Atypical Presentation of Pill Aspiration in Older Adults with Dysphagia: A Picture Not To Be Forgotten
Article information
Abstract
Nonconventional clinical presentations of diseases are common in older adults. Even dramatic events, such as foreign body (FB) inhalation, can occur in a subtle and non-specific manner. Pill aspiration is a rare yet overlooked cause of airway injury. It accounts for approximately 7% of all FB aspirations. In contrast, oral dysphagia and polypharmacology, mainly administrated in solid oral dosage forms (SDOF), like tablets and pills, are common conditions in older adults. Herein, we present a case of SDOF aspiration in a 78-year-old man. FB inhalation developed with general clinical deterioration and neurological impairment (delirium) rather than overt respiratory symptoms. Bronchoscopy provided remarkable images of this unexpected finding. Caregivers and healthcare workers must be aware of the risk of SDOF aspiration and adopt proper safety measures. Early recognition and bronchoscopy for diagnostic and therapeutic purposes can be lifesaving in such cases.
INTRODUCTION
Pill aspiration is a rare yet overlooked cause of airway injury. It represents 7% of all foreign body (FB) aspirations in adults.1) In contrast, oral dysphagia and polypharmacology are common conditions in older adults. Drugs are mainly administered in solid oral dosage forms (SDOF), such as tablets and pills. Diagnosing pill aspirations presents many challenges. For example, clinical and radiological findings can be subtle and non-specific. Moreover, the suspicion of SDOF causing airway injury is often low-grade. Finally, pills may dissolve into the airways; thus, they are not observed during bronchoscopy.2) Herein, we present a case of pill aspiration in a 78-year-old man with an elusive clinical presentation. Pictures from the bronchoscopy of this patient raise a concern about the risks associated with the use of SDOF in older adults with oral dysphagia. Written informed consent was obtained from the patient for publication of this case report and accompanying image.
CASE REPORT
A 78-year-old man was admitted to our geriatric internal medicine ward with multiple spontaneous bone fractures due to metastasis of cancer of unknown primary origin, severe clinical deterioration, and delirium. The patient had a history of heavy smoking (approximately 80 pack-years). No other diseases were known, mainly because of poor medical supervision.
His relatives reported that he was quite well until approximately 20 days before hospitalization. Previously, he started presenting with widespread bone pain. An X-ray scan revealed multiple spontaneous pathological bone fractures. He had started taking painkillers (first paracetamol, then oxycodone and naloxone), and a computed tomography (CT) scan was scheduled. However, in the following days, he started presenting with clinical deterioration and sudden worsening of neurological signs. After a non-traumatic fall, relatives brought him to the emergency room (ER).
The patient presented with severe clinical deterioration upon arrival. He was agitated, disoriented, and unable to maintain attention. He was eupnoeic in room air at a temperature of 36°C and had a blood pressure of 130/80 mmHg. Brain CT did not reveal intracranial hemorrhage. Chest radiography (Fig. 1) showed abnormal elevation of the left hemidiaphragm and reduced transparency of the corresponding lung due to possible atelectasis, with abundant pleural effusion on the left side. The levels of blood inflammation markers were elevated, likely due to current acute infection (leukocytes 21.33×109/L with 88.3% neutrophils, C-reactive protein 234.0 mg/L); therefore, antibiotic therapy was initiated.

Chest radiography showed abnormal elevation of the left hemidiaphragm and reduced transparency of the corresponding lung due to possible atelectasis, with abundant pleural effusion on the left side.
On the following day, the patient was transferred to our hospital. He was eupnoeic in room air upon arrival. Physical examination of the lungs showed diminished breath sounds, especially on the left lung base, diffused rhonchi, and wheezing, mostly on the left side of the chest. The patient was heavily sarcopenic. Arterial blood gas showed hypoxemic respiratory failure (pH 7.48, PaCO2 45.7 mmHg, PaO2 53.6 mmHg, sO2 87.9%, lactates 1.7 mmol/L, HCO3– 33.1 mmol/L).
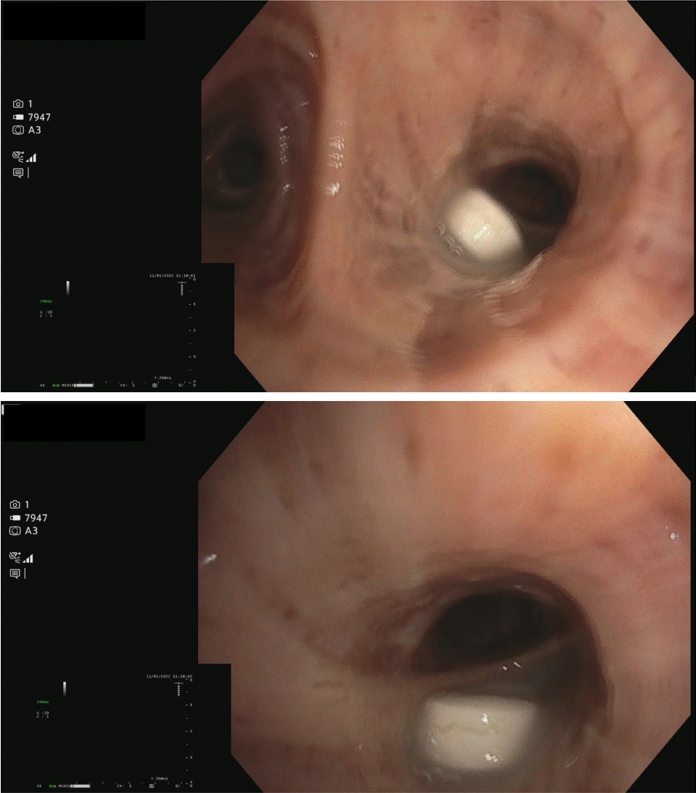
Chest CT showed that the left lung had collapsed due to airway occlusion. Bronchoscopy performed the next day unexpectedly showed a pill occluded the left mainstem bronchus (Fig. 2). Its size and appearance suggested an intact paracetamol pill. In addition, X-ray imaging performed on arrival showed lung atelectasis. For these reasons, we believed that aspiration had occurred several weeks before his hospitalization, at the beginning of his pain management therapy.
The FB was successfully removed during the procedure; however, the patient died due to pulmonary infection and respiratory failure the next day.
DISCUSSION
We report the case of a 78-year-old patient who experienced pill aspiration, characterized by atypical clinical manifestations.
Unconventional clinical presentations are common in older adults. However, in this case, FB aspiration developed with general clinical deterioration and neurological signs and symptoms (delirium) rather than overt respiratory symptoms such as dyspnea.
Oral dysphagia is a common geriatric syndrome (10%–33%).3) It is associated with a high burden of mortality and morbidity in older adults, mainly due to dehydration, malnutrition, and infection. The swallowing process has two important and complementary functions: ingestion of food and airway protection.4,5) Swallowing problems are often comorbid with various conditions such as neurological diseases (e.g., Parkinson disease and Alzheimer disease), musculoskeletal conditions, cancer, and sarcopenia. They may also occur when stressors (i.e., infections, drugs, hospitalization) disrupt the delicate balance of frail older adults. Moreover, the aging population experiences a physiological reduction in swallowing function referred to as presbyphagia.6)
In older adults, managing dysphagia is crucial when administering medical therapy. According to the SHELTER study, nearly 50% of older adults in nursing homes across Europe take 5–9 drugs, while 24.3% take ≥10 drugs.7) Difficulties in swallowing SDOFs may affect not only older adults with overt dysphagia (45.5%) but also those with presbyphagia or even no dysphagia (12.3%).8) FB aspiration can also occur “silently” without any clinical evidence of swallowing difficulty. Older age and common geriatric conditions (e.g., cerebrovascular impairment, diabetes, previous myocardial infarction, and chronic obstructive pulmonary disease) are risk factors associated with silent aspiration.9) Although the relatives in the present case reported that the patient was independent in activities of daily living (ADL) and did not suffer from symptomatic oral dysphagia before the worsening of his clinical condition, he had risk factors that made his swallowing function highly vulnerable, such as age-related paraphysiological changes, sarcopenia, active cancer, and probable chronic obstructive pulmonary disease.10)
SDOF can cause airway inflammation, obstruction, and systemic toxicity.1) The time course of obstruction before an intervention can vary from days to months. Studies have highlighted the importance of early recognition and bronchoscopy for diagnosing and treating SDOF aspiration.11)
Oral drugs are often administered in geriatric healthcare settings by crushing tablets or opening capsules and dispersing powders in water or gel. This represents the off-label use of the medication, which may negatively impact both efficacy and safety.12) A possible solution to this problem is the implementation of alternative formulations, such as orally disintegrating tablets13) or dispersible formulations. Some drugs are already available in “dysphagia-friendly” formulations. For many others, however, further investigation by geriatric pharmacology and investments are needed.
The risks associated with SDOF in older adults support calls to action for deprescribing, as this can help in two ways. First, some drugs are involved in swallowing disorders by causing esophageal injuries, xerostomia, and dysphagia.8) Second, reducing the number of medications can also reduce the probability that tablets and capsules may “go down the wrong way.”
Safety measures to prevent FB aspiration involve appropriate rest between swallows, adjusting posture, placing the pill or tablet in the patient’s mouth according to the type of deficit, swallowing rehabilitation, and minimizing the use of hypnotics and sedatives.14,15) In addition, managing and preventing sarcopenic dysphagia in hospitalized and bedridden patients may be useful.16)
It is crucial for all caregivers and healthcare workers to be aware of the possible risks related to SDOF aspiration in older adults with dysphagia and to adopt appropriate safety measures. The consequences of FB inhalation can be fatal. However, when they occur, the ability to recognize them and proceed with proper management can be lifesaving.
Notes
CONFLICT OF INTEREST
The researchers claim no conflicts of interest.
FUNDING
None.
AUTHOR CONTRIBUTIONS
Conceptualization, FL, VB, SC, CC; investigation, VB, CAM, SC, CC, CR, CM, GG; project administration FL; supervision, FL, MT, VB; visualization, SC; writing-original draft, SC; writing-review & editing, SC, MT, RC, DE. All authors read and approved the final version.