A Case of Ralstonia pickettii Bloodstream Infection and the Growing Problem of Healthcare Associated Infections in Frail Older Adults
Article information
Abstract
Frailty is a clinically measurable state of vulnerability to developing increased dependency and/or mortality when exposed to a stressor. Chronic diseases, aggressive treatments, antibiotic overuse, microbiota changes, immune senescence, and increased use of medical devices and implants (i.e., central lines and catheters) expose modern patients to healthcare-associated infections (HAIs), multidrug-resistant bacteria, and new and unusual opportunistic pathogens. Older adults are among the main victims of HAIs and are associated with high costs, disability, morbidity, and mortality. Ralstonia pickettii is an emerging opportunistic pathogen that causes rare nosocomial infections in frail individuals. Herein, we present a case of bloodstream infection caused by R. pickettii in an 88-year-old woman with a relatively mild course. In addition to describing this unusual finding, this report discusses the problem of HAIs in older adults. Older age, comorbidities, and hospital admissions were among the main risk factors for HAIs. Adherence to guidelines, training, auditing, and surveillance is crucial for reducing the burden of HAIs in acute settings. Furthermore, avoiding incongruous hospitalizations would have positive implications both for preventing HAIs and improving patient quality of life.
INTRODUCTION
Frailty is defined as a clinically measurable state of vulnerability to developing increased dependency and/or mortality when exposed to a stressor.1) As shown by the coronavirus disease 2019 (COVID-19) pandemic, measuring frailty represents a key concept for evaluating therapeutic options, outcomes, and risks.2-4) Longevity does not necessarily come with “healthy aging” and “healthy frailty,”5) and the presence of several determinants like chronic diseases, exposure to aggressive treatments, overuse of antibiotics, changes in microbiota, immune senescence, and the growing use of medical devices and implants (i.e., central lines and catheters) expose modern patients to healthcare-associated infections (HAIs), multidrug-resistant bacteria, and new and unusual pathogens that usually have low virulence in healthy individuals. Older adults are among the main victims of HAIs and are associated with high costs, disability, morbidity, and mortality.6,7) Ralstonia pickettii is a Gram-negative bacillus identified as an emerging opportunistic pathogen responsible for rare nosocomial infections in immunocompromised and multimorbid individuals.8)
Herein, we present a case of bloodstream infection caused by R. pickettii in an 88-year-old woman. In addition to describing this unusual finding, this report also discusses the challenge of HAIs in older adults.
CASE REPORT
An 88-year-old woman was admitted to our Geriatric Medicine ward because of involuntary movements of her left leg and walking difficulties. She was completely dependent in her activities of daily living (ADL) and had a history of Alzheimer disease with severe cognitive impairment, severe behavioral and psychological symptoms, dyslipidemia, chronic anemia, osteoporosis, previous hemorrhagic and ischemic strokes, tight carotid artery stenosis (95%), and unspecified arrhythmic heart disease.
In the emergency room (ER), she was alert but not self-oriented in space and time upon her arrival. Her vital parameters were within normal ranges and she was not feverish. Physical examination revealed three pressure ulcers in the sacral area (third stage) and both heels (third stage, with eschar), for which a urinary catheter was placed. Wound treatment was initiated, as indicated by the Advanced Wound Treatment Team. Her C-reactive protein level was moderately high (20.7 mg/dL), and her leukocyte levels were within normal limits (5.23×109/L). Cerebral computed tomography (CT) was negative for acute ischemic or hemorrhagic events. The following day, she was transferred to our hospital.
She did not exhibit any involuntary movements of her left leg upon arrival or during the following days. Her drug history was negative for possible risk factors, and the electroencephalogram was negative for epileptic activity.
Four days after admission, she presented with a fever (38.2°C) and decreased consciousness. Blood and urinary cultures were negative. After 2 days, she presented again with a fever (38.5°C); this time, blood cultures tested positive for R. pickettii, which was sensitive to piperacillin-tazobactam and resistant to amikacin, cefotaxime, ceftazidime-avibactam, ceftolozane-tazobactam, gentamicin, and tobramycin. She showed increased blood inflammation marker levels (leukocytes, 30.63×109/L, of which 91.8% were neutrophils; C-reactive protein, 131.6 mg/L), worsening renal function during the septic state (estimated glomerular filtration rate [eGFR] from 64 to 16 mL/min/1.73 m2). Owing to venous unavailability, a mini-midline peripheral insertion central catheter was placed after 4 days to ensure the administration of antibiotic therapy. A nasogastric feeding tube was inserted because of reduced consciousness. Both devices were removed after improvement in her clinical conditions, including her state of consciousness.
Piperacillin-tazobactam was prescribed and blood cultures performed 72 hours after the start of antibiotic therapy tested negative. Antibiotics were administered for a total of 14 days, with a decrease in blood inflammation marker levels, improved renal function, and overall clinical conditions (C-reactive protein, 11.6 mg/mL; leukocytes 8.01×109/L; eGFR, 52 mL/min/1.73 m2). The patient was discharged.
Written informed consent was obtained from the patient.
DISCUSSION
R. pickettii is a Gram-negative bacillus identified as an emerging opportunistic pathogen responsible for rare nosocomial infections in immunocompromised and multimorbid individuals. R. pickettii has been associated with several bacteremia outbreaks due to contamination of water and medical solutions, and also with infections of prostheses and medical devices such as central lines.9) Both mild and severe cases of bloodstream infections, pneumonia, meningitis, urinary tract infections, wound infections, endocarditis, septic arthritis, osteomyelitis, and endophthalmitis caused by R. pickettii have been reported.10,11) Disruption of oral microbiota and contamination from R. pickettii has been associated with increased mortality in patients who underwent hematopoietic stem cell transplantation.12)
In the present case, the source of infection was unclear. The patient had peripheral venous access and a urinary catheter, but the first blood and urine culture samples were negative. Although neither swab culture nor tissue biopsies were performed in this specific case, wound infections due to R. pickettii have been reported.13) Therefore, one possible source of infection and bacteremia was the contamination of the sacral pressure ulcers, despite regular treatment.
Frailty is a condition that determines the major state of vulnerability to stressors. The relevant determinants of frailty in this patient were advanced age, severe cognitive deterioration, complete dependence on personal care, and comorbidities. Increasing evidence identifies frailty as a multi-system dysregulation that depends on physical, psychological, and social health and is characterized by deep changes in the biological phenotype. More specifically, frailty is associated with an increased pro-inflammatory state and an alteration of the immune system, referred to as inflammaging and immune senescence, which ultimately lead to reduced efficiency of the immune system (immunodepression).14,15) In our case, increased exposure to potential pathogens due to hospitalization and pressure ulcers and reduced efficiency of the immune system favored the development of an opportunistic HAI.
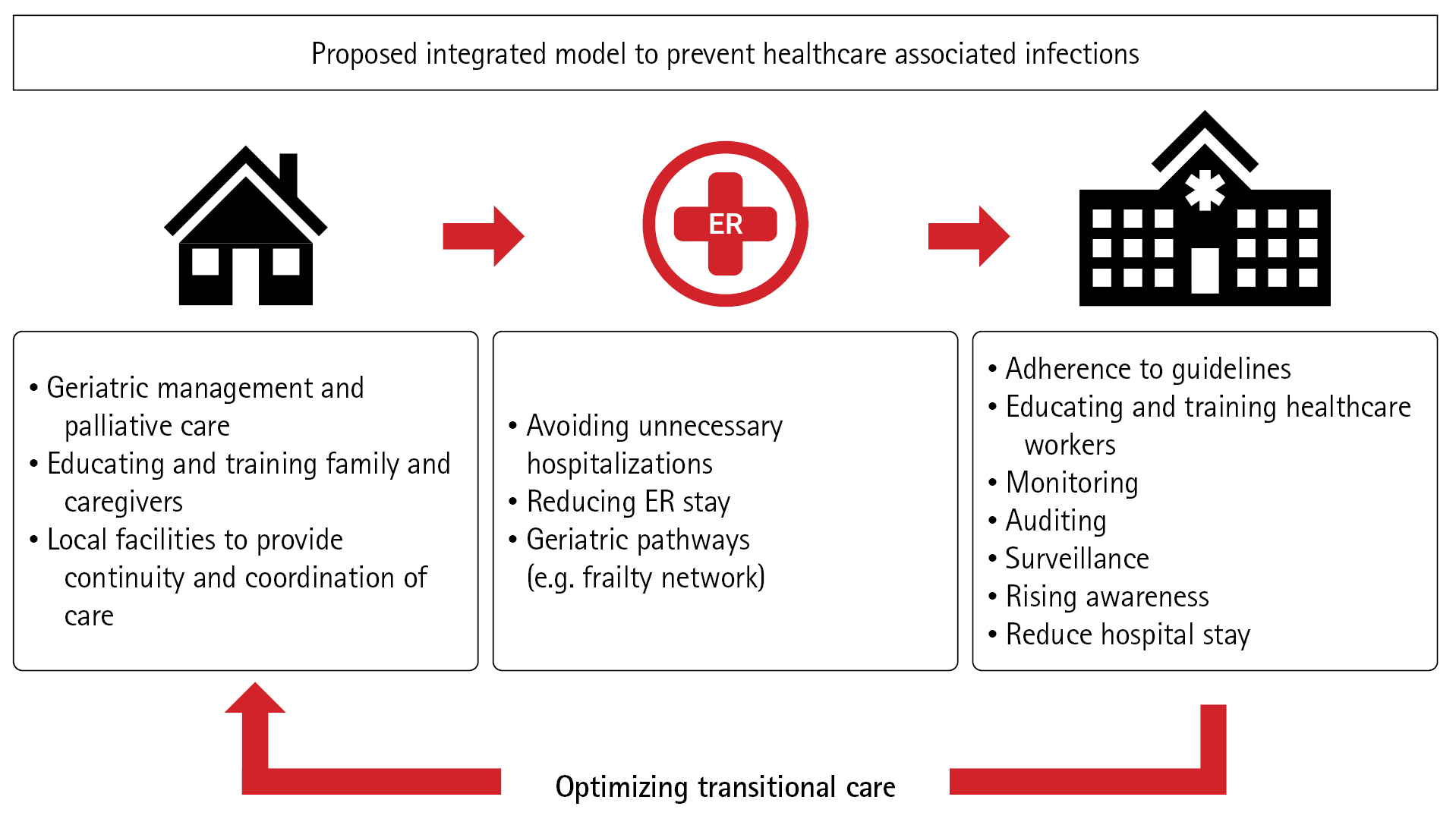
Frailty and hospital readmission are among the main risk factors for HAIs. The global population is increasing in number.16) In Italy, according to the latest report, 43% of the population aged over 65 years has severe non-communicable diseases, with the percentage increasing to >60% in older adults ≥85 years of age.17) A strict adherence to the guidelines established by the World Health Organization,18) appropriate training, auditing, and surveillance are crucial to protect frail patients from HAIs, as well as conducting campaigns to raise awareness among healthcare workers, patients, and visitors. In recent years, our hospital, the Fondazione Policlinico Universitario Agostino Gemelli IRCCS, has made great efforts and conducted several campaigns to fight HAIs.19) Nevertheless, much work remains to be done, and no one can let their guard down, as overlooking the risk of infection in hospitalized patients means exposing them to a potentially fatal threat. In this scenario, the need for more sustainable healthcare and the pivotal role of geriatricians is increasing.20) In hospitals, a more adequate model should involve a shorter length of stay in ERs and acute wards, creating senior-friendly hospitals with dedicated paths. One possible model is represented by the geriatric frailty network currently implemented in our hospital, which aims to assist emergency rooms and ward doctors in preventing the most common geriatric syndromes and reducing the number of incongruous hospitalizations. The characteristics of the proposed model have been discussed elsewhere.21) Attention should be paid to optimizing transitional care and ensuring better communication between hospitals and families, caregivers, and local facilities. The ultimate goal should be not only to optimize diagnostic and therapeutic procedures but also to avoid unnecessary ER readmissions by effectively managing frail and complex patients outside the hospital (Fig. 1).22,23)
In conclusion, we report a case of R. pickettii bloodstream infection in an 88-year-old woman with a relatively mild course. R. pickettii is one of several emerging healthcare-associated pathogens that affect frail older adult patients. Older age, comorbidities, and hospital admissions are among the main risk factors for HAIs. Adherence to guidelines, training, auditing, and surveillance is crucial for reducing the burden of HAIs. Furthermore, avoiding incongruous hospitalizations has positive implications both for preventing HAIs and improving patient quality of life. The possible strategies involve improving the transition-of-care processes, providing attentive follow-up to identify and treat possible causes of hospitalization, and ensuring both the patients’ and caregivers’ compliance with discharge instructions. The true core of geriatric medicine should be primary care.
Notes
CONFLICT OF INTEREST
The researchers claim no conflicts of interest.
FUNDING
None.
AUTHOR CONTRIBUTIONS
Conceptualization, FF, SC, EM, RB, FL; Data curation, RB, FL; Investigation, FF, SC, RM, GS, ST, CA, MA, FM, ET, MM; Supervision, EM, RB, FL; Writing-original draft, FF, SC; Writing-review & editing, SC, MM, EM, ET, RB, FL.