INTRODUCTION
Since the World Health Organization (WHO) declared the coronavirus disease 2019 (COVID-19) pandemic on March 12, 2020, as of July 3, 2023, a total of 32,131,606 cumulative confirmed cases of COVID-19 in Korea have been recorded by the WHO.
1) COVID-19 is primarily transmitted through respiratory droplets when an infected person coughs, sneezes, talks, or breathes. The symptoms range from mild to severe, with the common symptoms including fever, cough, shortness of breath, fatigue, and loss of taste or smell.
2-4) However, some individuals, particularly older adults, and those with underlying health conditions, may experience severe respiratory distress and other complications.
Previous COVID-19-related research in Korea examined the impact of the comorbidity burden on mortality in patients infected with the virus. However, these studies were limited in scope, relying on data from only 7,590 patients registered until May 15, 2020, and did not specifically focus on older adults.
5) Although studies have been conducted in Wuhan, China, to examine the association between acute respiratory distress syndrome (ARDS), mortality, and risk factors, these studies used data from the overall age range of infected individuals.
6) Another study conducted in South Korea that evaluated the COVID-19 case fatality risk found that, while younger age groups had higher infection rates, older adults had higher mortality rates. However, that study had limitations owing to its relatively small sample size.
7)The COVID-19 pandemic has majorly impacted global health, particularly among older adults who are more vulnerable to severe illness and mortality.
5,6) Understanding the risk factors associated with COVID-19 infection and mortality in this population is crucial for effective prevention and management strategies. South Korea has implemented comprehensive healthcare systems including universal health coverage, providing an ideal setting for investigating these risk factors.
This study aimed to identify key risk factors contributing to COVID-19 infection and mortality among older adults in South Korea. Age, comorbidity burden, disease severity, and insurance type were examined to assess their associations with infection and mortality rates. By utilizing a large-scale nationwide cohort, this study provides robust evidence of specific risk factors affecting this population.
MATERIALS AND METHODS
Data Source
We used the Korea Disease Control and Prevention Agency-COVID-19-National Health Insurance Service (K-COV-N) cohort data from the National Health Insurance Service (NHIS). The data are provided through the universal health coverage for Koreans. Data from the population aged ≥65 years registered between January 1, 2019, and December 31, 2019, were used for analysis. Death was defined as the loss of national health insurance qualification. For COVID-19 confirmation, individuals who claimed with the coronavirus code from January 1, 2020, to March 31, 2022, were included in the analysis. COVID-19 mortality was defined as death within 30 days from the coronavirus code entered for the last time until April 30, 2022.
Using data from the National Health Insurance Corporation's qualification information for 2020, specifically the data related to insured individuals in the 0th percentile of the calculated insurance premium for January 2020, we indirectly reflected the income level by considering the eligibility for NHIS beneficiaries or Medical Aid recipients. In South Korea, the national social security system, known as Medical Aid, provides medical assistance to low-income individuals who lack the means to sustain their livelihoods or who face financial difficulties.
Study Population
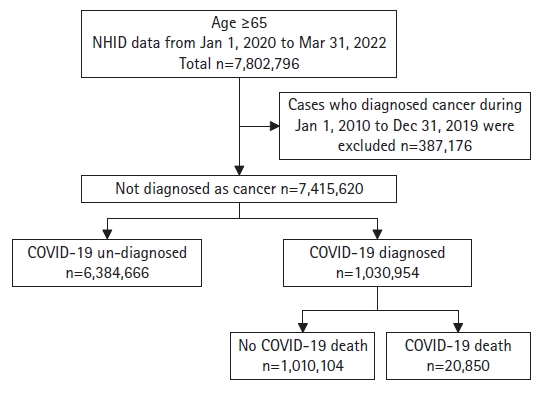
Data from a total of 7,802,796 (n=6,725,628 of non-COVID-19; n=1,077,168 of COVID-19) patients registered between January 1, 2020, and March 31, 2022, were obtained from the NHID database. Based on the qualification data for 2020, those aged ≥65 years were included. Among them, cases where the “C” code (cancer diagnosis),was entered more than once in the primary diagnosis or sub-diagnosis during the 10 years from January 1, 2010, to December 31, 2019, were excluded. Among the group of patients with confirmed COVID-19, only data from those aged ≥65 years were included, and the number of people entered by combining the coronavirus codes from January 1, 2020, to March 31, 2022, was confirmed. Death from COVID-19 was defined as death within 30 days of the last entry of the code U07.1 as a primary or sub-diagnosis, and deaths up to April 30, 22 were included (
Fig. 1).
Data Collection
We utilized data on sex, age, type of insurance, residential area, Charlson Comorbidity Index (CCI), and disease severity. The CCI was calculated based on the diagnosis codes recorded from January 1, 2019, to December 31, 2019. Age groups were categorized as 65–74, 75–84, and ≥85 years. The mean and standard deviation were rounded to the nearest decimal place, while the percentages were rounded to the second decimal place. Insurance eligibility was divided into National Health Insurance and Medical Aid recipients. Residential areas were classified as capital regions, including Seoul, Gyeonggi Province, and Incheon.
Disease severity was classified by assessing whether specific treatment codes were present within the infectious period, enabling us to categorize hospitalization and the condition severity. The treatment levels of "oxygen therapy" and "oxygen by mask or nasal prongs" were defined as "hospitalized mild disease," while "non-invasive ventilation or high-flow oxygen," "intubation and mechanical ventilation," and "ventilation + additional organ support (continuous renal replacement therapy [CRRT], extracorporeal membrane oxygenation [ECMO])" were categorized as "hospitalized severe disease" if implemented. The classification was based on the most severe point of the condition.
Ethical Consideration
This study was approved by the Institutional Review Board of Kyung Hee University Hospital (No. KHUH 2022-11-059). The requirement for informed consent was waived because this study used de-identified administrative data. Also, this study complied the ethical guidelines for authorship and publishing in the
Annals of Geriatric Medicine and Research.
8)
Statistical Analysis
Using frequencies and percentages, we compared the characteristics of COVID-19 patients and individuals without confirmed infection. Additionally, we conducted a multivariate logistic regression analysis to identify the factors associated with the occurrence of and death due to COVID-19. We calculated adjusted odds ratios (ORs) for nine factors: region, sex, age group, CCI, four specific diseases, and MA status. We defined the significance level as two-tailed p-values <0.05.
In the analysis of disease severity, we first compared confirmed cases that were not hospitalized with those that were hospitalized. Second, we compared “hospitalized severe disease” and deceased patients with other patients. Finally, we compared deceased patients with the remaining patients.
RESULTS
Characteristics and Risk Factors for COVID-19 Infection
Among the 7,415,620 participants, 44.33% resided in the capital region. Of the 1,030,954 infected individuals, 49.26% resided in the capital region. A total of 43.53% of non-infected individuals also lived in the capital region. Men comprised 41.87%, and 41.05% of the entire study population and infected individuals, respectively. The 65–74-year age group accounted for 4,263,439 individuals, representing 57.49% of the total population. Among them, 643,625 were affected by COVID-19, corresponding to 62.43% of the 1,030,954 infected individuals. In the 75–84-year age group, 286,940 individuals were affected by COVID-19. The OR for this age group compared with the 65–74-year age group was 0.756 (95% confidence interval [CI], 0.753–0.76), indicating a lower risk of infection. The population aged ≥85 years (790,234 individuals, 10.66%) included 100,389 confirmed cases (9.74%). The OR was 0.789 (95% CI, 0.783–0.795), indicating a lower infection risk than that in the 65–74-year age group. These results suggested that the infection risk of COVID-19 did not necessarily increase with age and that the infection rate was lower in older age groups (
Table 1).
Among the 1,030,954 confirmed cases, 225,710 (21.89%), 255,637(24.8%), and 549,607(53.31%) had CCI scores of 0, 1, and 2, respectively. Compared with the reference group with CCI scores of 0, the ORs were 1.217 (95% CI, 1.209–1.224) for a CCI score of 1 and 1.33 (95% CI, 1.321–1.339) for a CCI score ≥2. Thus, the infection rate increased with higher CCI scores.
Regarding the relationship between income level and susceptibility to infection, when considering medical insurance status, the OR for Medical Aid recipients compared to that for insurance beneficiaries was 0.898 (95% CI, 0.89–0.906). Thus, Medical Aid recipients had a lower risk of infection than insurance beneficiaries.
Characteristics and COVID-19 Mortality
Comparison of the risk of death based on residential area showed that 47.54% of the deceased individuals resided in the capital region. When using individuals residing in the capital region as the reference, the OR for non-capital region residents confirmed to have COVID-19 was 0.928 (95% CI, 0.903–0.955). Among all confirmed and deceased cases, 41.05% and 42.35% were men, respectively. The OR for the risk of death in women compared to men was 0.607 (95% CI, 0.59–0.625), indicating a higher risk of death in men. The average age of the confirmed cases was 73.5 years, while the average age of the deceased after confirmation was 82.4 years. Among all confirmed cases, 61.43% were aged 65–74 years, 27.83% were aged 75–84 years, and 9.74% were aged ≥85 years. Comparison of the risk of progression to death using the group aged 65–74 years as a reference, the OR for the 75–84 years age group was 4.406 (95% CI, 4.236–4.582), while that for the ≥85 years age group was 16.032 (95% CI, 15.399–16.691). Compared to the reference group with a CCI score of 0, the ORs for the risk of death after confirmation among patients with CCI scores of 1 and ≥2 were 1.172 (95% CI, 1.111–1.236) and 1.537 (95% CI, 1.459–1.618), respectively. This indicates that as the burden of comorbidities increased (higher CCI score), the risk of death also increased. Compared to the general population with medical insurance, patients with Medical Aid showed a higher risk of death (OR=1.692; 95% CI, 1.623–1.763) (
Table 2).
Correlation between Age and COVID-19 Severity and Length of Hospitalization
A total of 173,816 of 1,030,954 confirmed cases aged ≥65 years were hospitalized. The analysis was conducted by categorizing individuals into four groups based on the severity of hospitalization: non-hospitalized, hospitalized mild disease, hospitalized severe disease, and death. We evaluated severity based on the most severe condition during the treatment period.
First, using the non-hospitalized group as a reference, we divided the hospitalized patients into age groups and assessed the risk of hospitalization according to the OR. Taking the age group of 65–74 years as the reference, the ORs of hospitalization for the 75–84 and ≥85 years age groups were 2.007 (95% CI, 1.983–2.032) and 4.933 (95% CI, 4.857–5.01), respectively, indicating a higher risk of hospitalization with increasing age.
The group exhibiting severe disease during hospitalization was compared with the group showing lower disease severity. Age-specific risks were also compared. Taking the age group of 65–74 years as the reference, the OR for the 75–84 and ≥85 years age groups were 3.129 (95% CI, 3.032–3.228) and 10.012 (95% CI, 9.685–10.35), respectively. Thus, the risk of progression to severe or higher COVID-19 severity increased with age. Comparison of mortality rates by age group showed an OR for the ≥85-years age group of 16.032 (95% CI, 15.399–16.691), indicating a significantly higher mortality rate as age increased, especially in the ≥85 years age group compared to that in the youngest age group. Finally, we compared the length of hospitalization by age, specifically among patients who were hospitalized for more than a week, with other confirmed cases as the control group. Among all infected individuals, 126,964 (12.32%) required hospitalization for more than 1 week.
Among the 643,625 infected individuals aged 65–74 years, 56,253 (8.74%) required hospitalization for more than one week. In comparison, 15.3% of those aged 75–84 years (OR=1.762; 95% CI, 1.738–1.786) and 26.69% of those aged ≥85 years (OR=3.515; 95% CI, 3.455–3.576) required hospitalization for more than one week. These findings confirmed that as age increases, the duration of hospitalization also tends to increase, indicating a higher need for hospitalization as individuals age.
Table 3 shows the severities and hospitalization dates of COVID-19 patients classified by age, and
Table 4 shows the results of the multivariate analysis.
DISCUSSION
Our study was conducted using a large-scale population-based cohort. The most influential factor in the severity and mortality rate of COVID-19 in older Korean adults was age. Furthermore, being an Medical Aid recipient and having multiple comorbidities increased the risk of COVID-19 infection progressing to mortality.
The risk of infection was lower for individuals with cardiovascular disease (OR=0.974; 95% CI, 0.969–0.978) and diabetes (OR=0.963; 95% CI; 0.958–0.968). In contrast, the risk of infection was higher in individuals with cerebrovascular disease (OR=1.057; 95% CI, 1.051–1.063) and chronic respiratory disease (OR=1.066; 95% CI, 1.061–1.072).
The risk of mortality increased significantly with cerebrovascular disease (OR=1.338; 95% CI, 1.295–1.383) and diabetes (OR=1.142; 95% CI, 1.107–1.178) but not for cardiovascular disease (OR=1.018; 95% CI, 0.984–1.052) and chronic respiratory disease (OR=0.887; 95% CI, 0.857–0.918).
Previous studies compared factors such as sex, medical history, disease severity, and mortality related to COVID-19 infection between older and younger age groups.
9-11) One study found that in all age groups, men had a higher oxygen demand and greater disease severity (p<0.01, p=0.0083).
9) Furthermore, univariate analysis revealed that the risk of non-mild COVID-19 was significantly higher (p<0.05) in middle-aged and older adults than in young adults.
9) Another study using data from a total of 1,537 patients reported that in-hospital mortality was associated with older age after adjusting for age, hypertension, diabetes mellitus, and corticosteroid use (risk ratio [RR]=2.01; 95% CI, 1.59–2.52).
10) These findings are consistent with the main findings of the present study. However, the previous study had limitations in terms of a smaller sample size and shorter observation period (from May 2020 to August 2020) compared to our study.
A previous study conducted using COVID-19-confirmed case data registered in South Korea until May 15, 2020, that evaluated the association between CCI values (3, 4, and 5 or higher) and mortality also found an increasing trend in mortality with increasing age-adjusted CCI score.
11) Although this study included data from a younger age group, a similar trend was observed in the present study.
In this study, patients with diabetes and cerebrovascular diseases had a higher COVID-19-related mortality rate, which is consistent with previously reported findings.
12) However, we observed no significant relationship between cardiovascular disease and COVID-19-related mortality rates. In this study, the cardiovascular disease categories included hypertension, ischemic heart disease, cardiomyopathy, atrial fibrillation, and heart failure. Previous studies have demonstrated that each of these conditions contributes to increased mortality in COVID-19 patients. A review reported that hypertension, which is the most common underlying disease, can increase the severity and mortality rates of COVID-19. However, the use of renin–angiotensin–aldosterone system (RAAS) inhibitors may provide benefits in the course of the disease.
13) Another study found that angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin receptor blockers (ARBs) mitigate COVID-19 mortality rates in patients with hypertension.
14) In the management of hypertension in South Korea, the most commonly used monotherapy is ARB (50.1%). Even in combination therapies (dual therapy), ARB/ACEi regimens dominate, accounting for 89.9% of cases.
15) This contradictory relationship may explain the lack of significance between cardiovascular disease and COVID-19 mortality.
The chronic respiratory disease categories in the present study included obstructive pulmonary disease, chronic bronchitis, emphysema, asthma, persistent asthma, and bronchiectasis. According to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2023 report, chronic obstructive pulmonary disease (COPD) is more likely to worsen with severe COVID-19. However, the impact of COPD on the risk of COVID-19 is unclear, which is consistent with the low risk of infection in our study.
16) In another study investigating the relationship between obstructive pulmonary disease (OPD) and COVID-19, a total of 7,549 patients with a history of COPD were included for comparison of mortality rate. The study found that patients with COPD had higher hospitalization rates (62% vs. 28%) and higher mortality rates (15% vs. 4%; adjusted OR=2.1; 95% CI, 1.96–2.26; p<0.001) compared to those without COPD.
17) Regarding asthma, a cohort study compared the risk of COVID-19-related mortality between adults using low-dose inhaled corticosteroids (ICS) and those without asthma. The study did not observe a significant difference in mortality risk between patients with and without asthma.
18) Another study suggested that one mechanism of asthma, involving type 2 airway inflammation and ACE2/TMPRSS2 receptor downregulation and the use of controllers such as ICS, might underrepresent COVID-19 symptoms.
19)In our study, patients with chronic respiratory disease showed decreased mortality rates (OR=0.887; 95% CI, 0.857–0.918), which could be due to asthma. Second, the prevalence of COPD in South Korea is relatively high, reaching 13.4% in individuals aged ≥40 years. However, in COPD, symptoms may remain mild or go unnoticed until the lung function is compromised by >50%. Moreover, many cases are attributed to aging-related symptoms, leading to underdiagnosis.
20) Lastly, our study has some limitations in the results as we did not consider data on the severity of chronic respiratory disease.
Previous domestic studies examining the association between mortality from COVID-19 and socioeconomic income levels, considering characteristics such as age, sex, and underlying diseases, observed no significant difference in the risk of death between Medical Aid recipients and health insurance beneficiaries.
21) In contrast, in our study, after adjusting for factors such as region, sex, age group, CCI, and major underlying diseases, we observed a higher mortality rate than infection rate in the Medical Aid patient group. This aligns with the findings of another systematic review and meta-analysis of 4.3 million patients from 68 studies which found that socioeconomic determinants were strongly associated with COVID-19 outcomes in racial and ethnic minority populations.
22) The previous domestic study included only 7,590 confirmed cases as of May 15, 2020, which may explain the discordant results.
We identified age as the factor with the greatest impact on the infection rates and subsequent mortality. Therefore, prioritizing the vaccination of older adults may be warranted in future infectious disease situations. Additionally, as age increased, the length of hospitalization tended to increase. Given the gradual aging of society and the increasing elderly population, policies aimed at securing an adequate number of hospital beds are needed. Analysis of the data by insurance type showed a lower infection rate among Medical Aid recipients than among NHIS beneficiaries; however, the mortality rate of Medical Aid recipients was higher. This can be attributed not only to socioeconomic differences, as pointed out in previous studies on COVID-19 infection and mortality rates in the domestic healthcare environment with universal health coverage, but also to other factors that may have had a marked impact, such as poor underlying health conditions, rapid early testing and treatment, transmission-reducing behaviors, and regional preparedness.
23) Considering the relatively high cost of self-testing kits and the surge in demand for masks, which have increased personal hygiene expenses, it is important to implement national policies that provide appropriate support and resources to Medical Aid recipients. This is crucial for preventing economic differences from translating into differences in infection and mortality rates.
Limitations and Strengths
This study has several strengths. First, it benefits from a nationwide cohort in which the entire population is enrolled in health insurance programs. This resulted in a large sample size, which increased the statistical significance of the findings. Additionally, the study focused exclusively on the elderly population aged ≥65 years. By identifying the most significant factors related to disease outcomes in older adults, who are generally considered vulnerable to infections due to the high prevalence of underlying health conditions, our findings can be utilized to prioritize management with limited resources in the event of future infectious diseases.
In addition, a previous study comparing age and COVID-19-related mortality in South Korea identified malignant neoplasms as having the highest hazard ratio among comorbidities.
23) In the present study, we excluded patients diagnosed with cancer within the past 10 years to ensure distinctiveness in our analysis. However, this study had some limitations. First, as the population decreases with increasing age, the infection rate among older adults may have been underestimated in the OR. However, the sufficiently large OR for mortality suggests that the results remain valid for evaluating the severity of COVID-19 and the importance of age in policy decisions. Second, statistical errors may have occurred due to the relatively low proportion of Medical Aid recipients compared with that in the total population. According to the "2021 Medical Aid Statistical Yearbook" jointly published by the National Health Insurance Corporation and Health Insurance Review and Assessment Service in October 2022, the number of Medical Aid recipients was 1,516,525, accounting for approximately 2.9% of the total population (approximately 52.92 million).
24) However, as 39.1% of Medical Aid recipients were aged ≥65 years and this study focused on this age group, our findings are highly significant in evaluating the relationship between COVID-19 and insurance status.
The study's limitation lies in the use of insurance type as a proxy for access to healthcare without accounting for other factors such as living conditions,
25) exposure to smoking, and work environments, which could also contribute to higher infection rates. Reports have suggested an association between smoking and COVID-19 progression and mortality.
26) However, the present study did not include such data, indicating the need for further research in this area. Moreover, the reduction in mortality among individuals surveyed later in the data collection period could be attributed to the commencement of the national COVID-19 vaccination in South Korea.
In this study, the incidence of COVID-19 among Medical Aid beneficiaries was lower than that among NHIS beneficiaries, and the mortality of COVID-19 among Medical Aid beneficiaries was higher than that among NHIS beneficiaries. These findings are in stark contrast to the results of previous studies.
27,28) While other studies have examined the early phase of the COVID-19 pandemic, our study covered a longer period of exceeding 2 years. Therefore, our study better reflects the trend of the COVID-19 pandemic. Because Medical Aid beneficiaries have relatively poor jobs, they may have lost their jobs due to the prolonged COVID-19 pandemic. Due to the COVID-19 pandemic, these individuals could not use community services such as welfare centers and senior citizen centers and likely spent more time at home. This may have reduced human contact, and consequently, reduced the prevalence of COVID-19. However, this is merely speculation, and no precise analysis has been performed. Further studies are needed to confirm this hypothesis. Our results may have been better supported if we had conducted a comparative analysis between COVID-19 infection status and COVID-
19-related deaths. However, this analysis was not possible, which is a limitation of our study.
Lastly, as long COVID syndrome has gained attention, discussion continues regarding its long-term effects. However, this study did not evaluate long-term complications, which is a limitation that warrants further investigation.
Conclusion
The most significant factor for COVID-19 infection was the severity of the underlying health conditions, whereas age and socioeconomic status were the most critical factors for post-infection mortality. The results of this study suggest that in the event of a large-scale respiratory infection, policies should prioritize vaccination and the provision of hospital beds for the elderly, rather than focusing solely on underlying health conditions. For individuals receiving Medical Aid, it is crucial to implement measures such as rapid screening tests and ensure the availability of healthcare supplies to correct the pathways contributing to the worsening of infection.
Overall, the results of this study provide valuable insights for the development of policies and interventions in response to respiratory infections, emphasizing the importance of age, underlying health conditions, and socioeconomic factors in determining infection and mortality rates.
29)