The National Programme for Health Care of the Elderly: A Review of its Achievements and Challenges in India
Article information
Abstract
Aging care is critical. Projections for 2020 indicate that India’s older population will comprise 6.57% of the overall population. The best-known newly developed technologies must be provided to the older population. Non-governmental organizations and private institutions are increasingly providing more door-to-door guidance and help. This study evaluated the impact of the National Programme for Health Care of the Elderly (NPHCE) in India and analyzed its achievements and challenges. The program’s key strategies include providing preventive and promotional care and sickness management, empowering geriatric services, and guaranteeing optimal rehabilitation. The NPHCE is an excellent project for caring for a rapidly aging population. This study described the existing programs and schemes related to older people in India, with a focus on the NPHCE and an analysis of the program’s achievements and challenges.
INTRODUCTION
“For happy old age keep a goal.” Aging is a process that converts a fit body into a frail one that is vulnerable to infections, injuries, and death.1) In India, “senior citizens” are defined as older adults of Indian nationality aged 60 years and above. The National Policy for Older Persons was established in 1999 by the Ministry of Statistics and Programme Implementation and the National Statistics Office of the Government of India. The older adult population has increased from 24.7 million in the 1961 census to a projected 137.9 million and 158.7 million for the 2022 and 2025 censuses, respectively, accounting for 11.1% of the overall population.2,3) This increasing older adult population leads to economic, social, and health concerns that require immediate and prompt responses from the government, enterprises, and society.4,5) The onus of morbidity is immense. Diseases pose great threats to older adults, whose socioeconomic status is questionable. Disabilities worsen the daily living activities of old age.6) While the United Nations Population Fund and Help Age India estimated that the senior population in India would increase to 173 million by 2026,7) by 2001, India had surpassed that percentage (7.47%) and is predicted to reach 12.6% by 2025. Hence, India’s aging population is drastically changing.8) In India, the populations aged 0–14, 15–59, and 60 years and above comprised 30.8%, 60.3%, and 8.6% of the total population, respectively.9) Older adults comprise 7.5% of the population, two-thirds of whom live in villages, with almost half in socioeconomically poor conditions.10) Every program for older adults created in India aims to provide older persons with discrete, specialized, and complete health care at various levels of the Indian healthcare delivery system, in addition to outreach programs. Over 70% of India’s geriatric population resides in rural areas, according to the 2011 census.11) It has been said that care for older adults should be the same as that for children. One Indian report indicated that 8%–10% of older adults will be bedridden and will require utmost care for their survival. The dual challenges of aging care include ensuring that older adults can live healthy, dignified, and productive lives and transforming them into partners rather than burdens on society.12) The rise in the senior population has resulted in an “older adult boom” in several parts of the country.13) The inequity and intricacies of India’s demographic shift are obscured by summary numbers that ignore the disparities and complexities of demographic transition among Indian states with varying degrees of economic development, cultural norms, and political circumstances.14) The main aim of this study is to describe the existing programs and schemes related to older people in India, with a focus on the National Programme for Health Care of the Elderly (NPHCE), and to analyze the achievements and challenges of this program.
MAIN FINDINGS
Issues Faced by the Older Population in India
Aging is a global phenomenon. India is in Stage 3 of the demographic transition, suggesting a fall in birth rate with the death rate remaining low and the population continuing to increase at a steady rate.15) This leads to a growth of the older population, making it crucial for India to develop policies addressing their health-related concerns. Instead of the traditional fragmented approach, which caters to the individual health challenges of the older population through disease-based programs for non-communicable illnesses, cancer, and mental health, a comprehensive approach to older population health care is required.16) Old age is associated with considerable mortality and morbidity, of which musculoskeletal pain is a major concern. This leads older adults to demand analgesics for pain relief. However, analgesics have detrimental effects on the body.17)
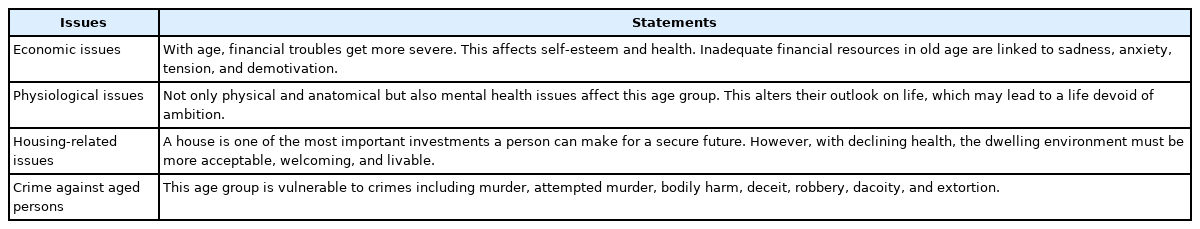
The key issues faced by older adults in India are outlined in Table 1. Other issues include vulnerability to certain types of infection. For example, waterborne infections are more common among the older population in rural locations. Older adults may not be aware of proper hygiene measures that contribute to their risk of illness. Thus, there is a need to increase awareness of basic hygiene in this community to prevent bacterial illnesses.18-21) Hence, older adults should be targeted for the prevention of bacterial infections.
Multimorbidity Patterns in Older Adults
According to the 2017 United Nations Population Fund report, performing activities of daily living is more difficult for older women than for older men.22) Aging accounts for a high prevalence of musculoskeletal diseases such as those affecting muscles, the spine, bone (osteoporosis), and joints (osteoarthritis), leading to frequent fall injuries.23) Aging is also influenced by various components, such as the surroundings in which older adults live, their families, their neighborhood, their communities, and their physical and mental capabilities, as well as their characteristics, including their sex, ethnicity, and socioeconomic status. The most crucial component that differs from younger populations is life experience. One of the pressing issues faced by the older population is depression, which manifests as social depression.24)
Multimorbidity has been a concern in recent decades, with increasing prevalence. India is experiencing significant epidemiological and demographic changes that have caused people to move faster toward aging. Through this transient phase, more older people have experienced long-term diseases that affect all aspects of their lives. Multimorbidity is more common overall among the older population (32.96%) and women (34.69%). Arthritis/rheumatism (54.75%), hypertension (45.79 %), tooth loss (32.94%), cataracts (31.34%), diabetes (23.11%), and asthma are the most common disorders among individuals with multiple morbidities (21.06%). Multimorbidity is strongly correlated with population aging and sex is a significant predictor of multimorbidity. Reducing the burden of multimorbidity requires researchers and policymakers to collaborate to create effective intervention techniques and programs.25-27)
To address this social issue, a screening program with timely review should be created. Multimorbidity patterns with robust epidemiological research for older adults will help mitigate the clinical complexities by targeting chronic diseases addressed by the healthcare delivery system from the grassroots to the national level.28-30) Polypharmacy should be evaluated regularly, to eliminate overlapping or superfluous medicines.31)
Urbanization Effects on the Older Population
Urbanization has caused a transition by transforming the economics of rural society, transport systems, and socioeconomic status.32) The residential patterns also affect the health of older adults due to the in-migration of the older population and the out-migration of young persons.33) The variety exhibited by the older population is not random and is affected by physical and social settings, as well as the influence of these factors on the possibilities and health behaviors. Personal traits such as the family older adults were born into, their sex, and their race distort their connection to the environment, resulting in health disparities.34)
Older adults are frequently stereotyped as fragile, dependent, and a societal burden. These and other ageist attitudes must be addressed by public health professionals and society as a whole, as they can lead to discrimination, influence policy development, and limit healthy aging.35,36)
Globalization Effects on the Older Population
Globalization, technological advancements (e.g., in transportation and communication), urbanization, migration, and changing gender norms have direct and indirect effects on the lives of older people. A public health response must assess the present and future trends and formulate appropriate policies.37) The abuse of older adults has been a pressing topic for many decades, defined as a single or recurrent act, or a failure to act appropriately, which causes injury or distress to older adults in any relationship where trust is expected.
Around 1 in 6 people 60 years and older had experienced some form of abuse in community settings during the past year, including physical, verbal, psychological, sexual, and financial, abuse, as well as neglect. This issue can be prevented through monetary help, helplines, and emergency shelters.38-41) The Health Care of the Older population implemented core and characteristically accessible services for the older population. However, older individuals face challenges and are not informed of these issues, preventing them from receiving advice on how to resolve them.42) Table 1 briefly summarizes the issues faced by older adults.
COVID-19 and Care of the Older Population
Since the spread of coronavirus disease 2019 (COVID-19) worldwide, there has been a boom in polypharmacy in the senior population. This exponential rise has made the older population more vulnerable to the side effects of many medications. The imperative for a multidisciplinary approach is a focus on effective medicine prescriptions, which encompasses all stakeholders, healthcare professionals, and other personnel.43)
Stress Reduction in the Geriatric Population
The Common Yoga Protocol launched by the Ministry of AYUSH of the Government of India provided guidelines for practitioners treating COVID-19. Studies have shown that yoga reduces the incidence of acute respiratory infections. Thus, yoga may benefit the psychosocial treatment and rehabilitation of patients with COVID-19 under quarantine and isolation to reduce anxiety and phobias in this population.44)
Polypharmacy in the Older Population
The negative effects of polypharmacy include death, falls, bad medication reactions, extended hospital stay, and hospital readmission soon after discharge.45,46) Increasing drug prescriptions increase the risks of side effects and injury.47) Numerous variables, such as drug-drug and drug-disease interactions, may cause harm. Owing to their lower lean body mass and diminished hearing, eyesight, cognition, and mobility, older people are at increased risk of negative side effects.48) Rather than a mere numerical count of medications, which has no practical relevance, studies have advised the use of the phrase “appropriate polypharmacy” to distinguish between “many” and “too many” medications.49) A universally accepted definition of polypharmacy is required.50)
Diseases and Biological Variations in Older Populations
India is experiencing a high non-communicable disease burden and lifestyle-related consequences.51,52) Healthy life in the older population includes refraining from tobacco or alcohol use, regular physical work, and consuming healthy products to help reduce communicable and non-communicable diseases, which ultimately decreases dependency on care in old age.53) At the cellular level, molecules and cells mutate with age. Aging causes physical and mental decline, as well as increased risks of various illnesses and death.
Variations
Biological variations and circumstantial modifications, such as retirement, pension, new housing, family support, death of partners and friends, food, and security, are also linked with aging. Geriatric syndromes are characterized by frailty, urinary incontinence, delirium, dementia, pressure ulcers, and falls. Common conditions include osteoarthritis, cataracts, refractive errors, diabetes, stroke, hypertension, asthma, chronic obstructive pulmonary disease, hearing loss, back and neck pain, depression, and cancer.3,54) In India, potential health disparities occurring among older adults are related to their economic class and require appropriate interventions to formulate actions to supervise achievements.55,56)
The NPHCE
This program was initiated in 2010 to address the many health-related challenges faced by the older population. With the enunciation of the UN Convention on the Rights of Persons with Disabilities, the National Policy on Older Persons, and the Maintenance and Welfare of Parents and Senior Citizens Act 2007, Section 20, the Ministry of Health and Family Welfare envisioned this program. The goal was to develop a facility entirely dedicated to adults aged 60 years and above. However, these schemes have not been extensively analyzed to determine the increasing health burden of senior citizens in India.57-59) The 12th Five Year Plan covered around 100 districts each year and established 12 more regional geriatric centers in the chosen medical tertiary care hospitals nationwide.60)
NPHCE vision and strategies
The vision of the NPHCE is to facilitate the best long-term comprehensive and dedicated services for active and healthy aging by making society affordable and accessible to the aging population. Table 2 specifies the NPHCE strategies required to implement the program for delivering better healthcare delivery to the older population.15,35)
All strategies were guided by state- and national-level governments at various levels of the healthcare system.61)
Schemes and Programs of the Government of India for the Welfare of the Older Population
The Ministry of Social Justice and Empowerment is a key ministry for senior welfare. The Ageing Division of the Department of Social Justice and Empowerment’s Social Defence Bureau is responsible for implementing policies and initiatives. The projects included help from the government, non-governmental organizations (NGOs), Panchayati Raj Institutions, local governments, and the general public. The policies implemented by the government also promote voluntary organizations to enhance support for family care and assistance to vulnerable individuals.2,62)
An integrated program for older adults
The main goal is to improve the quality of care and provide justified shelter, food, and medical care to encourage productive active aging.63) The agencies listed include Panchayati Raj or local bodies, NGOs, government-established autonomous bodies, and charitable trusts (Nehru Yuvak Kendra Sanghathan).
The national policy for older persons (1999)
This policy works with the assistance of the state to support and ensure the well-being of older adults. The policy’s goal is to safeguard older persons from exploitation and abuse, while also allowing them to flourish by providing money, food stability, and housing. It also aims to build the best healthcare system to encourage self-sufficiency in this population. New amendments are in the process of finalization according to data.
Maintenance and Welfare of Parents and Senior Citizens Act (2007)
This act was based on the requirements of parents and older adults, as well as their prosperity. This act was not implemented in Jammu and Kashmir states, Himachal Pradesh, as these states have their own acts. Since the last decade, there has been a need to work on the provisions implemented nationwide with an aim for modernization. In 2019, the bill was amended in Lok Sabha of this Act, which included the definitions, monetary rewards, family maintenance amounts, and nodal officers for senior citizens in every police station.34) In 2002, the Act was amended to state that older adults have the right to appeal for their necessities.54)
Rashtriya Varishth Jan Swasthya Yojana (RVJSY)
This scheme provides government health insurance to families below the poverty line nationwide. AIIMS, New Delhi, and Madras Medical College, Chennai, are two National Centers for Aging (NCAs), where the NPHCE is conducted through the Centre for Health Informatics (CHI) to deal with data on geriatric facilities across the country.
Pradhan Mantri Jan Arogya Yojana (PM-JAY)
The Ministry of Health and Family Welfare, which is affiliated with Ayushman Bharat and the National Health Authority, has been approved to implement Ayushman Bharat (PM-JAY) nationwide, which is the second component under Ayushmann Bharat which was launched in 2018. It aims to cover approximately 50 crore (500 million) beneficiaries (vulnerable and poor families). Through the nation's public and private empanelled hospitals, it offers a health cover of Rs. 5 lakhs (500,000 rupees) per family per year for secondary and tertiary care hospitalization. Health benefit packages 2.0 covers 867 packages and is split across 1,573 procedures. There were no constraints on family size, age, or gender. The public sector continues to play an important role, particularly in the neglected areas of India.64,65) The initiative has also aided in the management of this issue by encouraging COVID-19 worker transportation in various sections of the country.66)
Indira Gandhi national old age pension scheme
The Indira Gandhi National Old Age Pension Scheme (IGNOAPS) was launched by the Indian Ministry of Rural Development under the National Social Assistance Program (NSAP) in 2007. It features senior citizens of India receiving monthly pensions and no contribution required from pensioners. People aged 60 to 79 years will be provided with a monthly pension of Rs. 200 and older adults above 80 years will receive Rs. 500 per month as a pension. States were asked to provide the same level of help as the central government. The eligibility criteria for the scheme were men and women adults aged 60 years and above.
The Pradhan Mantri Vaya Vandana Yojana (PNVVY)
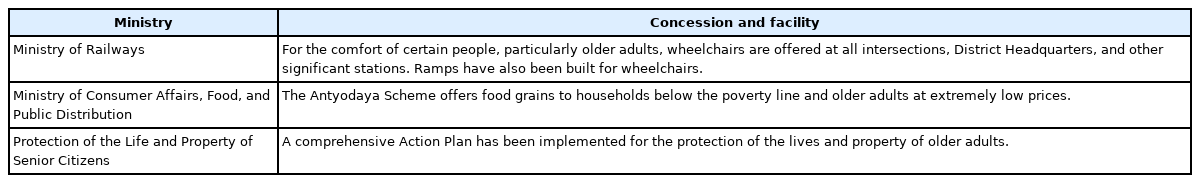
The PNVVY was launched in 2017 exclusively for people older than 60 years of age. The scheme was extended until March 2023, with an association with the Life Insurance Corporation of India. This insurance scheme has been in place for 10 years, with the amount of insurance ranging from Rs. 162,162 to Rs. 1,500,000, which is paid monthly, quarterly, half-yearly, and annually. Other ministries, such as the Ministry of Finance, the Ministry of Road Transport and Highways, the Ministry of Railways, and the Ministry of Consumer Affairs, Food, and Public Distribution, also provide schemes to support older adults and make them self-sufficient. Table 3 shows other ministries implemented provisions considering health in the country.
Other plans and initiatives
Other plans and initiatives include the National Action Plan for the Welfare of Senior Citizens (NAPSrC), the Scheme of Integrated Programme for Senior Citizens, the State Action Plan for Senior Citizens, the Convergence with Initiatives of other Ministries/Departments in Government of India in the field of Senior Citizens Welfare (CWMSrC), National Awards for Senior Citizens-Vayoshreshtha Samman, the Rashtriya Vayoshri Yojana: Scheme for Providing Physical Aids and Assisted-Living Devices for Senior Citizens, and the Senior Citizens Welfare Fund, which provides provisions, programs, schemes, and Walkathons mostly on October 1 every year in India. All these schemes and programs have the same goals to protect and secure the lives of senior citizens, with an enhanced approach to hospitalization and greater financial security.
Packages of Services Provided to Older People under the NPHCE
(1) Subcenters (SCs): Provide services for healthy aging education by experts and routine domiciliary visits with family education to maintain the health of bedridden or older adult patients who are disabled. They also provide suitable supportive devices from the primary health center to allow older patients to be ambulatory and run operational support groups in their localities.
(2) Primary health center (PHC): Provide a weekly geriatric clinic managed by a trained medical officer who maintains the records of the visit in a standard format provided by the government of India. PHCs conduct routine check-ups with basic clinical examinations, such as eye examinations, blood pressure, and blood sugar check-ups. In addition, free medicines are provided, with appropriate advice on chronic diseases. PHCs also raise health awareness and offer rehabilitation in health and village sanitation camps or days. Referral services are also provided to CHCs or district hospitals (DHs) as per requirements.
(3) Community health center (CHC): CHCs are considered the first referral unit from the PHC and lower levels. CHCs also implement two weekly geriatric clinics with physiotherapy and counseling units for older persons. The other provided services include domiciliary visits for bedridden patients and referrals to DHs.
(4) NCA: NCAs involve multidisciplinary clinical services of medical and surgical disciplines. They also provide day-care services with special clinics, such as memory/fall/syncope/frail/implants and cosmetic clinics. A special focus on patients aged 75 years and above is given to intensive care services and acute rehabilitation.
Thus, the NPHCE provides different levels of service packages. The program constitutes an integrated program in conjunction with the National Rural Health Mission and State and District Health Societies.
Dedicated Geriatric OPD Services under the NPHCE
While India has implemented numerous programs aimed at the senior population in recent decades, geriatric health clinics, geriatric physicians, and caregivers remain insufficient to provide proper care for older adults. Long-term care for older adults with physical and mental issues is referred to as geriatric or older adult care. Outpatient department (OPD) care is one of the most important and highly recommended services at all levels of the health care delivery system. Geriatric OPD is still in its infancy in India; however, a national survey showed that more than 80% of medical professionals and interns reported a need for specialized OPDs for geriatric services.67)
(1) DHs: Provide regular dedicated OPD for the older age group with facilities for labs and investigations for ailments and routine check-ups. DHs consist of 10 bedded geriatric wards covering specialties such as medicine, orthopedics, and ophthalmology for acute and chronic ailments. Patients referred from PHCs and CHCs are treated, and camps are also conducted for screening. From DHs, patients with severe cases are referred to tertiary hospitals.
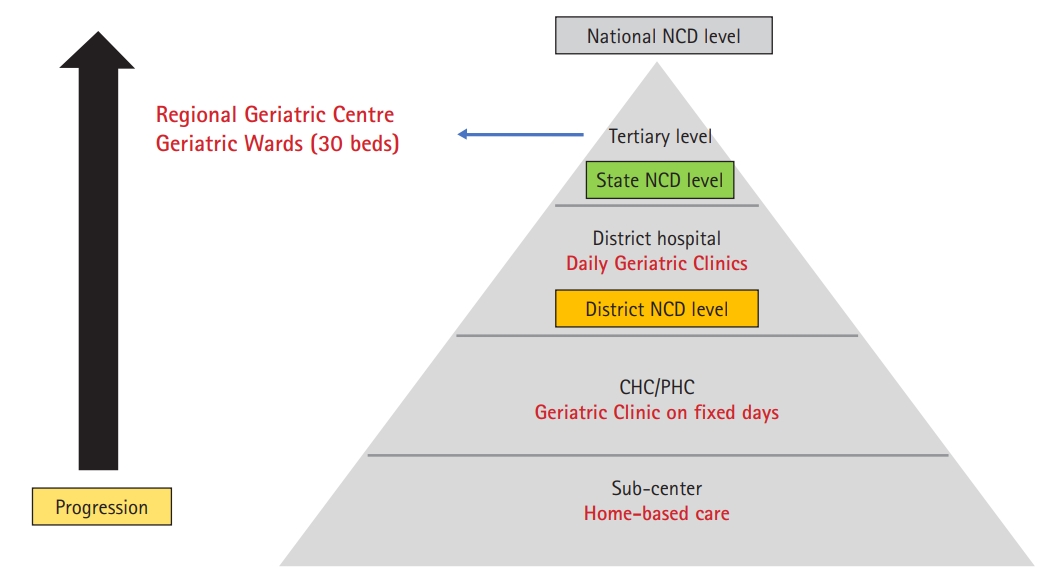
(2) Regional geriatric center (RGC): These specialized OPDs include 30 beds for geriatric inpatient wards, including departments such as medicine, neurology, surgery, urology, and psychiatry, and laboratory facilities with special collection centers. Patients are referred from medical colleges, DHs, and below.
Comprehensive geriatric outpatient care offers older adult patients a thorough treatment plan and access to social services, which lowers the demand for medical resources.
Achievements in the implementation of the NPHCE6)
(1) The development of primary and secondary geriatric care services in all districts: One hundred districts were sanctioned for NPHCE services during the 11th plan period, while 421 districts were sanctioned to provide specialized geriatric OPD, inpatient department (IPD), physiotherapy, and lab services during the 12th plan period. All 713 districts were sanctioned for geriatric primary and secondary care services, including OPD, IPD, physiotherapy, and laboratory services, with the remaining 114 districts sanctioned in 2019–2020.
(2) Tertiary-level activities of the NPHCE: The “Rashtriya Varisth Jan Swasthya Yojana” (2016–2017)—NPHCE has sanctioned 19 RGCs at selected medical colleges in 18 states to provide tertiary care services in the form of specialist OPDs, 30-bed wards in RGCs, including earmarked beds in various specialties such as urology, orthopedics, and ophthalmology as well as personnel development and research activities. Currently, 18 RGCs provide outpatient treatment, 16 RGCs provide inpatient services, 14 RGCs provide physiotherapy, and 13 RGCs provide laboratory services. Two NCAs have also been established as Geriatric Care Centers of Excellence. A 200-bed NCA has been built and is active in the COVID ward at Madras Medical College in Chennai, while another NCA is under construction at AIIMS in New Delhi.
(3) Comprehensive geriatric care training modules: Three sets of training modules for medical officers, nurses, and community-based workers were established to provide comprehensive geriatric care. Chhattisgarh, Meghalaya, Haryana, and Punjab have held state-level training of the trainers of medical officers for comprehensive geriatric care. Tamil Nadu and Maharashtra produced approximately 236 state-level master trainers and 85 national master trainers, including 27 medical officers, 26 staff nurses, and 32 community-based workers.
(4) NPHCE website (https://main.mohfw.gov.in/major-programmes/Non-Communicable-Diseases/Non-Communicable-Diseases-1): This website provides detailed information about geriatric facilities and services via the CHI as the management information system.
(5) Information and education communication: Awareness of the myths, stereotypes, and social stigma is the most important step and makes stakeholders cognizant of geriatric care. Audio/video data are used for the geriatric age group. Other materials, including hard copy material and posters, should be available in English, Hindi, and all other regional languages.
(6) Monitoring and evaluation/audit: At all levels, the Union Ministry of Health and Family Welfare, as well as the Directorate General of Health Services, will continue to monitor and assess the program. Implementing World Health Organization’s “Age-Friendly Primary Health Care Centres Toolkit” will assist persons of all ages to improve the quality of their care.68) Village panchayats work best in monitoring health service delivery and also assist in planning reproductive and child health services.69,70) The knowledge gap can also be addressed by enhancing communication between stakeholders.71)
Advancements in the operationalization of programme activities, 2020–2021
According to the Progress Report, between April and December 2020, 19 RGCs, 18 operational OPD, 16 indoor wards, 14 physiotherapy services, and 13 laboratory services were sanctioned. A total of 718 DHs were sanctioned by the government, in addition to 584 operational OPDs, 507 indoor wards, 445 physiotherapy service units, and 539 laboratory services. A total of 4,869 CHCs were sanctioned, with 3,111 operational OPDs; however, no indoor wards were operational. Physiotherapy and laboratory services accounted for 1,131 and 2,408 units, respectively. A total of 18,407 PHCs were sanctioned, including 10,180 operational OPDs; however, no provision for indoor wards, physiotherapy, and laboratory services units was reported.
Provision of geriatric care services, 2019–2020
The Annual Progress Report from April 2019 to March 2020 listed nine services: OPD care services, indoor admissions, physiotherapy care, lab tests, number of older adults screened and given a health card, number of older adults provided home care services, number of older adults provided supportive devices, cases referred, and cases died in the hospital. These services were divided into RGCs, DHs, CHCs, PHCs, and SCs. Thus, the 133,545 OPD care services were provided in RGCs, 7,567,744 in DHs, 7,016,670 in CHCs, 9,032,922 in PHCs, and 2,843,211 in SCs, totaling 26 million. The total of 0.96 million indoor admissions included 9,992 in RGCs, 688,966 in DHs, 269,286 in CHCs. The 1.5 million physiotherapy care units comprised 34,637 in RGCs, 754,186 in DHs, and 2,348,922 in CHCs. The 9.07 million laboratory testing services included 230,749 in RGCs, 4,215,883 in DHs, 2,348,922 in CHCs, and 2,275,600 in PHCs. The 0.24 million older adults who received home care services included 11,157 in DHs, 92,657 in CHCs, 68,674 in PHCs, and 68,783 in SCs. The 0.047 million older adults who received supportive devices included 4,820 in DHs, 18,006 in CHCs, 7,256 in PHCs, and 17,502 in SCs. The 0.22 million referred case included 32,017 in DHs, 59,202 in CHCs, 65,057 in PHCs, and 64,119 in SCs. The 0.019 million deaths in hospitals included 17,026 in DHs, 2,156 in CHCs, and 384 in PHCs.
The expected outcomes of the NPHCE focus on most health issues.72,73) Fig. 1 illustrates the implementation of the NPHCE in India.74)
Human resource development
The Medical Council of India announced 15 MD geriatric medicine seats as a curriculum. This course provides more insights into geriatric care. Over 3,000 doctors have been trained and have provided service to geriatric patients in diverse areas for >16 years. NCAs were created in AIIMS, New Delhi, and Madras Medical College, Chennai, as part of the NPHCE, with key duties including interdisciplinary team training, research, and healthcare delivery in the field of geriatrics.75)
Training manual for medical officers for older adult care
The care of older individuals requires a holistic approach, which is addressed in this training module. The manual outlines the components of geriatric evaluation, including physical, mental, psychological, and socioeconomic aspects, as well as comorbidity profiles, diet, and medical utilization.76)
Concerns regarding Tribal Populations
With 8.6% of the population being tribal, India faces challenges in closing the healthcare gap between tribal and nontribal residents. The current scenario inevitably results in lower levels of economic achievement,78) with only 56% of children receiving all recommended vaccinations, as evidenced by an infant mortality rate of 44.4% and an under-5-year mortality rate of 57.2%.79) Additionally, 11% of the tribal population believes that nobody can stop diseases since it is God’s will. Other research suggests that this population believes that sickness is caused by hostile spirits, ghosts, breaking certain taboos, and godly curses.80) One of the most important challenges in providing healthcare for the tribal population is ensuring timely access. Older adults are more vulnerable to health conditions with multiple comorbidities. Hence, it is essential to work on the reorganization of service delivery mechanisms in tribal areas. A recent tribal India report suggested offering a broader range of 15 types of services, including geriatric and palliative healthcare services, through tribal health and wellness centers.79)
Healthcare delivery to isolated older adults in such tribal settings can be aided by medical outreach camps and mobile health clinics. The attendance of tribal older people at health facilities may be increased by offering emergency transportation, hiring health workers from tribal communities, and establishing tribal counselors who make weekly visits to tribal hamlets to raise awareness of health issues and encourage healthy behaviors.81)
Ongoing Research
Longitudinal Ageing Study in India (LASI)
In 2016, the Ministry of Health and Family Welfare in India began a country-level scientific review of health, economic, and social factors, and the aftereffects of India’s aging population of 45 years and older. The International Institute for Population Sciences (IIPS) Mumbai was maintained as India’s National Nodal Agency for the LASI survey. Technical support for Wave I of LASI was provided by the Harvard T.H. Chan School of Public Health (HSPH) and the University of Southern California.6,82,83)
LASI Initiation
Wave I of the LASI was conducted from April 2017 to December 2018 and enrolled 72,250 older adults. The LASI includes data from four domains: health, health care and health care financing, social, and economic. The findings of Wave I were released on January 6, 2021.25,84,85) Table 5 specifies the goals for conducting the longitudinal aging study in India. The LASI is the largest global longitudinal aging study in terms of sample size, providing comprehensive and internationally comparable high-quality scientific data on the overall well-being of older adults in India. The LASI involves 30 states and 6 union territories, which cover 640 districts.
The LASI gathers information on four important subject areas76):
(1) Disease burden and risk factors in health (reported and measured).
(2) Healthcare and healthcare financing.
(3) Social: programs for older persons in the family, social networks, and social welfare.
(4) Economic: earnings, wealth, spending, employment, retirement, and pension.
A multivariate decomposition analysis of LASI data among older adults in 2017–2018 reported that older women are the highest priorities for health care professionals and necessitate the early prediction of disability, as well as the preservation of daily functioning.86) The initial findings of the LASI revealed that older Indians face a wide range of health, social, and financial insecurities, with significant heterogeneity across several dimensions.87)
CONCLUSION
While the NPHCE is a good initiative, it requires more monitoring and increased involvement of policymakers and stakeholders. These efforts are helping to develop a universal, accessible, and affordable long-term care service system with high-quality upstream prevention to postpone impairment and offer support services for family caregivers. The NPHCE prepares families for the worst circumstances and constructs a framework for each family to become a valuable participant in such programs. Public health measures could provide better national transport systems, provide buildings designed for the old people, adapt the course of the nature of the life cycle of older adults, and create a space for the psychological growth of newly experienced ideas.
This can be achieved through the education of health professionals, routine health check-ups, centralized specialized geriatric OPDs, and support and funding from the government at every level of the healthcare delivery system. Boys and girls from tribal communities with little formal education can be educated as community health workers and encouraged to work in their local neighbourhoods. LASI has performed a comprehensive nationwide study of the health, economic, and social factors, and implications of India’s population ageing. It is necessary to look forward to preventing communicable and non-communicable diseases at each healthcare level. Efforts should be made in line with family support, social well-being, and measures to address psychological issues. Providing corporate statutes to geriatric healthcare services will galvanize the healthcare delivery system and encourage healthy ageing.
Notes
CONFLICT OF INTEREST
The researchers claim no conflicts of interest.
FUNDING
None.
AUTHOR CONTRIBUTIONS
Conceptualization, LMV, SHJ; Data curation, LMV, SHJ; Investigation, LMV, SHJ; Methodology, LMV, SHJ; Project administration, SHJ, AUJ; Supervision, AUJ, AMM; Writing–original draft, LMV, SHJ; Writing–review & editing, LMV, SHJ, AUJ, AMM.