize the benefits and minimize potential harm to the patient. A literature review11) proposed the use of botulinum injection in adults aged >75 years with achalasia and recommended it as an efficacious yet lower-risk modality. Ideally, further research in the form of randomized controlled trials is required to prove the clinical benefits of this intervention. In conclusion, this unique case of achalasia in a nonagenarian serves as an important reminder of the uncommon causes of weight loss and dysphagia. A multidisciplinary approach involving geriatricians, gastroenterologists, geriatric nurses, therapists, and dieticians enabled the holistic management of this patient in a geriatric ward. Comprehensive investigations and carefully considered management of achalasia can markedly improve the quality of life in older adults.
Notes
CONFLICT OF INTEREST
The researchers claim no conflicts of interest.
FUNDING
None.
AUTHOR CONTRIBUTIONS
Conceptualization: GKSidhu, GKSern; Data curation: HHK; Investigation: GKSidhu, GKSern, HHK; Methodology: GKSidhu, GKSern, HHK; Project administration: GKSidhu, GKSern, HHK; Supervision: GKSidhu, GKSern.
