|
 |
- Search
| Ann Geriatr Med Res > Volume 28(1); 2024 > Article |
|
Abstract
The sit-to-stand test is an essential tool used to assess lower limb function and muscle strength in older adults and various patient populations, and also plays a role in sarcopenia screening. Among its forms, the five-time sit-to-stand test (FTSST) is widely used, with previous studies suggesting cutoff values of >10 seconds and >11 seconds for the sitting-to-standing and standing-to-sitting transitions, respectively. The 30-second and 1-minute sit-to-stand tests (30STS and 1MSTS, respectively) also provide comprehensive assessments. While much of the current research on sarcopenia focuses on the FTSST, there is a burgeoning need for an in-depth exploration of the 30STS and 1MSTS. Studies on these tests are vital to refine the criteria for sarcopenia, establish accurate cutoff values, and enhance diagnostic precision and treatment effectiveness. This need highlights the importance of further research into the 30STS and 1MSTS for refining the diagnostic criteria for sarcopenia.
Muscle mass and strength are crucial for maintaining physical health in older adults. Decreased body muscle mass is referred to as sarcopenia.1) Sarcopenia is associated with not only a decrease in muscle strength but also a reduction in balance, leading to an increased risk of falls.1,2) Fractures resulting from falls can severely limit mobility in older adults and patients.2) Mobility is crucial for performing daily activities and significantly impacts overall quality of life.3) Additionally, a decline in mobility leads to a decrease in the quality of life of older adults and their patients.4,5)
Therefore, proactively identifying and preventing sarcopenia in older adults is crucial. The common methods for screening sarcopenia include surveys, calf circumference measurements, hand grip strength tests, and the sit-to-stand test (STST).6) Among these methods, handgrip strength and the STST are used to assess muscle strength. Measuring hand grip strength can be challenging without equipment. However, the STST is a more convenient test that can be easily administered anywhere and requires only a chair, making it highly practical. Additionally, the STST not only assesses lower limb muscle strength but is also a comprehensive tool for evaluating balance and exercise capacity. This test measures the transition from a seated to a standing position and serves as an indicator of basic functional ability in daily activities, akin to a precursor to walking. Therefore, it is a highly versatile testing method, not only for older adults but also for individuals with a variety of diseases.
The five-time sit-to-stand test (FTSST) is commonly used to screen for sarcopenia. Furthermore, in addition to the FTSST, various other STSTs can be used to assess lower limb function and muscle strength. These STSTs enable a more accurate evaluation of lower-limb function and muscle strength tailored to specific situations.7) Therefore, this study introduces commonly used STST methods and proposes recommendations for selecting an appropriate STST based on specific situations.
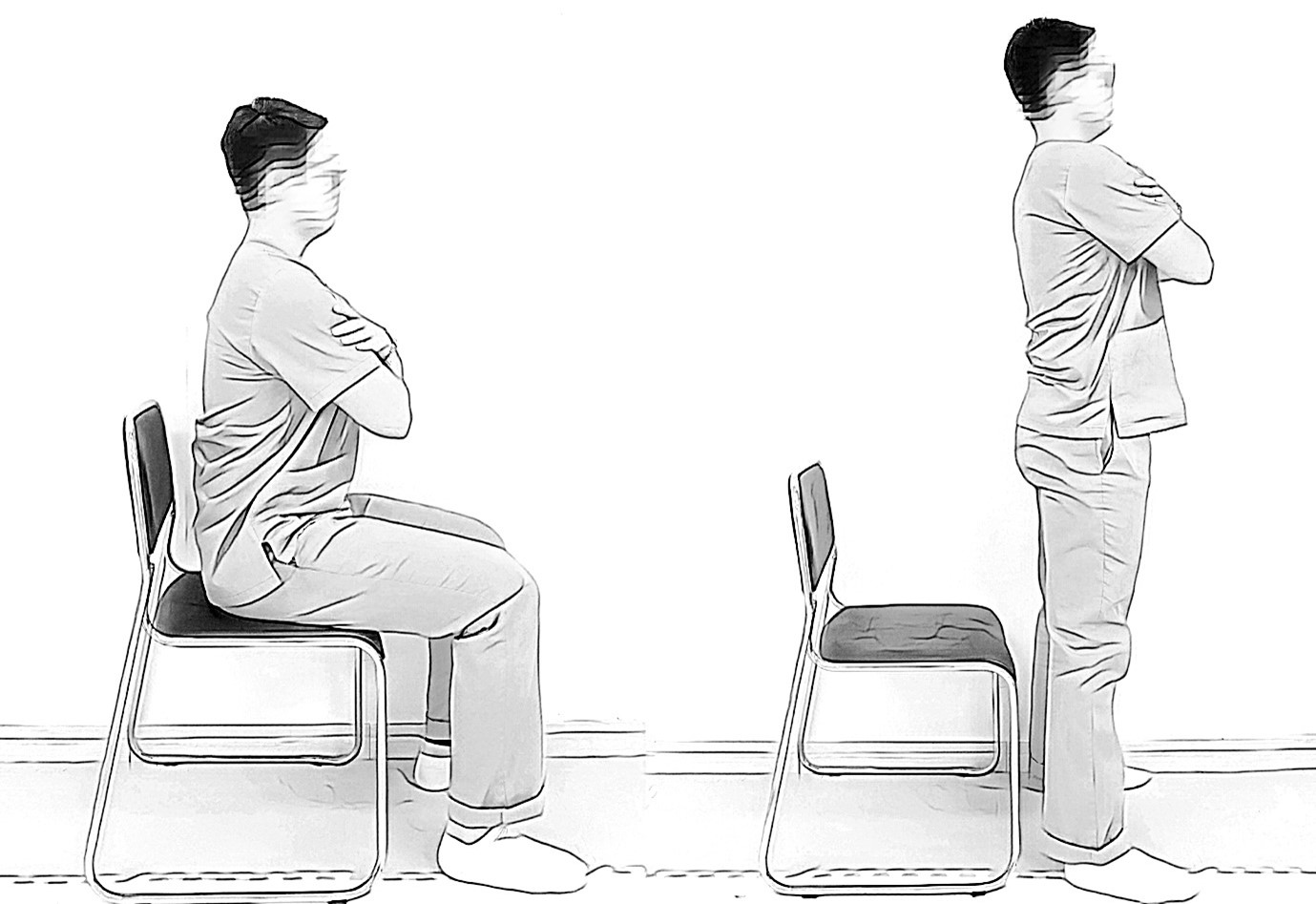
The FTSST is a commonly used version of the STST and is one of the assessments included within the Short Physical Performance Battery (SPPB).8) The FTSST is widely used because it allows easy and rapid measurements using a chair. Moreover, this test is a criterion for assessing sarcopenia in both the Asian Working Group for Sarcopenia (AWGS) 2019 and the European Working Group on Sarcopenia in Older People 2 (EWGSOP-2).9,10) The FTSST involves rapid standing up and sitting down five times consecutively. In this test, the participants start with their arms crossed over their chest, sitting on a chair without armrests, with their hip and knee joints at 90° (Fig. 1). The participants begin the evaluation once they receive the instructions "ready" and "start." The time required to sit or stand five times is recorded.8,11) The measurement is performed twice with a 1â2 minute rest interval, with the fastest time used for assessment.12,13) The results of the FTSST test by age reported in previous studies are presented in Table 1.14-17)
The 30-second sit-to-stand test (30STS) is an effective and valid tool used to evaluate lower limb strength in community-dwelling older adults and offers a wider assessment of ability levels compared with the FTSST.18) Furthermore, the 30STS provides a strong ability to discriminate, particularly in expected differences across age categories and physical activity levels.18) The 30STS is performed in the same posture as the FTSST. However, it is not a test that involves repeating the sitting and standing motions five times; instead, it records the number of times an individual can sit and stand within 30 seconds.13,19) The test is repeated twice after the initial attempt, with a rest interval of 1â2 minutes between measurements.13) The 30STS has been incorporated into functional and balance assessment programs for older adults, such as the Stopping Elderly Accidents, Deaths, and Injuries algorithm developed by the Center for Disease Control and Prevention and the Otago program.20-22) A previous study including 20 healthy Korean men in their 20s reported an average of 32.37Âą4.49 repetitions in the 30STS.23) In a study involving 661 individuals aged 62.6â83.2 years in the Japanese community, the average number of repetitions was 17.26 (95% confidence interval [CI], 15.98â18.55.24) The reported results of the 30STS by age are presented in Table 2.23-27)
One-minute sit-to-stand test (1MSTS) is conducted in the same manner as the 30STS, but the test time is extended from 30 seconds to 1 minute. The test posture is the same as that for the FTSST and 30STS. The 1MSTS records the number of times an individual can sit and stand within 1 minute7) and provides auditory notifications when 30 seconds and 15 seconds remain during the test.28) The test is repeated twice, with a 10-minute rest interval after each test to allow the heart rate and oxygen saturation to return to baseline values before proceeding again.29) The 1MSTS correlates with the 6-minute walking test (6MWT).30) A previous study including 20 healthy Korean men reported an average of 62.75Âą11.09 repetitions in the 1MSTS.23) In a study involving 30 community-dwelling older women aged âĽ65 years in Korea, the average number of repetitions was 40.87Âą8.76.31) The reported results of the 1MSTS by age are presented in Table 3.23,31,32)
Several factors can influence the measurement results when conducting STST. First, the height of the chair used in STST varies across studies, ranging from 40 cm to 48 cm.7,29,30,33-36) Chair height is crucial because it influences the biomechanical movements while standing up from a chair.37) When the chair height is too high, standing is relatively easy, even with an insufficient range of forward trunk flexion.38) Shifting body weight forward while standing allows for a more comfortable range of movement in the trunk, knees, and ankle joints, thus facilitating the overall biomechanical process.39) Therefore, standing can occur quickly with minimal muscular effort.37,39) Given the importance of chair height, ensuring 90° flexion in both the knee and hip joints contributes to objectivity in these measurements and standardizes the test conditions regardless of the chair height.29)
Second, when conducting the examination, the posture standards for both sitting in a chair and standing upright must be communicated and guidance on hand positioning must be provided. One repetition of sitting and standing is defined as the state in which the lower limbs are fully extended after rising from the chair, with clear contact between the chair and hips when sitting.35) Additionally, the participants' hands should be well controlled to prevent the use of hands or arms to assist with movement.35) The use of the hands may involve grasping the knees or chair to assist in standing.
The third consideration is the endpoint criterion. In STST, the final endpoint criterion is defined by two aspects: when seated and when in the fully standing position. The endpoint criterion for the fully standing position is based on the SPPB protocol, whereas that for the seated position is a modified version of the SPPB protocol.11) Specifically, this aspect of the FTSST is crucial because the resulting value is measured within a short duration. The recorded results differ based on the duration taken to complete the test, with variations between the sitting and standing endpoints. A previous study applied a regression equation to 9,383 individuals who underwent the FTSST and were screened for sarcopenia based on the gait speed criterion of <1.0 m/s established by the AWGS 2019. The results indicated that using the standing endpoint resulted in a screening criterion of 11.1 seconds, whereas using sitting as the endpoint yielded a criterion of 11.7 seconds.40)
Finally, the use of digital equipment must be considered. When performing the STST, the state of standing from a seated position is monitored using a load cell and a light detection and ranging (LiDAR) sensor on the chair, allowing for the verification of the total number of stand-up and sit-down cycles.41,42) Although the seated position can be easily measured using the load cell, accurately determining the upright standing posture using both the load cell and LiDAR sensor may pose some challenges. In contrast, if the measurements rely solely on an observer rather than digital equipment, immediate verification of the standing posture is possible; however, accurately confirming the seated posture can be challenging. Therefore, the comprehensive utilization of both approaches allows the most accurate execution of STST. In addition, improving the limitations of digital equipment may lead to more effective measurement methods.
Among STST methods for sarcopenia screening, the FTSST is widely used. The EWGSOP-2 defines >15 seconds as the cutoff value for sarcopenia screening using the FTSST,10) while the AWGS 2019 defines a cutoff of âĽ12 seconds.9)
This difference in criteria can be attributed to various factors such as regional variations, population characteristics, and cultural differences. However, an important factor is the difference in gait speed. The EWGSOP-2 and AWGS 2019 set the gait speed criterion for sarcopenia at â¤0.8 m/s and <1.0 m/s, respectively. A previous study reported a negative correlation between chair stand time and gait speed and proposed a cutoff formula for FTSST of -8.41Ăgait speed+20.0 (R2=0.34) for sarcopenia screening.43) The formulas presented in previous studies confirmed that the cutoff values of the FTSST vary slightly depending on the gait speed standard.
A Korean study on sarcopenia screening criteria suggested FTSST cutoff values of >11 seconds and >10 seconds for finishing in a seated or standing position, respectively.6) These criteria, based on previous studies,6,9) differ from the established standards of the EWGSOP-2 and AWGS 2019. Specifically, they presented criteria based on an endpoint, which was a distinctive feature (Table 4).
In addition to the FTSST, the 30STS has also been proposed as a criterion for sarcopenia screening. The Korean Working Group on Sarcopenia Guidelines provide criteria for the 30STS, suggesting cutoff values of â¤17 and â¤15 repetitions for men and women, respectively.6) These cutoffs were based on the results of a Japanese study targeting older adults.27) Analysis of the receiver operating characteristic curves revealed a threshold of â¤17 repetitions for men in the 30STS, which showed an area under the curve (AUC) of 0.80, a sensitivity of 75.0%, and a specificity of 71.7%. For women, the cutoff was â¤15 repetitions, which showed an AUC of 0.84, a sensitivity of 76.4%, and a specificity of 76.8%.
However, few studies have evaluated the 30STS and 1MSTS and the criteria for sarcopenia. This may be attributed to the limited use of the 30STS and 1MSTS, as the FTSST allows for rapid sarcopenia assessment. Despite these considerations, the 30STS and 1MSTS continue to be widely used for assessing balance in older adults and exercise capacity in individuals with respiratory conditions.34,44,45) Their superior ability to reflect leg strength compared with the FTSST allows these tests to be applied more broadly beyond sarcopenia, serving a diverse range of patients.18,23,46) This highlights the need for further research to develop more targeted sarcopenia-specific criteria for both the 30STS and 1MSTS to enhance their effectiveness and accuracy in sarcopenia screening.
The STST is a comprehensive test that assesses overall muscle strength, dynamic balance, and cardiovascular endurance.47-50) The STST not only assesses the transition from a seated to a standing position but also represents the most fundamental daily activity as the precursor to walking. Successful sitting-to-standing movements require good biomechanical strength in the knee extensor muscles.51) The STST is a test method strongly associated with lower limb strength. The 30STS shows a high correlation with leg press (r=0.71â0.78),18) and through hierarchical linear regression analysis, isokinetic knee extensor concentric contraction at 180° (adjusted R2=0.425, p=0.004) and eccentric contraction (adjusted R2=0.427, p=0.004) were identified as significant independent predictor variables in 30STS.52) STST is significantly correlated (r=-0.49â-0.36) with the thickness of the quadriceps muscle.53)
In a study measuring physical activity levels, individuals with typical activity levels had FTSST times of 5.93Âą1.29 seconds, 22.11Âą3.12 30STS repetitions, and 41.72Âą7.26 1MSTS repetitions.54) However, individuals with high-intensity activity levels showed significantly higher results than those with typical activity levels, with FTSST times of 5.13Âą1.10 seconds, 26.00Âą4.93 30STS repetitions, and 50.54Âą10.26 1MSTS repetitions.54) Another study investigating the correlation between 6MWT distance and 30STS and 1MSTS repetitions in 20 healthy adult men and 20 women in their 20s reported a 6MWT distance of 667Âą55.9 m, 23.6Âą4.35 30STS repetitions, and 45.2Âą9.56 1MSTS repetitions. A significant positive correlation was observed between the 6MWT distance and the STST, with r values of 0.61 for 30STS and 0.64 for 1MSTS, suggesting a moderate correlation.46) Additionally, older adults with relatively poor FTSST results may have a higher risk of falling.55) Moreover, previous studies have investigated FTSST cutoff values for individuals with low physical function. The results of a 2-year follow-up revealed that an FTSST duration of 10.8â12.8 seconds could help identify community-based individuals at risk of impaired physical function, which suggests the potential for designing and implementing preventive interventions.56)
A review of the results of previous studies revealed the numerous associations between the STST and physical function. Therefore, conducting STST assessments in older adults and patients and using these results as a basis for confirming and evaluating physical function is feasible. Among STST methods, the FTSST is commonly used because it allows for rapid examination and provides immediate results regarding lower limb function and strength. While the FTSST is fundamentally the most widely used screening criterion for sarcopenia, using it to assess lower limb strength and function across various age groups may be overly simplistic.17) Therefore, the 30STS and 1MSTS, with slightly higher difficulty in assessing lower limb function and muscle strength, are feasible not only for older adults but also for individuals of various ages. Moreover, the correlation of the 6MWT with the 30STS and 1MSTS has been verified more extensively than with the FTSST; therefore, the 30STS and 1MSTS would be better to use rather than the FTSST in situations where it is difficult to conduct the 6MWT.30,46)
The STST is a tool that can be easily and conveniently used anywhere to assess physical function and screen for sarcopenia, not only in the older adult population but also in patients with various diseases. Different STSTs have been used in research, and their value is being increasingly recognized. The appropriate application of the STST as proposed in the present study is as follows: FTSST should be used for rapid sarcopenia screening. The 30STS should be additionally performed after the FTSST to assess muscle strength. Furthermore, either the 30STS or the 1MSTS should be used to assess balance, exercise capacity, and leg strength in community-dwelling older adults, patients with respiratory diseases, or those with other medical conditions. Presently, most sarcopenia criteria research focuses on the FTSST, including the proposed cutoff values. However, there is a growing need for more research on the criteria for sarcopenia involving the 30STS and 1MSTS, along with the establishment of corresponding cutoff values.
Table 1.
Reference values for the standard five-time sit-to-stand test (unit: second)
| Study | Year | Type of participants | FTSST |
|---|---|---|---|
| Park et al.17) | 2023 | Healthy people | 20s: M (30) 5.15Âą1.02, F (30) 5.46Âą0.95 |
| 30s: M (30) 4.80Âą1.26, F (30) 5.57Âą1.26 | |||
| 40s: M (30) 4.89Âą0.96, F (30) 5.93Âą1.43 | |||
| 50s: M (30) 5.46Âą1.09, F (30) 6.18Âą1.19 | |||
| 60s: M (30) 6.25Âą1.31, F (30) 7.72Âą2.46 | |||
| 70s: M (30) 6.69Âą1.75, F (30) 7.65Âą1.83 | |||
| Bohannon et al.14) | 2010 | Community-dwelling people | 20s: M/F (36) 6.5Âą1.2 |
| 30s: M/F (22) 6.1Âą1.4 | |||
| 40s: M/F (15) 7.6Âą1.8 | |||
| 50s: M/F (20) 7.7Âą2.6 | |||
| 60s: M/F (25) 7.8Âą2.4 | |||
| 70s: M/F (24) 9.3Âą2.1 | |||
| Makizako et al.16) | 2022 | Community-dwelling older adults | |
| 65â69 y: M (62) 7.2Âą1.7, F (102) 7.4Âą2.1 | |||
| 70â74 y: M (73) 8.1Âą2.1, F (114) 7.7Âą2.5 | |||
| 75â79 y: M (53) 8.2Âą2.6, F (77) 8.3Âą2.3 | |||
| Gao et al.15) | 2021 | Community-dwelling older adults | 50â54 y: M (911) 9.36Âą2.79, F (1,031) 10.46Âą3.17 |
| 55â59 y: M (1,228) 9.86Âą3.14, F (1,391) 10.91Âą3.33 | |||
| 60â64 y: M (1,092) 10.23Âą3.13, F (1,053) 11.36Âą3.44 | |||
| 65â69 y: M (725) 10.61Âą3.19, F (674) 12.11Âą3.67 | |||
| 70â74 y: M (504) 11.75Âą3.58, F (390) 12.82Âą4.04 | |||
| 75â79 y: M (281) 12.52Âą4.05, F (259) 13.46Âą3.96 |
Table 2.
Reference values for the standard 30-second sit-to-stand test (unit: times)
| Study | Year | Type of participants | 30STS |
|---|---|---|---|
| Park et al.23) | 2023 | Healthy people | 20s: M (20) 32.37Âą4.49 |
| Lein et al.26) | 2022 | Healthy people | 20s: M/F (81) 33.00Âą5.40 |
| Bjerregaard et al.25) | 2021 | Greenland population health | 55â64 y: M (186) 15.1Âą5.2, F (234) 12.7Âą4.4 |
| 65â74 y: M (137) 12.8Âą5.9, F (152) 10.7Âą4.3 | |||
| 75â84 y: M (31) 10.7Âą4.6, F (37) 9.2Âą5.4 | |||
| Sawada et al.27) | 2021 | Community-dwelling older adults | 65â97 y: M (235) 20.1Âą5.6, F (443) 18.5Âą6.4 |
| Nakazono et al.24) | 2014 | Community-dwelling older adults | Mean age 62.6â83.2 y |
| M/F (661) average 17.26 (95% CI, 15.98â18.55) |
Table 3.
Reference values for the standard 1-minute sit-to-stand test (unit: times)
| Study | Year | Type of participants | 1MSTS |
|---|---|---|---|
| Park et al.23) | 2023 | Healthy people | 20s: M (20) 62.75Âą11.09 |
| Ritchie et al.32) | 2005 | Community-dwelling older adults | 55â70 y: M (11) 34.6Âą6.9, F (9) 26.7Âą4.9 |
| Park and Shin31) | 2023 | Community-dwelling older adults | âĽ65 y: F (30) 40.87Âą8.76 |
REFERENCES
1. Kim M, Won CW. Sarcopenia in Korean community-dwelling adults aged 70 years and older: application of screening and diagnostic tools from the Asian Working Group for Sarcopenia 2019 update. J Am Med Dir Assoc 2020;21:752â8.


2. Schaap LA, van Schoor NM, Lips P, Visser M. Associations of sarcopenia definitions, and their components, with the incidence of recurrent falling and fractures: the Longitudinal Aging Study Amsterdam. J Gerontol A Biol Sci Med Sci 2018;73:1199â204.


3. Samson MM, Meeuwsen IB, Crowe A, Dessens JA, Duursma SA, Verhaar HJ. Relationships between physical performance measures, age, height and body weight in healthy adults. Age Ageing 2000;29:235â42.


4. Brandao GS, Brandao GS, Sampaio AA, Damas Andrade L, Fonseca AL, Campos FK, et al. Home physical exercise improves functional mobility and quality of life in the elderly: a CONSORT-prospective, randomised controlled clinical trial. Int J Clin Pract 2021;75:e14347.


5. Karakaya MG, Bilgin SC, Ekici G, Kose N, Otman AS. Functional mobility, depressive symptoms, level of independence, and quality of life of the elderly living at home and in the nursing home. J Am Med Dir Assoc 2009;10:662â6.


6. Baek JY, Jung HW, Kim KM, Kim M, Park CY, Lee KP, et al. Korean Working Group on Sarcopenia Guideline: expert consensus on sarcopenia screening and diagnosis by the Korean Society of Sarcopenia, the Korean Society for Bone and Mineral Research, and the Korean Geriatrics Society. Ann Geriatr Med Res 2023;27:9â21.




7. Furlanetto KC, Correia NS, Mesquita R, Morita AA, do Amaral DP, MontâAlverne DG, et al. Reference values for 7 different protocols of simple functional tests: a multicenter study. Arch Phys Med Rehabil 2022;103:20â8.


8. Guralnik JM, Ferrucci L, Pieper CF, Leveille SG, Markides KS, Ostir GV, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci 2000;55:M221â31.


9. Chen LK, Woo J, Assantachai P, Auyeung TW, Chou MY, Iijima K, et al. Asian Working Group for Sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc 2020;21:300â7.


10. Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyere O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 2019;48:16â31.




11. Yamada M, Lim JY, Assantachai P, Tanaka T, Kim M, Lee SY, et al. Five-repetition sit-to-stand test: end with the fifth stand or sit? Geriatr Gerontol Int 2022;22:362â4.



12. Munoz-Bermejo L, Adsuar JC, Mendoza-Munoz M, Barrios-Fernandez S, Garcia-Gordillo MA, Perez-Gomez J, et al. Test-retest reliability of five times sit to stand test (FTSST) in adults: a systematic review and meta-analysis. Biology (Basel) 2021;10:510.



13. Petersen C, Steffen T, Paly E, Dvorak L, Nelson R. Reliability and minimal detectable change for sit-to-stand tests and the functional gait assessment for individuals with Parkinson disease. J Geriatr Phys Ther 2017;40:223â6.


14. Bohannon RW, Bubela DJ, Magasi SR, Wang YC, Gershon RC. Sit-to-stand test: performance and determinants across the age-span. Isokinet Exerc Sci 2010;18:235â40.



15. Gao SY, Xia Y, Wu QJ, Chang Q, Zhao YH. Reference values for five-repetition chair stand test among middle-aged and elderly community-dwelling Chinese adults. Front Med (Lausanne) 2021;8:659107.



16. Makizako H, Kiyama R, Nakai Y, Kawada M, Tomioka K, Taniguchi Y, et al. Reference values of chair stand test and associations of chair stand performance with cognitive function in older adults. Aging Health Res 2022;2:100090.

17. Park TS, Tak YJ, Ra Y, Kim J, Han SH, Kim SH, et al. Reference respiratory muscle strength values and a prediction equation using physical functions for pulmonary rehabilitation in Korea. J Korean Med Sci 2023;38:e325.




18. Jones CJ, Rikli RE, Beam WC. A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Res Q Exerc Sport 1999;70:113â9.


19. Diaz-Balboa E, Gonzalez-Salvado V, Rodriguez-Romero B, Martinez-Monzonis A, Pedreira-Perez M, Cuesta-Vargas AI, et al. Thirty-second sit-to-stand test as an alternative for estimating peak oxygen uptake and 6-min walking distance in women with breast cancer: a cross-sectional study. Support Care Cancer 2022;30:8251â60.




20. Shubert TE, Goto LS, Smith ML, Jiang L, Rudman H, Ory MG. The Otago exercise program: innovative delivery models to maximize sustained outcomes for high risk, homebound older adults. Front Public Health 2017;5:54.



21. Stevens JA. The STEADI tool kit: a fall prevention resource for health care providers. IHS Prim Care Provid 2013;39:162â6.


22. Stevens JA, Phelan EA. Development of STEADI: a fall prevention resource for health care providers. Health Promot Pract 2013;14:706â14.

23. Park TS, Lee SJ, Shin MJ, Kang JH. Types of sit-to-stand tests and research on the correlation with body muscle mass. PNF Mov 2023;21:223â9.

24. Nakazono T, Kamide N, Ando M. The reference values for the chair stand test in healthy Japanese older people: determination by meta-analysis. J Phys Ther Sci 2014;26:1729â31.



25. Bjerregaard P, Ottendahl CB, Jorgensen ME. Hand grip strength and chair stand test amongst Greenlandic Inuit: reference values and international comparisons. Int J Circumpolar Health 2021;80:1966186.



26. Lein DH Jr, Alotaibi M, Almutairi M, Singh H. Normative reference values and validity for the 30-second chair-stand test in healthy young adults. Int J Sports Phys Ther 2022;17:907â14.


27. Sawada S, Ozaki H, Natsume T, Deng P, Yoshihara T, Nakagata T, et al. The 30-s chair stand test can be a useful tool for screening sarcopenia in elderly Japanese participants. BMC Musculoskelet Disord 2021;22:639.




28. Strassmann A, Steurer-Stey C, Lana KD, Zoller M, Turk AJ, Suter P, et al. Population-based reference values for the 1-min sit-to-stand test. Int J Public Health 2013;58:949â53.



29. Kuhn M, Vollenweider S, Clarenbach CF, Kohlbrenner D. The effects of standardised versus individualised seat height on 1-minute sit-to-stand test performance in healthy individuals: a randomised crossover trial. Eur J Appl Physiol 2023;123:1543â51.




30. Crook S, Busching G, Schultz K, Lehbert N, Jelusic D, Keusch S, et al. A multicentre validation of the 1-min sit-to-stand test in patients with COPD. Eur Respir J 2017;49:1601871.


31. Park TS, Shin MJ. A study on the correlation between respiratory muscle strength, physical strength, and muscle mass in community-dwelling elderly women. J Kor Acad Cardiorespir Phys Ther 2023;11:33â8.

32. Ritchie C, Trost SG, Brown W, Armit C. Reliability and validity of physical fitness field tests for adults aged 55 to 70 years. J Sci Med Sport 2005;8:61â70.


33. Bohannon RW. Sit-to-stand test for measuring performance of lower extremity muscles. Percept Mot Skills 1995;80:163â6.



34. Bohannon RW, Crouch R. 1-Minute sit-to-stand test: systematic review of procedures, performance, and clinimetric properties. J Cardiopulm Rehabil Prev 2019;39:2â8.


35. Kohlbrenner D, Benden C, Radtke T. The 1-minute sit-to-stand test in lung transplant candidates: an alternative to the 6-minute walk test. Respir Care 2020;65:437â43.


36. Newcomer KL, Krug HE, Mahowald ML. Validity and reliability of the timed-stands test for patients with rheumatoid arthritis and other chronic diseases. J Rheumatol 1993;20:21â7.

37. Ng SS, Cheung SY, Lai LS, Liu AS, Ieong SH, Fong SS. Five Times Sit-To-Stand test completion times among older women: influence of seat height and arm position. J Rehabil Med 2015;47:262â6.


38. Carr JH. Balancing the centre of body mass during standing up. Physiother Theory Pract 1992;8:159â64.

39. Schenkman M, Riley PO, Pieper C. Sit to stand from progressively lower seat heights: alterations in angular velocity. Clin Biomech (Bristol, Avon) 1996;11:153â8.


40. Yamada M, Lim JY, Assantachai P, Tanaka T, Kim M, Lee SY, et al. Reply to the comments on âfive-repetition sit-to-stand test: end with the fifth stand or sit?â. Geriatr Gerontol Int 2022;22:539â40.



41. Baek JY, Jang IY, Jung HW, Park SJ, Lee JY, Choi E, et al. Serum irisin level is independent of sarcopenia and related muscle parameters in older adults. Exp Gerontol 2022;162:111744.


42. Jung HW, Roh H, Cho Y, Jeong J, Shin YS, Lim JY, et al. Validation of a multi-sensor-based kiosk for short physical performance battery. J Am Geriatr Soc 2019;67:2605â9.



43. Nishimura T, Arima K, Okabe T, Mizukami S, Tomita Y, Kanagae M, et al. Usefulness of chair stand time as a surrogate of gait speed in diagnosing sarcopenia. Geriatr Gerontol Int 2017;17:659â61.



44. Zhang Q, Li YX, Li XL, Yin Y, Li RL, Qiao X, et al. A comparative study of the five-repetition sit-to-stand test and the 30-second sit-to-stand test to assess exercise tolerance in COPD patients. Int J Chron Obstruct Pulmon Dis 2018;13:2833â9.




45. McDonald O, Perraton L, Osadnik C. Validity and clinical applicability of the 60-second sit-to-stand test in people with acute exacerbations of COPD. Respir Med 2023;107264.


46. Gurses HN, Zeren M, Denizoglu Kulli H, Durgut E. The relationship of sit-to-stand tests with 6-minute walk test in healthy young adults. Medicine (Baltimore) 2018;97:e9489.



47. Yee XS, Ng YS, Allen JC, Latib A, Tay EL, Abu Bakar HM, et al. Performance on sit-to-stand tests in relation to measures of functional fitness and sarcopenia diagnosis in community-dwelling older adults. Eur Rev Aging Phys Act 2021;18:1.




48. Bennell K, Dobson F, Hinman R. Measures of physical performance assessments: Self-Paced Walk Test (SPWT), Stair Climb Test (SCT), Six-Minute Walk Test (6MWT), Chair Stand Test (CST), Timed Up & Go (TUG), Sock Test, Lift and Carry Test (LCT), and Car Task. Arthritis Care Res (Hoboken) 2011;63 Suppl 11:S350â70.


49. Mateos-Angulo A, Galan-Mercant A, Cuesta-Vargas AI. Muscle thickness contribution to sit-to-stand ability in institutionalized older adults. Aging Clin Exp Res 2020;32:1477â83.



50. Alcazar J, Losa-Reyna J, Rodriguez-Lopez C, Alfaro-Acha A, Rodriguez-Manas L, Ara I, et al. The sit-to-stand muscle power test: an easy, inexpensive and portable procedure to assess muscle power in older people. Exp Gerontol 2018;112:38â43.


51. Kim DH, Park SM, Jeon D, Sung DH. Kinetic and kinematic comparison of sit-to-stand movement between healthy young and elderly subjects. J Korean Acad Rehabil Med 2006;30:385â91.
52. Crockett K, Ardell K, Hermanson M, Penner A, Lanovaz J, Farthing J, et al. The relationship of knee-extensor strength and rate of torque development to sit-to-stand performance in older adults. Physiother Can 2013;65:229â35.



53. Yoshiko A, Ogawa M, Shimizu K, Radaelli R, Neske R, Maeda H, et al. Chair sit-to-stand performance is associated with diagnostic features of sarcopenia in older men and women. Arch Gerontol Geriatr 2021;96:104463.


54. GĂźrses HN, Denizoglu Kulli H, Durgut E, Zeren M. Effect of gender and physical activity level on sit-to-stand test performance among young adults. Bezmialem Sci 2020;8:222â6.

55. Yamada T, Demura S. Effectiveness of sit-to-stand tests for evaluating physical functioning and fall risk in community-dwelling elderly. Hum Perform Meas 2015;12:1â7.