|
 |
- Search
| Ann Geriatr Med Res > Volume 26(4); 2022 > Article |
|
Abstract
Frailty is a clinically measurable state of vulnerability to developing increased dependency and/or mortality when exposed to a stressor. Chronic diseases, aggressive treatments, antibiotic overuse, microbiota changes, immune senescence, and increased use of medical devices and implants (i.e., central lines and catheters) expose modern patients to healthcare-associated infections (HAIs), multidrug-resistant bacteria, and new and unusual opportunistic pathogens. Older adults are among the main victims of HAIs and are associated with high costs, disability, morbidity, and mortality. Ralstonia pickettii is an emerging opportunistic pathogen that causes rare nosocomial infections in frail individuals. Herein, we present a case of bloodstream infection caused by R. pickettii in an 88-year-old woman with a relatively mild course. In addition to describing this unusual finding, this report discusses the problem of HAIs in older adults. Older age, comorbidities, and hospital admissions were among the main risk factors for HAIs. Adherence to guidelines, training, auditing, and surveillance is crucial for reducing the burden of HAIs in acute settings. Furthermore, avoiding incongruous hospitalizations would have positive implications both for preventing HAIs and improving patient quality of life.
Frailty is defined as a clinically measurable state of vulnerability to developing increased dependency and/or mortality when exposed to a stressor.1) As shown by the coronavirus disease 2019 (COVID-19) pandemic, measuring frailty represents a key concept for evaluating therapeutic options, outcomes, and risks.2-4) Longevity does not necessarily come with ŌĆ£healthy agingŌĆØ and ŌĆ£healthy frailty,ŌĆØ5) and the presence of several determinants like chronic diseases, exposure to aggressive treatments, overuse of antibiotics, changes in microbiota, immune senescence, and the growing use of medical devices and implants (i.e., central lines and catheters) expose modern patients to healthcare-associated infections (HAIs), multidrug-resistant bacteria, and new and unusual pathogens that usually have low virulence in healthy individuals. Older adults are among the main victims of HAIs and are associated with high costs, disability, morbidity, and mortality.6,7) Ralstonia pickettii is a Gram-negative bacillus identified as an emerging opportunistic pathogen responsible for rare nosocomial infections in immunocompromised and multimorbid individuals.8)
Herein, we present a case of bloodstream infection caused by R. pickettii in an 88-year-old woman. In addition to describing this unusual finding, this report also discusses the challenge of HAIs in older adults.
An 88-year-old woman was admitted to our Geriatric Medicine ward because of involuntary movements of her left leg and walking difficulties. She was completely dependent in her activities of daily living (ADL) and had a history of Alzheimer disease with severe cognitive impairment, severe behavioral and psychological symptoms, dyslipidemia, chronic anemia, osteoporosis, previous hemorrhagic and ischemic strokes, tight carotid artery stenosis (95%), and unspecified arrhythmic heart disease.
In the emergency room (ER), she was alert but not self-oriented in space and time upon her arrival. Her vital parameters were within normal ranges and she was not feverish. Physical examination revealed three pressure ulcers in the sacral area (third stage) and both heels (third stage, with eschar), for which a urinary catheter was placed. Wound treatment was initiated, as indicated by the Advanced Wound Treatment Team. Her C-reactive protein level was moderately high (20.7 mg/dL), and her leukocyte levels were within normal limits (5.23├Ś109/L). Cerebral computed tomography (CT) was negative for acute ischemic or hemorrhagic events. The following day, she was transferred to our hospital.
She did not exhibit any involuntary movements of her left leg upon arrival or during the following days. Her drug history was negative for possible risk factors, and the electroencephalogram was negative for epileptic activity.
Four days after admission, she presented with a fever (38.2┬░C) and decreased consciousness. Blood and urinary cultures were negative. After 2 days, she presented again with a fever (38.5┬░C); this time, blood cultures tested positive for R. pickettii, which was sensitive to piperacillin-tazobactam and resistant to amikacin, cefotaxime, ceftazidime-avibactam, ceftolozane-tazobactam, gentamicin, and tobramycin. She showed increased blood inflammation marker levels (leukocytes, 30.63├Ś109/L, of which 91.8% were neutrophils; C-reactive protein, 131.6 mg/L), worsening renal function during the septic state (estimated glomerular filtration rate [eGFR] from 64 to 16 mL/min/1.73 m2). Owing to venous unavailability, a mini-midline peripheral insertion central catheter was placed after 4 days to ensure the administration of antibiotic therapy. A nasogastric feeding tube was inserted because of reduced consciousness. Both devices were removed after improvement in her clinical conditions, including her state of consciousness.
Piperacillin-tazobactam was prescribed and blood cultures performed 72 hours after the start of antibiotic therapy tested negative. Antibiotics were administered for a total of 14 days, with a decrease in blood inflammation marker levels, improved renal function, and overall clinical conditions (C-reactive protein, 11.6 mg/mL; leukocytes 8.01├Ś109/L; eGFR, 52 mL/min/1.73 m2). The patient was discharged.
Written informed consent was obtained from the patient.
R. pickettii is a Gram-negative bacillus identified as an emerging opportunistic pathogen responsible for rare nosocomial infections in immunocompromised and multimorbid individuals. R. pickettii has been associated with several bacteremia outbreaks due to contamination of water and medical solutions, and also with infections of prostheses and medical devices such as central lines.9) Both mild and severe cases of bloodstream infections, pneumonia, meningitis, urinary tract infections, wound infections, endocarditis, septic arthritis, osteomyelitis, and endophthalmitis caused by R. pickettii have been reported.10,11) Disruption of oral microbiota and contamination from R. pickettii has been associated with increased mortality in patients who underwent hematopoietic stem cell transplantation.12)
In the present case, the source of infection was unclear. The patient had peripheral venous access and a urinary catheter, but the first blood and urine culture samples were negative. Although neither swab culture nor tissue biopsies were performed in this specific case, wound infections due to R. pickettii have been reported.13) Therefore, one possible source of infection and bacteremia was the contamination of the sacral pressure ulcers, despite regular treatment.
Frailty is a condition that determines the major state of vulnerability to stressors. The relevant determinants of frailty in this patient were advanced age, severe cognitive deterioration, complete dependence on personal care, and comorbidities. Increasing evidence identifies frailty as a multi-system dysregulation that depends on physical, psychological, and social health and is characterized by deep changes in the biological phenotype. More specifically, frailty is associated with an increased pro-inflammatory state and an alteration of the immune system, referred to as inflammaging and immune senescence, which ultimately lead to reduced efficiency of the immune system (immunodepression).14,15) In our case, increased exposure to potential pathogens due to hospitalization and pressure ulcers and reduced efficiency of the immune system favored the development of an opportunistic HAI.
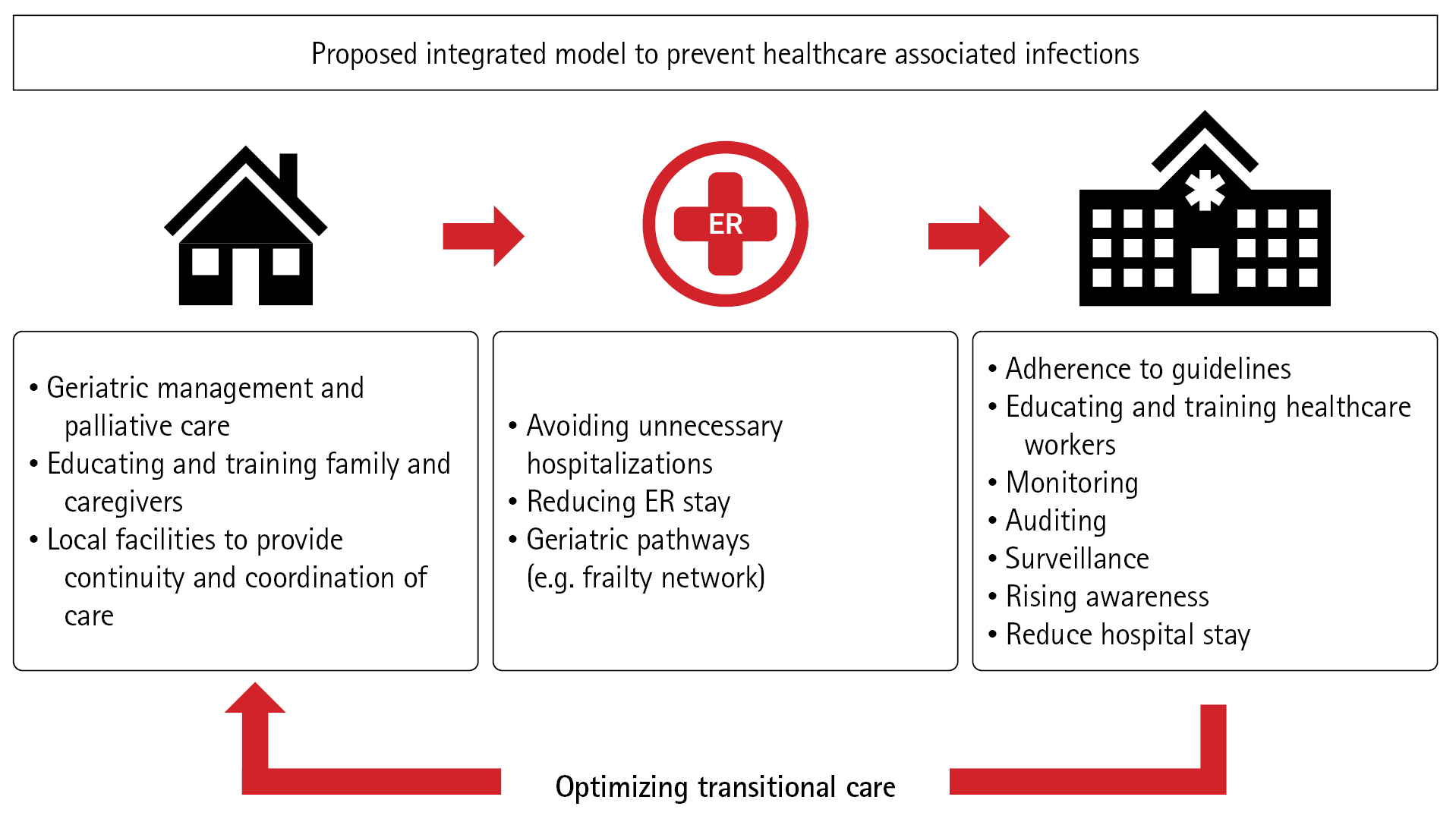
Frailty and hospital readmission are among the main risk factors for HAIs. The global population is increasing in number.16) In Italy, according to the latest report, 43% of the population aged over 65 years has severe non-communicable diseases, with the percentage increasing to >60% in older adults Ōēź85 years of age.17) A strict adherence to the guidelines established by the World Health Organization,18) appropriate training, auditing, and surveillance are crucial to protect frail patients from HAIs, as well as conducting campaigns to raise awareness among healthcare workers, patients, and visitors. In recent years, our hospital, the Fondazione Policlinico Universitario Agostino Gemelli IRCCS, has made great efforts and conducted several campaigns to fight HAIs.19) Nevertheless, much work remains to be done, and no one can let their guard down, as overlooking the risk of infection in hospitalized patients means exposing them to a potentially fatal threat. In this scenario, the need for more sustainable healthcare and the pivotal role of geriatricians is increasing.20) In hospitals, a more adequate model should involve a shorter length of stay in ERs and acute wards, creating senior-friendly hospitals with dedicated paths. One possible model is represented by the geriatric frailty network currently implemented in our hospital, which aims to assist emergency rooms and ward doctors in preventing the most common geriatric syndromes and reducing the number of incongruous hospitalizations. The characteristics of the proposed model have been discussed elsewhere.21) Attention should be paid to optimizing transitional care and ensuring better communication between hospitals and families, caregivers, and local facilities. The ultimate goal should be not only to optimize diagnostic and therapeutic procedures but also to avoid unnecessary ER readmissions by effectively managing frail and complex patients outside the hospital (Fig. 1).22,23)
In conclusion, we report a case of R. pickettii bloodstream infection in an 88-year-old woman with a relatively mild course. R. pickettii is one of several emerging healthcare-associated pathogens that affect frail older adult patients. Older age, comorbidities, and hospital admissions are among the main risk factors for HAIs. Adherence to guidelines, training, auditing, and surveillance is crucial for reducing the burden of HAIs. Furthermore, avoiding incongruous hospitalizations has positive implications both for preventing HAIs and improving patient quality of life. The possible strategies involve improving the transition-of-care processes, providing attentive follow-up to identify and treat possible causes of hospitalization, and ensuring both the patientsŌĆÖ and caregiversŌĆÖ compliance with discharge instructions. The true core of geriatric medicine should be primary care.
REFERENCES
1. Morley JE, Vellas B, van Kan GA, Anker SD, Bauer JM, Bernabei R, et al. Frailty consensus: a call to action. J Am Med Dir Assoc 2013;14:392ŌĆō7.



4. Gemelli Against COVID-19 Geriatrics Team, Landi F, Barillaro C, Bellieni A, Brandi V, Carfi A, et al. The geriatrician: the frontline specialist in the treatment of COVID-19 patients. J Am Med Dir Assoc 2020;21:937ŌĆō8.



5. Zahran S, Altringer L, Prasad A. The longevity-frailty hypothesis: evidence from COVID-19 death rates in Europe. Int J Environ Res Public Health 2022;19:2434.



6. Istituto Superiore di Sanita. [Healthcare-associated infection] [Internet]. Rome, Italy: Istituto Superiore di Sanita; c2022 [cited 2022 Dec 11]. Available from: https://www.epicentro.iss.it/infezioni-correlate/.
7. Cristina ML, Spagnolo AM, Giribone L, Demartini A, Sartini M. Epidemiology and prevention of healthcare-associated infections in geriatric patients: a narrative review. Int J Environ Res Public Health 2021;18:5333.



8. Ryan MP, Pembroke JT, Adley CC. Ralstonia pickettii: a persistent gram-negative nosocomial infectious organism. J Hosp Infect 2006;62:278ŌĆō84.

9. Stelzmueller I, Biebl M, Wiesmayr S, Eller M, Hoeller E, Fille M, et al. Ralstonia pickettii-innocent bystander or a potential threat? Clin Microbiol Infect 2006;12:99ŌĆō101.


10. Menekse S, Haciseyitoglu D, Suzuk Yildiz S, Bayrakdar F. An outbreak of Ralstonia pickettii bloodstream infection and clinical outcomes. J Infect Dev Ctries 2022;16:705ŌĆō11.



11. Birlutiu RM, Roman MD, Cismasiu RS, Fleaca SR, Popa CM, Mihalache M, et al. Sonication contribution to identifying prosthetic joint infection with Ralstonia pickettii: a case report and review of the literature. BMC Musculoskelet Disord 2017;18:311.




12. Oku S, Takeshita T, Futatsuki T, Kageyama S, Asakawa M, Mori Y, et al. Disrupted tongue microbiota and detection of nonindigenous bacteria on the day of allogeneic hematopoietic stem cell transplantation. PLoS Pathog 2020;16:e1008348.



13. Huang Y, Cao Y, Zou M, Luo X, Jiang Y, Xue Y, et al. A comparison of tissue versus swab culturing of infected diabetic foot wounds. Int J Endocrinol 2016;2016:8198714.




14. Pothier K, Gana W, Bailly N, Fougere B. Associations between frailty and inflammation, physical, and psycho-social health in older adults: a systematic review. Front Psychol 2022;13:805501.



15. Yao X, Li H, Leng SX. Inflammation and immune system alterations in frailty. Clin Geriatr Med 2011;27:79ŌĆō87.



16. United Nations. World population prospects 2022: summary of results [Internet]. New York, NY: United Nations; 2022 [cited 2022 Dec 11]. Available from: https://www.un.org/development/desa/pd/sites/www.un.org.development.desa.pd/files/wpp2022_summary_of_results.pdf.
17. Istituto Nazionale di Statistica. [The health of the elderly is improving but the demand for care and assistance is growing] [Internet]. Rome, Italy: Istituto Nazionale di Statistica; 2021 [cited 2022 Dec 11]. Available from: https://www.istat.it/it/files/2021/07/Report-anziani-2019.pdf.
18. World Health Organizaion. Guidelines on core components of infection prevention and control programmes at the national and acute health care facility level [Internet]. Geneva, Switzerland: World Health Organization; 2016 [cited 2022 Dec 11]. Available from: https://apps.who.int/iris/bitstream/handle/10665/251730/9789241549929-eng.pdf?sequence=.
19. Puro V, Coppola N, Frasca A, Gentile I, Luzzaro F, Peghetti A, et al. Pillars for prevention and control of healthcare-associated infections: an Italian expert opinion statement. Antimicrob Resist Infect Control 2022;11:87.




20. Cesari M, Marzetti E, Thiem U, Perez-Zepeda MU, Abellan Van Kan G, Landi F, et al. The geriatric management of frailty as paradigm of ŌĆ£The end of the disease eraŌĆØ. Eur J Intern Med 2016;31:11ŌĆō4.


21. Salini S, Giovannini S, Covino M, Barillaro C, Acampora N, Gravina EM, et al. Frailty network in an acute care setting: the new perspective for frail older people. Diagnostics (Basel) 2022;12:1228.



- TOOLS