 |
 |
- Search
| Ann Geriatr Med Res > Volume 27(4); 2023 > Article |
|
Abstract
Background
Methods
Results
Fig. 1.
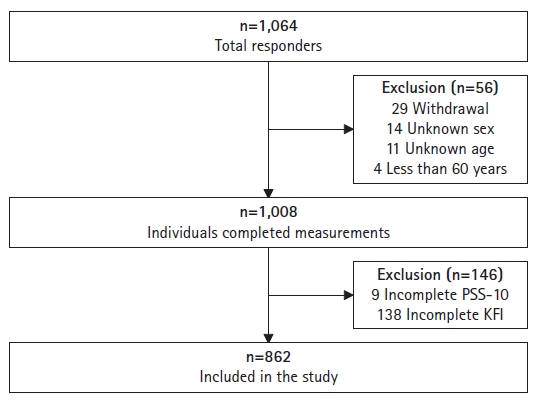
Table 1.
| Total (n=862) | Robust (n=576) | Pre-frail (n=193) | Frail (n=93) | p-value | |
|---|---|---|---|---|---|
| Age (y) | 73.62±5.867 | 72.92±5.835 | 74.58±5.491 | 75.96±5.993 | <0.001 |
| Sex | 0.315 | ||||
| Male | 297 (34.5) | 204 (35.4) | 58 (30.1) | 35 (37.6) | |
| Female | 565 (65.5) | 372 (64.6) | 135 (69.9) | 58 (62.4) | |
| Educationa) | <0.001 | ||||
| Low | 376 (43.6) | 219 (38.0) | 107 (55.4) | 50 (53.8) | |
| High | 474 (55.0) | 350 (60.8) | 82 (42.5) | 42 (45.2) | |
| Missing | 12 (1.4) | 7 (1.2) | 4 (2.1) | 1 (1.0) | |
| Residence | 0.822 | ||||
| Urban | 471 (54.6) | 314 (54.5) | 109 (56.5) | 48 (51.6) | |
| Suburban | 267 (31.0) | 183 (31.8) | 55 (28.5) | 29 (31.2) | |
| Rural | 124 (14.4) | 79 (13.7) | 29 (15.0) | 16 (17.2) | |
| Cohabitation | <0.001 | ||||
| Alone | 349 (40.5) | 186 (32.3) | 107 (55.4) | 56 (60.2) | |
| Not alone | 510 (59.2) | 388 (67.4) | 85 (44.1) | 37 (39.8) | |
| Missing | 3 (0.3) | 2 (0.3) | 1 (0.5) | 0 (0) | |
| Marital status | <0.001 | ||||
| Married | 444 (51.5) | 347 (60.2) | 71 (36.8) | 26 (28.0) | |
| Unmarriedb) | 410 (47.6) | 223 (38.7) | 120 (62.2) | 67 (72.0) | |
| Missing | 8 (0.9) | 6 (1.1) | 2 (1.0) | 0 (0) | |
| Working status | 0.010 | ||||
| Working | 253 (29.4) | 176 (30.6) | 62 (32.2) | 15 (16.1) | |
| Not working | 601 (69.7) | 394 (68.4) | 129 (66.8) | 78 (83.9) | |
| Missing | 8 (0.9) | 6 (1.0) | 2 (1.0) | 0 (0) | |
| PSS-10 | 15.26±3.991 | 14.34±3.529 | 16.04±3.750 | 19.30±4.336 | <0.001 |
| ULS | 38.90±11.282 | 36.29±10.137 | 41.60±10.217 | 49.78±12.483 | <0.001 |
| Missing | 35 (4.1) | 21 (3.6) | 9 (4.7) | 5 (5.4) | |
| CESD | 5.21±4.777 | 3.82±3.606 | 6.9±4.923 | 10.34±6.086 | <0.001 |
| Missing | 18 (2.1) | 10 (1.7) | 7 (3.6) | 1 (1.1) | |
| SWLS | 16.74±4.426 | 17.65±4.080 | 15.55±4.410 | 13.57±4.514 | <0.001 |
| Missing | 7 (0.8) | 4 (0.7) | 2 (1.0) | 1 (1.1) |
Values are presented as mean±standard deviation or number (%).
PSS-10, Perceived Stress Scale-10; ULS, UCLA Loneliness Scale; CESD, Centre for Epidemiological Studies Depression; SWLS, Satisfaction with Life Scale.
Table 2.
Model-1, age and sex adjusted; Model-2, Model-1 + education, residence, cohabitation, marital status and working status adjusted; Model-3, Model-2 + UCLA Loneliness Scale (ULS), Satisfaction with Life Scale (SWLS), and Centre for Epidemiological Studies Depression (CESD) adjusted; CI, confidence interval.
REFERENCES
- TOOLS
-
METRICS

-
- 0 Crossref
- 0 Scopus
- 1,386 View
- 171 Download
-
Related articles in
Ann Geriatr Med Res -
Trajectories, Transitions, and Trends in Frailty among Older Adults: A Review2022 December;26(4)
Delirium in Frail Older Adults2021 September;25(3)
Review of COVID-19 Vaccines and Their Evidence in Older Adults2021 March;25(1)
Air Pollutants and Frailty in Older Adults: A Geriatrician’s Perspective2019 December;23(4)
Diabetes and Muscle Dysfunction in Older Adults2019 December;23(4)






