The Impact of the Otago Exercise Program on Frailty and Empowerment in Older Nursing Home Residents: A Randomized Controlled Trial
Article information
Abstract
Background
This study assessed the impact of Otago exercises on frailty and empowerment in older nursing home residents.
Methods
This randomized controlled trial included 72 individuals aged over 65 years residing in a single nursing home in Izmir, Turkey. The participants were randomly assigned to the Otago exercise group (OEG) or control group (CG). The OEG performed Otago exercises for 45 minutes, 3 days per week for 12 weeks plus a walking program the 3 other days of the week. In addition to Otago exercise training, the OEG received training based on empowerment consisting of 10 sessions lasting 30 minutes each. The CG received no intervention except routine care in the nursing home. The data collected were sociodemographic characteristics, Edmonton Frail Scale (EFS) scores, and Elderly Empowerment Scale (EES) scores before and 3 months after the intervention.
Results
We observed significant differences between the mean EFS (p=0.0001) and mean EES (p=0.0001) before and 3 months after the intervention in the OEG compared to the CG. We also observed a significant difference between the OEG and CG in mean EFS (p=0.018) and EES (p=0.0001) 3 months after the intervention.
Conclusion
The results of the present study demonstrated the positive impact of the Otago exercise program on preventing/delaying frailty and enhancing empowerment in older people.
INTRODUCTION
Population aging is the most important medical, demographic, and social change of the 21st century and a public health phenomenon.1,2) Based on the Global Population Vision 2019, 703 million people are aged 65 years and over globally, accounting for 9% of the world’s population. The number of older people globally is estimated to reach 1.5 billion people by 2050.3) The aging trend continues rapidly in Turkey. According to the Turkish Statistical Institute (TUIK), in 2020, the older population has increased by 22.5% in the last 5 years, and older adults account for 9.5% of the total population.4) It has been observed that this increase is especially greater in people in the age range of 85 years and above. Aging is a multidimensional phenomenon that includes physiological, psychosocial, and biological changes.5) Aging is defined as a continuous process under cumulative, progressive, intrinsic, and deleterious factors.6,7) Frailty is an important concept in the science of aging and a very common aging syndrome.8) Frailty is defined as a state of increased vulnerability due to reduced physiological reserves and function in different organ systems when exposed to stress in individuals of the same chronological age. Frailty is strongly associated with negative outcomes such as disability, hospitalization, admission to the nursing home, and falls and death.9,10) Empowerment has become a common term in the health literature. Several definitions and approaches have been proposed for empowerment.11,12) According to the World Health Organization, empowerment is defined as individuals who and social process in which individuals have more control over decisions and actions that affect their health.13) Empowerment affects people’s participation in health behaviors, promotes autonomy and self-care behaviors, takes responsibility for their health, reduces healthcare costs, and improves general health.14-16) Purposeful empowerment in older people enhances well-being, a healthy lifestyle, and social bonds, minimizing the effects of age-related complications and enabling older people to live independently.17,18) The Otago exercise program is based on each person’s tolerance. It has been developed by health professionals and includes empowerment, balance, and aerobic exercise. It was first developed and tested at the University of Otago in New Zealand.19) Several studies have indicated that exercise and individual multifactorial interventions are involved in delaying or reversing frailty and increasing empowerment, quality of life, and well-being.14,20-24) The present study aimed to assess the impact of Otago exercises on frailty and empowerment in older people living in a nursing home. We hypothesizes that older people who participate in the intervention groups will show significant improvements in these outcomes compared to their peers in the control group.
MATERIALS AND METHODS
Study Design and Study Population
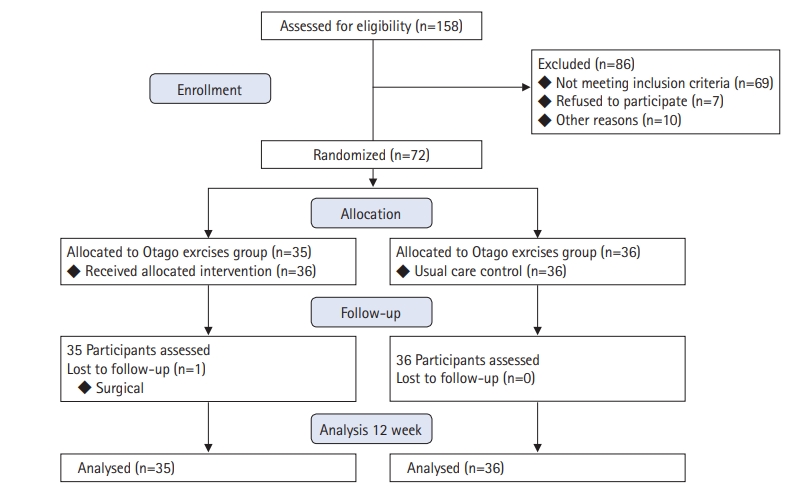
This experimental and randomized controlled trial (Fig. 1) was conducted at Izmir Narlidere Nursing Home from September 2016 to June 2017. The study population consisted of people aged 65 years and older residing in Narlidere Nursing Home. The study participants continued receiving the optimal medical treatment recommended by their physicians throughout the study.
Inclusion criteria were being 65 years of age or older and having the ability to read and write in the Turkish language. Exclusion criteria were needing palliative care; having loss of sight, hearing, and other senses that prevented communication; having a previous diagnosis of dementia, hypotension (systolic blood pressure <90 mmHg, diastolic blood pressure <60 mmHg), anemia (hemoglobin level <9 g/dL), any acute metabolic disorder, uncontrolled hypertension (systolic blood pressure >160 mmHg, diastolic blood pressure >100 mmHg), uncontrolled arrhythmia, stable/unstable angina pectoris, uncontrolled metabolic and chronic disease, and advanced cerebrovascular and peripheral vascular insufficiency; having undergone surgery during the last 6 weeks; and having any physical disability that prevents exercising. Fig. 1 showed a flowchart of the study participants.
The Ethics Committee of Ege University Faculty of Medicine approved this study (No. 70198063-050.06.04). All procedures performed followed the principles of the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The patients were informed of the study protocols in detail and provided their written consent.
Randomization
This study used a convenience and stratified random sampling method. To balance the different individual effects of the exercise program, we classified them according to age and sex. The participants were assigned to each research groups using a simple random method (coin flipping). The groups were as follows: the Otago exercise group (OEG/intervention group) or control group (CG).
The sample size for the present study was calculated to detect a significant clinical difference on the EFS test.25) Using G*Power version 3.1, a test power (1–β error probability) of 0.80, and α=0.05 reliability (type 1 error probability), the research sample size was calculated to be 29 older people for each group to detect a mean difference ≥1 in the EFS (SD=0.5). The sample size was increased by 25% to consider the probability of dropout during follow-up. The final sample size was 72 older people, equally distributed between the two groups (36 participants in each group). However, one participant in the OEG was excluded owing to the need to undergo acute cholecystitis surgery after the start of the study. Hence, this study included 71 older people.
Interventions
Participants in the OEG performed exercises for 45 minutes each on 3 days a week for 12 weeks, plus 30 minutes of walking the other 3 days of the week. The OEG also received 10 30-minute sessions of empowerment-based training. In both OEG and CG, we performed measurements before and after the 3-month intervention and compared them statistically.
Otago Exercise Group
The Otago Exercise Program includes strengthening, balancing, and walking exercises. The Otago exercises were performed in four levels (summarized in Supplementary Table S1). All exercises were performed in 9-member groups under the supervision of a researcher with Otago Exercise Program certification and a nursing home physiotherapist at the Narlidere Nursing Home gym using a practical display method on the pre-programmed days and hours. In all trainings, the characteristics of the older people were considered. We used visual tools (projectors, etc.) to facilitate learning and enhance the knowledge of the older people about training and also provided them a booklet describing the Otago exercises and containing photos of the exercises, some examples of which are included in Supplementary Figs. S1 and S2. Ankle cuff weights, weighing about 0.5 kg, were used in lower extremity resistance exercises under the supervision of a physiotherapist. We also observed the warm-up and cool-down movements before and after exercise. More detail is available from the Otago Medical School University of Otago (https://www.livestronger.org.nz/assets/Uploads/acc1162-otago-exercise-manual.pdf).
The OEG also received 10 30-minute empowerment-based training sessions on topics such as self-care behaviors, problem-solving, decision-making, self-motivation, psychosocial coping, resource utilization, and self-efficacy.
Control Group
The CG received routine health care at Narlidere Nursing Home, including monthly physician visits, tests, prescription medications, and continued daily activities. The CG participants were asked not to participate in any intervention training program during the 3-month study period. To observe the ethical principles in the present study, after completing the research data, knowledge on the concepts of empowerment training and the Otago training program and its applications was also provided to the CG.
Assessments
After providing the necessary information about the study, we obtained written informed consent form from the participants. The participants then completed the research data forms enabling data collection on sociodemographic characteristics, and Edmonton Frail Scale (EFS) and Elderly Empowerment Scale (EES) scores in person. The sociodemographic characteristics form consisted of two parts. The first part included age, sex, educational status, occupation, income level, marital status, number of children, and the place where participants spent much of their time. The second part assessed the participants’ health status, including questions on chronic disease, history of hospitalization, medication use, exercise pattern, sleep pattern, smoking, and alcohol consumption.
We applied the EFS to assess frailty status. The scale was developed by Rolfson et al.26) at the University of Alberta in Canada to describe frailty in older people. The EFS consists of nine dimensions and includes a total of 11 items for the comprehensive assessment of aging as a determinant of frailty. Its dimensions include cognition, general health status, functional independence, social support, medication usage, nutrition, mood, continence, and functional performance. The scores range from 0 to 17. The maximum score, 17, indicates the highest level of frailty. Robust and frail participants were defined based on EFS scores as follows: robust (≤5 points), pre-frail (6–7 points), and frail (≥8 points).26-28) The validity and reliability of the Turkish version of this scale were examined by Aygor et al.,29) with a reported Cronbach’s alpha coefficient of 0.75.
We also used the EES to assess empowerment status. This scale for older people was developed from the Diabetes Empowerment Scale-Short Form (DES-SF) by Anderson et al.30) and was later translated into Turkish.31) The EES includes eight items (one item for each subscale). The eight subscales include satisfaction and dissatisfaction related to old age, identification and achievement of personally meaningful goals, application of a systematic problem-solving process, coping with aspects of living with old age, stress management, appropriate social support, self-motivation, and making cost/benefit decisions about behavior changes. Each item is scored on a 5-point Likert scale, ranging from 5 (strongly agree) to 1 (strongly disagree). The minimum and maximum scale scores are eight and 40 points, respectively, with higher scores indicating stronger empowerment.30-33) The validity and reliability of the scale in Turkish were examined by Jahanpeyma et al.,31) with a reported Cronbach’s alpha of 0.883.
Statistical Analyses
We used IBM SPSS Statistics for Windows (version 22.0; IBM, Armonk, NY, USA) to analyze the data. The categorical variables are expressed as number and percentage, while continuous variables are expressed as mean and SD. Between-group differences were determined using chi-squared and independent t-tests. In statistical evaluations of the variables, we assessed the normality of the variables using Kolmogorov–Smirnov tests. Independent-samples t-test and paired-samples t-test were used in pairwise comparisons and within-group and between-group evaluations because they were consistent with the normal distribution. p<0.05 was considered statistically significant.
RESULTS
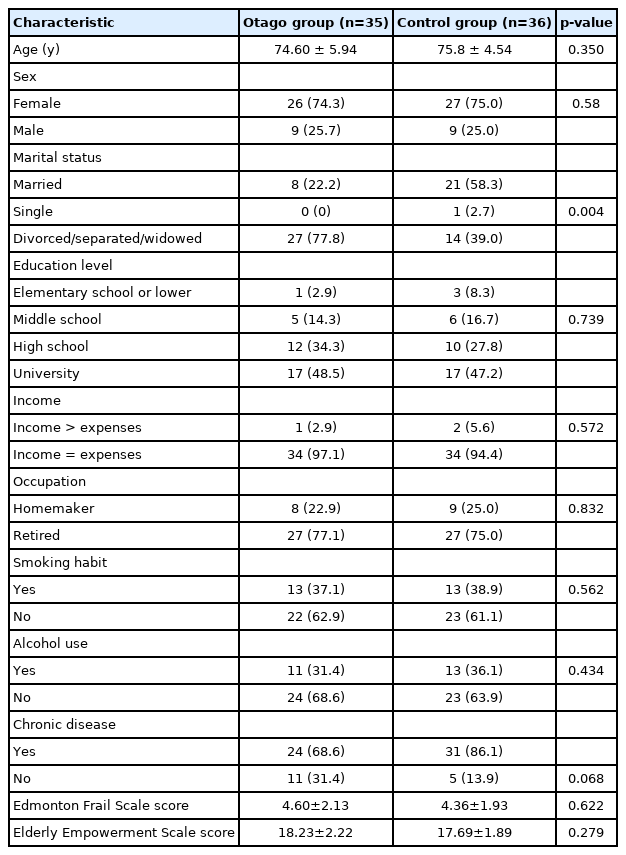
The mean ages of the OEG and CG (74.6±5.9 and 75.8±4.5 years, respectively) were similar, and most participants in both groups were female (74.3% and 75%, respectively). The other demographic characteristics of the two groups were similar, except for marital status (Table 1). We also did not observe significant differences in mean and SD of baseline EES and EFS scores between the OEG and CG (Table 1). We also performed within-group and between-group assessments after calculating the median and mean values for each of the scales before and 3 months after the intervention. The mean EFS before and 3 months after the intervention differed significantly in the OEG (p=0.0001). The mean and SD of EFS before the intervention, 4.60±2.13, decreased to 3.46±1.17 after the intervention, indicating the effectiveness of the Otago exercise program on preventing or delaying frailty. However, we observed no significant changes in the CG (p=0.999). We also observed a significant difference between the two groups in the mean EFS values 3 months after the intervention (p=0.018) (Table 2).
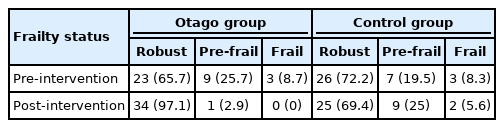
Examination of frailty status in the OEG before the intervention showed that 25.7% of the participants were pre-frail, and this decreased to 2.9% 3 months after the intervention. Eight pre-frail and three partcipants got the robust status 3 months after the intervention, and no participants experienced frailty (Table 3).
In the OEG, the mean EES differed significantly between before and 3 months after the intervention (p=0.0001). The mean and standard deviation of EES before the intervention, 18.23±2.22, increased to 20.77±1.93 after the intervention. However, we observed no significant changes in the CG (p=0.831). The two groups also showed a significant difference in the mean values of EES 3 months after the intervention (p=0.0001) (Table 4).
DISCUSSION
The present study assessed the impact of the Otago Exercise Program on frailty and empowerment in older people aged 65 and over who were residing in nursing homes. Frailty is a biological syndrome in older adults. The factors affecting frailty include a combination of deficiencies in strength, balance, motor processing, cognition, nutrition, endurance, and physical activity.34,35) Our comparisons of the mean EFS scores before and 3 months after the intervention showed a significant difference between the OEG and CG (p=0.0001). Sadjapong et al.9) also reported a significant change (<0.01) in the frailty score of the intervention group compared to the control group. Hsieh et al.21) also observed a significant change (p<0.01) in frailty score in the intervention group than the control group. Finally, Ferreira et al.36) observed that older people in the exercise group showed a 34% reduction in the prevalence of frailty criteria compared to a reduction of approximately 6% in the control group. In our study, most of the older people in the exercise group had a pre-frailty status. We observed an approximately 73% reduction in the number of older people classified as frail in the OEG. In contrast, we observed no significant change between the pre-exercise and post-exercise periods in the CG. Yu et al.37) also observed a significant decrease in frailty score in the intervention group (1.3, p<0.001) but had increased in frailty score in the control group. In general, our results are comparable with those of previous studies. However, contrary to other studies, Takano et al.38) showed that the implementation of 4-month exercise interventions did not significantly affect frailty status.
Empowerment is a multidimensional topic in health and includes the areas of self-care behaviors; self-efficacy; self-control; problem-solving, obtaining support; motivation; psychosocial coping; decision-making; resource utilization; and the relationships of individuals with healthcare providers, healthcare systems, and healthcare services.18) Empowerment affects the participation of people in self-care behaviors, sense of responsibility, taking preventive measures, and decision-making among older adults regarding their health issues to promote health in this population.39,40) We applied the EES to assess the empowerment status of older people in the present study. The mean EES before and 3 months after the intervention differed significantly among the OEG and CG (p=0.001), with higher mean values among participants in the OEG group compared to those in the CG. However, few published studies have assessed the impact of empowerment at the individual or community level. Most studies have been conducted on people with diabetes and different disease groups. Castillo et al.41) reported a significant reduction in glycated hemoglobin (HbA1C) levels and systolic blood pressure after providing empowerment training for people with type 2 diabetes; however, they observed no significant change in body mass index (BMI). Furthermore, Tang et al.42) observed significant reductions in HbA1C and BMI among participants with diabetes in empowerment-based self-management support programs. Yeh et al.43) demonstrated effective results for empowerment and perceived control after 12 weeks of an empowerment training and exercise program in people with heart failure, while Aliakbari et al.44) observed a significant change (p<0.001) in the mean of behavioral ability, self-efficacy, and empowerment score only in the intervention group after providing empowerment training for patients with chronic obstructive pulmonary disease. Karaman et al.45) reported a significant increase in the mean score of the empowerment scale in older people with heart failure who received the intervention. Finally, in their systematic review of 13 studies, Kuijpers et al.14) reported that four studies did not show significant changes in the empowerment of the intervention group.
The limitations of the present study include the short follow-up period, small sample size, and single study area. Thus, the evaluation of the long-term effects with larger sample sizes and in different geographical areas is recommended. Another limitation was that we did not examine the relationship between demographic variables and frailty. Moreover, most of the participants were women; thus, the results may not fully reflect the older population.
In conclusion, the Otago Exercise Program showed positive effects on preventing or delaying frailty and enhancing empowerment in older adults; thus, it may be an effective intervention for preventing and reducing frailty in old-aged nursing home residents.
The study results showed that the implementation of the Otago Exercise Program may be effective in improving physical function and increasing independence in older adults, reducing hospitalization, and reducing costs imposed on the medical system. Therefore, the Otago Exercise Program is recommended as an effective intervention to prevent/delay frailty and increase empowerment in older adults living in nursing homes.
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via https://doi.org/10.4235/agmr.21.0095.
Characteristics of the Otago Exercise Program
Illustration of the Otago exercise: strength exercise.
Illustration of the Otago exercise: balance exercise.
Notes
CONFLICT OF INTEREST
The researchers claim no conflicts of interest.
FUNDING
None.
AUTHOR CONTRIBUTION
Conceptualization: SS, FŞA, YY, PJ; Data curation and Formal analysis: SS, PJ; Investigation and Methodology: SS, FŞA, YY, PJ; Project administration: SS, PJ; Supervision: SS, FŞA, YY; Writing-original draft: SS, FŞA, YY, PJ; Writing-review and editing: FŞA, YY, PJ.