Optimal Cut-Off Points of 4-meter Gait Speed to Discriminate Functional Exercise Capacity and Health Status in Older patients with Chronic Obstructive Pulmonary Disease
Article information
Abstract
Background
Gait speed, a vital sign of health and functional capacity, is commonly used to measure mobility. Although studies have assessed gait speed in older adults and individuals with chronic obstructive pulmonary disease (COPD) separately, few have evaluated gait speed in older adults with COPD. Therefore, the primary objective of our study was to determine the threshold point for the 4-meter gait speed test (4MGS) to better discriminate between functional exercise capacity and health status in older patients with COPD. The second objective was to determine possible predictors of gait speed.
Methods
In this cross-sectional study, we assessed participants’ pulmonary function, dyspnea, health status (COPD Assessment Test [CAT]), gait speed (4MGS), functional exercise capacity (6-minute walk test [6MWT]), and physical activity.
Results
Forty-five older patients with COPD participated in this study. The predicted 6MWT and CAT scores were independent and significant determinants of the 4MGS score, explaining 54% of the variance (p<0.001). We identified gait speeds of 0.96 m/s and 1.04 m/s as thresholds to predict abnormal functional exercise capacity (sensitivity 85% and specificity 56%) and impaired health status (sensitivity 90% and specificity 69%), respectively (p<0.05).
Conclusion
Our findings demonstrated that gait speed can discriminate between abnormal functional exercise capacity and impaired health status in older patients with COPD. Moreover, functional exercise capacity and health status are predictors of gait speed.
INTRODUCTION
Chronic obstructive pulmonary disease (COPD), a major global burden, is an inflammatory lung disease that causes respiratory difficulties and airflow limitations.1) Age and COPD prevalence are directly related, making COPD a prominent health problem among older adults.2) Age-related anatomical and physiological changes in the cardiorespiratory system result in high mortality in this population.3) COPD at older ages further impairs physical well-being and leads to functional disability.4)
Low gait speed is also a serious risk factor for cardiovascular and all-cause mortality in community-dwelling older individuals.5-7) Additionally, gait speed is a marker of functional exercise capacity in both patients with COPD and older adults.5,8) Gait requires complex integration and interaction between motor, sensory, and cognitive systems.9) Gait speed, the vital sign of health and functional capacity, is commonly used to measure mobility.9) Lower gait speed is an indicator of impairment, especially in chronic respiratory diseases.10) The 4-meter gait speed test (4MGS) is a valid and reliable test to assess gait speed in patients with COPD.11)
Although studies have assessed gait speed in patients with COPD and older adults separately, few have assessed the combination of these factors. Determining the optimal cut-off scores and predictors of 4MGS will contribute to literature and is important for understanding the possible effects of both aging and COPD. Moreover, despite the importance of gait speed in older adults with COPD, literature on the threshold points for gait speed to discriminate between functional exercise capacity and health status is also lacking. Therefore, the main purpose of the present study was to determine the cut-off point for the 4MGS to better discriminate between functional exercise capacity and health status in older patients with COPD. The second purpose was to determine possible predictors of gait speed in this patient population.
MATERIAL AND METHODS
Study Design and Participants
This cross-sectional study included 45 older patients (aged ≥60 years) with COPD. An experienced specialist diagnosed COPD according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines. Patients who (1) were clinically stable, (2) were not receiving any antibiotic treatment, and (3) had followed the same medication regimen for at least 3 weeks were included in the study. We excluded clinically unstable patients or those with musculoskeletal, neurological, or cardiovascular diseases that could hinder assessments.
This study complied the ethical guidelines for authorship and pubhishing in the Annals of Geriatric Medicine and Research.12) The study protocol was approved by Selcuk University, Faculty of Health Sciences Ethics Committee (No. 2021/857). The study adhered to the principles of the Declaration of Helsinki, and all participants provided written informed consent.
Outcome Measures
According to the European Respiratory Society (ERS) and American Thoracic Society (ATS) guidelines, we used a spirometer (Quark-SPIRO; COSMED, Roma, Italy) to evaluate pulmonary function,13) including forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1), and FEV1/FVC.
We used the modified Medical Research Council (mMRC) Dyspnea Scale to assess dyspnea during certain daily activities. This self-administered tool measures the level of difficulty attributable to dyspnea in daily life. The scale has five expressions covering the entire range of dyspnea from no limitations (level 0) to full capacity insufficiency (level 4).14)
We used the COPD Assessment Test (CAT) to assess symptoms and effect of COPD on the health-related well-being of individuals. This reliable and valid tool has eight items, and the score for each range from 0 to 5 (maximum total score=40), with higher scores indicating higher symptom burden.15,16) The GOLD guidelines define a CAT score ≥10 as “impaired health.”17)
We used the 4MGS to evaluate gait speed.11) Using floor marking tape, an 8-m-long hallway was divided into three zones: acceleration (2 m), testing (4 m), and deceleration (2 m) zones. The participants were asked to walk at their usual speed along the hallway, and the examiner recorded the total time from the start to the endpoint using a stopwatch. To calculate gait speed, the walking distance was divided by time.8)
We used the 6-minute walk test (6MWT) to assess functional exercise capacity, as indicated in the ERS and ATS guidelines. Each participant performed two 6MWTs with a minimum rest of 30 minutes.18) In each of the two tests, as the participants walked more, the value was recorded and expected walking percentage values were calculated. We recorded the longer of the two walking distances and calculated the percentage of predicted (%pred) values.19) The functional capacity of the participants was categorized as normal (≥82%pred) or abnormal (<82%pred).20) None of the participants had COPD requiring oxygen therapy during the tests.
We used the International Physical Activity Questionnaire Short Form (IPAQ-SF) to evaluate physical activity level in terms of gait and vigorous-to-moderate activities. We assessed the scale score by multiplying each activity duration by its known metabolic equivalents (METs).21,22)
Sample Size
We determined the minimum required sample size for multiple linear regression analysis using G*Power software (version 3.1.9.7; Heinrich Heine University, Düsseldorf, Germany) based on the results of a previous study, in which the 6MWT scores were a significant indicator of 4MGS scores in patients with COPD (R2=0.19).23) The results showed that at least 37 participants were required for eight determinants in the model (age, body mass index [BMI], predicted FEV1, mMRC score, CAT score, 6MWT distance, predicted 6MWT, and IPAQ-SF) (a probability level of 0.05, an anticipated effect size of 0.234, and a statistical power level of 80%).24)
Statistical Analysis
We used IBM SPSS Statistics for Windows (version 25.0; IBM Corp., Armonk, NY, USA) to analyze the data. Histograms and Shapiro-Wilk tests were used to check for normality. Values are expressed as median (interquartile range) and mean±standard deviation for continuous variables and as numbers for categorical variables.
To examine correlations between 4MGS and other variables, we used Pearson product-moment correlation coefficients. In addition, we applied stepwise multiple linear regression analysis to identify variables with the largest effect on 4MGS. We also created a regression equation for this study.
We applied receiver operating characteristic (ROC) curve analysis to assess the discriminative value of 4MGS for abnormal functional exercise capacity (6MWT predicted <82%) and impaired health status (CAT score ≥10).25) p-values <0.05 were considered statistically significant.
RESULTS
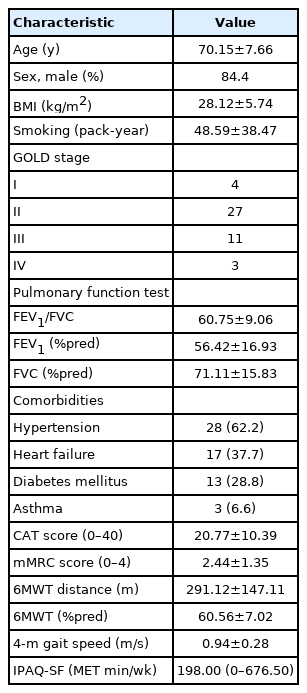
This study included 45 older adult patients with COPD (mean age, 70.15±7.66 years). Among all the patients, 84.4% were male. The participant characteristics are listed in Table 1.
4MGS was significantly correlated with predicted FEV1 (r=0.513), mMRC score (r=-0.586), CAT score (r=-0.630,), 6MWT distance (r=0.675), predicted 6MWT (r=0.709), and IPAQ-SF score (r=0.510) (p<0.001; Table 2).
The results of the stepwise multiple regression analysis revealed predicted 6MWT and CAT score as independent and significant determinants of 4MGS, explaining 54% of the variance (p<0.001) (Table 3). The regression equation formula was as follows:
4MGS = 0.791 + (0.005 × 6MWT predicted) + (-0.008 × CAT score).
4MGS had a discriminative value for abnormal functional exercise capacity, with an area under the curve (AUC) of 0.71 (p=0.030, 95% confidence interval 0.56–0.86). The 4MGS cut-off of 0.96 m/s had an 85% sensitivity and 56% specificity to predict abnormal functional exercise capacity (Fig. 1A).
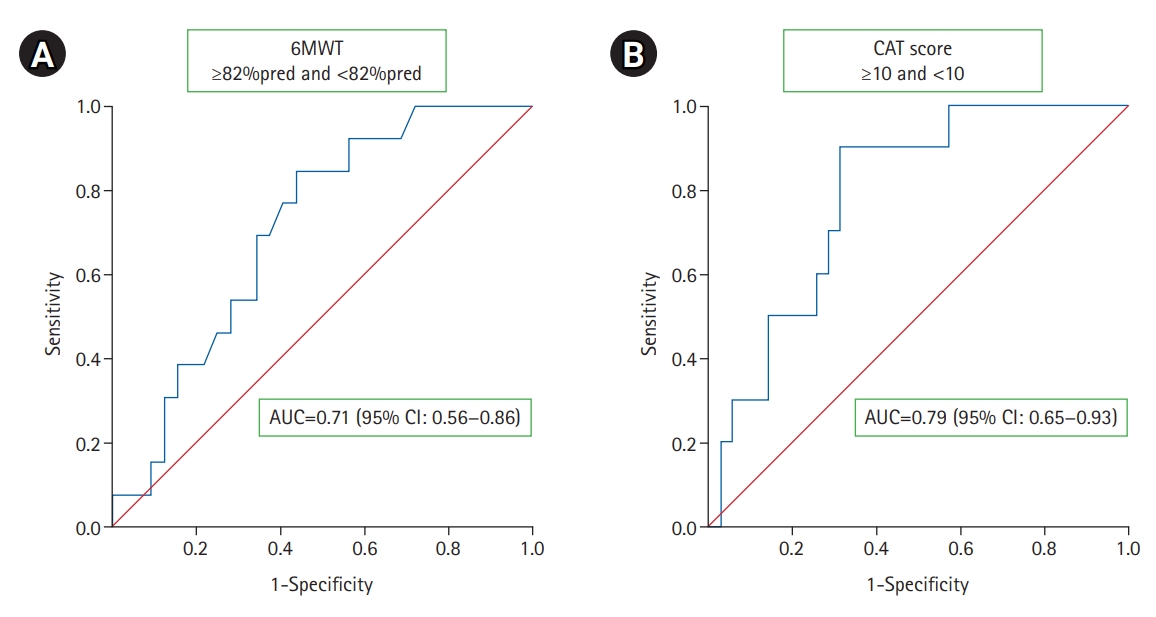
Receiver operating characteristic (ROC) curves for 4-meter gait speed cut-off point to discriminate functional exercise capacity and health status in older with chronic obstructive pulmonary disease. (A) 6MWT <82%pred and ≥82%pred (cut-off point 0.96 m/s; sensitivity 85%; specificity 56%; AUC=0.71, 95% CI 0.56–0.86; p=0.03). (B) CAT score ≥10 and <10 (cut-off point 1.04 m/s; sensitivity 90%; specificity 69%; AUC=0.79, 95% CI 0.65–0.93; p=0.006). 6MWT, 6-minute walk test; AUC, area under the ROC curve; CI, confidence interval; CAT, COPD Assessment Test.
4MGS had a discriminative value for impaired health status, with an AUC of 0.79 (p=0.006, 95% confidence interval 0.65–0.93). The 4MGS cut-off of 1.04 m/s had a 90% sensitivity and 69% specificity for determining impaired health status in the sample (Fig. 1B).
DISCUSSION
The leading finding of the study demonstrated that gait speeds of 0.96 m/s and 1.04 m/s were thresholds predicting abnormal functional exercise capacity and impaired health status, respectively. In addition, our results indicated that health status and functional exercise capacity were significant predictors of gait speed, explaining 54% of the variance in this population.
4MGS is a valid and reliable tool for patients with COPD,11) while gait speed is commonly considered a vital sign in the literature.26) Moreover, in chronic lung disease, mainly COPD, gait speed is related to pulmonary function,27) physical activity,28) dyspnea,29) functional exercise capacity,28) quality of life,27) and self-efficacy.28) Consistent with the literature, we observed correlations between gait speed and pulmonary function, dyspnea, health status, functional exercise capacity, and physical activity.
6MWT provides an objective evaluation of functional exercise capacity and is commonly used to assess patients with moderate to severe pulmonary diseases.30) Changes in 6MWT distance and other derived measurements can be used to determine treatment outcomes and predict mortality and morbidity in chronic respiratory diseases.18) Gait speed is a determinant of functional capacity in COPD.27) Our results demonstrated that functional exercise capacity is a factor influencing gait speed in older patients with COPD. These findings indicate that gait speed may be impaired in exercise-intolerant older patients with COPD.
COPD is related to impaired health status.31) The effect of COPD on patient health status can be assessed using the CAT.15) The CAT score is a determinant of functional exercise capacity,32) higher risk of exacerbation,33) and frailty34) in patients with COPD. We found that CAT was a determinant of 4MGS, indicating that impaired health status can cause a limitation in gait speed in this population. Improving patient health status can lead to increased gait speed.
Different 4MGS cut-off scores have been reported in the literature. Karpman et al.8) reported 0.8 m/s as a cut-off gait speed to predict abnormal exercise capacity in patients with COPD. Another study in the same population reported that a maximum gait speed of 1.27 m/s discriminated intact exercise capacity.35) A study of cardiac patients suggested a gait speed of 0.7 m/s as the cut-off to predict abnormal exercise capacity.36) Additionally, individuals with walking speeds >1 m/s were independent in activities of daily living (ADL), less likely to be hospitalized, and less likely to have an adverse event.26) Our findings showed that gait speeds of 0.96 m/s and 1.04 m/s were indicators of abnormal functional exercise capacity (sensitivity 85%, specificity 56%) and impaired health status (sensitivity 90%, specificity 69%), respectively, in older patients with COPD. The diversity in reported cut-off values may be because of differences in methodologies and sample populations. Differences in test administration strategies and reference values might be the underlying causes of discrepancies in the reported cut-off values.
This study had several limitations. First, although the study sample size was larger than the minimum required, most participants were in GOLD classes II and III. Thus, our findings cannot be generalized to all levels of COPD severity. The second limitation was the absence of an age- and sex-matched healthy control group. The inclusion of a control group in this study could provide a deeper and wider perspective. Third, we referred to values reported by Enright and Sherrill19) as the reference values for 6MWT were not validated in the Turkish population.
In conclusion, our findings indicated that gait speed could discriminate between impaired health status and abnormal functional exercise capacity in older patients with COPD. Moreover, functional exercise capacity and health status were independent determining factors for gait speed in this population.
Notes
CONFLICT OF INTEREST
The researchers claim no conflicts of interest.
FUNDING
None.
AUTHOR CONTRIBUTIONS
Conceptualization: IO, MIK, NZ, CK, AE; Data curation and Formal analysis: IO, MIK, NZ; Investigation and Methodology: IO, MIK, CK, AE; Project administration: IO, AE; Supervision: IO, MIK, NZ, CK, AE; Writing-original draft: IO, MIK, CK, AE; Writing-review and editing: IO, MIK, NZ, CK, AE.