|
 |
- Search
| Ann Geriatr Med Res > Volume 22(3); 2018 > Article |
|
Abstract
Background
Current guidelines recommended that chest compression depths during car-diopulmonary resuscitation (CPR) should be at least one-fifth of the external chest ante-riorposterior (AP) diameter. The chest AP diameter increases because of dorsal kyphosis, senile emphysema, and poor lung compliance associated with aging. This study aimed to compare the proportion of the heart compressed by chest compression (based on the ejection fraction [EF]) in geriatric and nongeriatric patients.
Methods
We performed a retrospective analysis of the chest computed tomography findings obtained between January 2010 and August 2016 and measured the chest anatomical parameters such as the perpendicular external and internal chest AP diameters with the heart AP diameter. Based on values of these parameters, EFs with 50- and 60-mm depths were obtained. In addition, we investigated and compared the proportion of 50- and 60-mm depths and heart AP to external chest AP diameter between the 2 groups.
Results
We randomly selected and analyzed 100 of 1,921 geriatric and 100 of 22,090 nongeriatric populations from a database. The means┬▒standard deviations of EFs with 50- and 60-mm depths for geriatric and nongeriatric people were 37.1%┬▒12.1% vs. 43.2%┬▒13.8% and 47.5%┬▒12.8% vs. 54.6%┬▒14.8%, respectively (all p<0.001). The proportion of 50- and 60-mm depths and heart AP to external chest AP diameter were significantly different between the 2 groups (all p<0.05).
The mean age of patients who experience out-of-hospital cardiac arrests vary from 49.7 to 71.7 years in 7 countries in Asia, while the average age of patients who experience cardiac arrest in Korea is 63.5┬▒19.0 years.1) Patients aged 65 years or older accounted for more than 50% of the total number of patients who experienced cardiac arrest in 2013 in Korea.2) The proportion of older patients who experience cardiac arrest may gradually increase. However, various studies on the survival rate of patients who experience cardiac arrest have demonstrated that as the age of a patient who experiences cardiac arrest increases, the likelihood that he or she will survive after cardiopulmonary resuscitation (CPR) decreases.3ŌĆō6)
The ŌĆ£Chain of SurvivalŌĆØ as an essential component of a series of actions designed to reduce mortality associated with cardiac arrest and includes early arrest recognition and emergency activation, early CPR, early defibrillation, expert advanced life support, and integrated postresus-citation care.7,8) Survival rates and favorable neurologic outcomes of patients who experience cardiac arrest are closely related to the quality of chest compressions during CPR.9,10) Chest compression depth is an important factor of high-quality chest compression and should be about 5 cm, but not exceed 6 cm in adult patients who experience cardiac arrest based on current guidelines.9,10) This depth of chest compression corresponds to one-fifth of the external chest depth and approximately 25%ŌĆō30% of the normal cardiac output.11)
However, dorsal kyphosis may develop in geriatric patients due to muscle weakness and degenerative disc diseases.12) Changes in the structure of the lungs are also mainly attributed to increases in the size of the alveolar space without any inflammation or alveolar wall destruction, so-called ŌĆ£senile emphysema,ŌĆØ resulting in the loss of the supporting structure of the lung parenchyma. Additionally, the elastic recoil capacity of the lungs is reduced with aging.13) Accordingly, the anteriorposterior (AP) diameter of the chest is increased in geriatric patients.14ŌĆō16) Therefore, the compressions performed in geriatric patients should be deeper than that performed in nongeriatric patients to deliver high-quality chest compressions and thus achieve sufficient cardiac output.
However, there is no mention of geriatrics as a specific subgroup potentially requiring adjustments in the chest compression technique in the current guidelines. To our knowledge, this is the first study to assess whether the chest compression depth according to the guidelines is sufficient for geriatric patients during CPR. We hypothesized that the chest AP diameter in geriatric patients is longer than that in younger patients and that the proportion of the heart compressed by chest compression with a 5- to 6-cm depth is insufficient in geriatric patients. We aimed to verify and compare the proportion of the heart compressed by chest compression between geriatric and non-geriatric patients based on the ejection fraction (EF) using mathematical methods and chest computed tomography (CT).
We performed a retrospective study to evaluate the differences in the proportion of the heart compressed by chest compression according to the international guidelines between geriatric and nongeriatric patients using chest CT. This study was performed at Hanyang University Hospital (Seoul, Korea) from March to June 2018 and was approved by the Institutional Review Board of Hanyang University Medical Centre (approval number: HYUH 2018-02-015).
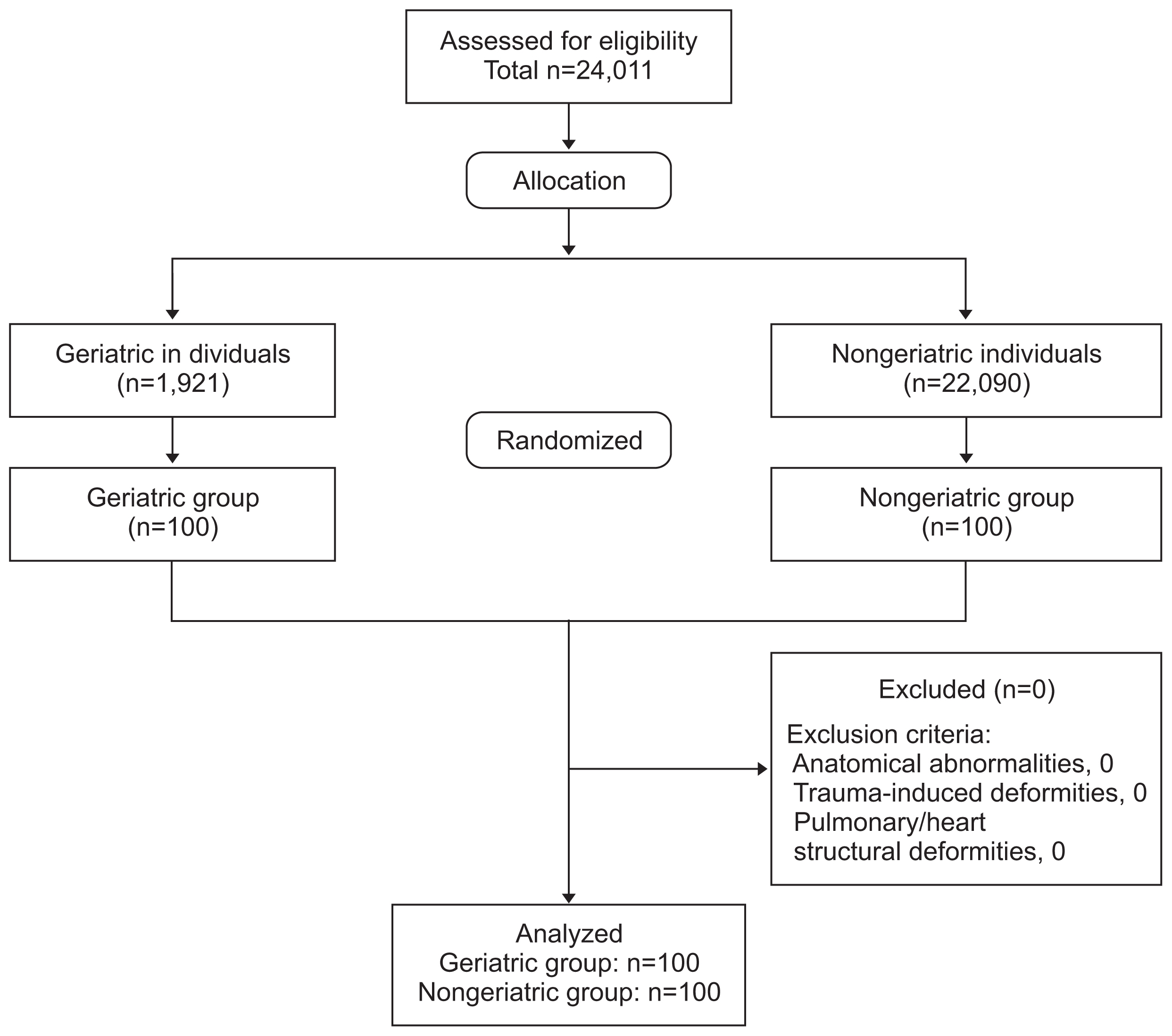
We extracted the medical records of 24,011 healthy individuals who underwent chest CT for health screening examination between January 2010 and August 2016. The inclusion criteria were age >18 years and no remarkable findings on chest CT. Patients with anatomical abnormalities such as pectus carinatum and excavatum in the chest, trauma-related deformities, or heart/pulmonary structural deformities were excluded. We divided the selected individuals into the geriatric (ageŌēź65 years) group and non-geriatric (age<65 years) group. Furthermore, we randomly included 100 individuals in the geriatric group and 100 individuals in the nongeriatric group using a Random Integer Set Generator (www.random.org). This program allows the extraction of as many random numbers as desired upon entering the number of variables.
We calculated that a minimum sample size of 200 individuals was required to observe a difference in the proportion of the heart compressed by chest compression with a 50-mm depth (i.e., [50 mm (internal chest AP diameter heart AP diameter)]/heart AP diameter├Ś100) between the 2 groups. We performed a pilot study with 100 individuals who were not included in this study using the soft package G-power 3.1.9 program (Heine Heinrich University, D├╝sseldorf, Germany) with an ╬▒ error of 0.05 and power of 0.95 considering a drop rate of 20% (mean┬▒standard deviation [SD]: 37.8%┬▒12.4% in the geriatric group and 45.0%┬▒12.9% in the nongeriatric group; effect size, 0.57) (Fig. 1).
The 2 types of CT equipment used in this study were the Somatom Definition Flash (Siemens Healthcare, Forchheim, Germany) and Brilliance 64 multi-detector CT scanner (Philips Healthcare, Best, the Netherlands). The settings were as follows: 120 kVp, 50ŌĆō80 mAs, 1.15-mm/sec table feed, 0.5-sec rotation time, 5-mm slice thickness, and 5-mm intervals. All CT images were stored in the picture archiving and communication system (PACS, Centricity, GE Healthcare, Milwaukee, WI, USA).
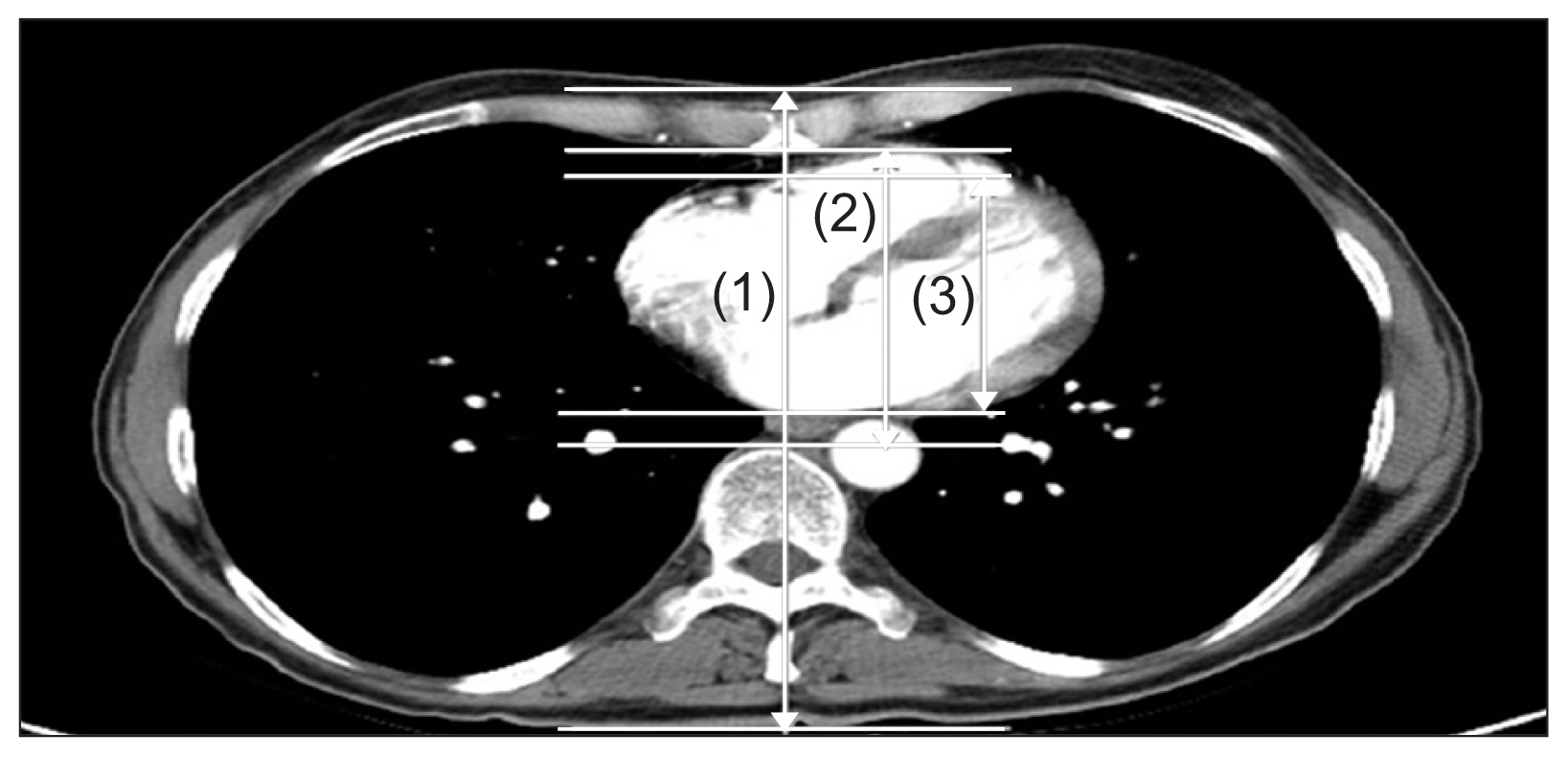
We collected patientsŌĆÖ basic characteristics, such as age, sex, height, weight, and body mass index (BMI). All CT images for each patient were reconstructed and shown as axial and midsagittal views using the PACS. Each image was simultaneously cross-linked to the images acquired with other setting. Two emergency physicians conducted the reconstruction of all the images of each patient. They measured the following parameters using a 3-dimensional image solution program (Rapidia, Version 2.8, Infinite, Seoul, Korea) with consensus (Fig. 2).17)
We estimated several parameters on the axial view that showed the midpoint of the lower half of the sternum in two groups: (1) external chest AP diameter (mm), from the skin on the sternum vertically to the skin on the back; (2) internal chest AP diameter (mm), from under the surface of the sternum vertically to the anterior longitudinal ligament on the body of the vertebra; and (3) heart AP diameter (mm), anterior to posterior diameter of the heart in line with the external and internal AP diameter. Finally, we hypothesized EF with a cardiac compression model to generate blood flow during chest compression. Variables in decompression state are defined as follows: x, chest compression depth; h, heart AP diameter; and d, noncardiac thoracic tissue which was subtracted heart AP diameter from internal chest AP diameter.18,19) We assumed that noncardiac thoracic tissue absorbed the compression force and was entirely compressed during the chest compression. As a result, the rest of the compression force (xŌĆōd) would be delivered to the heart and EF could be calculated as follows:
The primary outcome was the EF with a 50-mm depth, which was the proportion of the heart compressed by chest compressions with a 50-mm depth: [50 mm (internal chest AP diameter heart AP diameter)]/heart AP diameter├Ś100
In addition, the EF with a 60-mm depth was the proportion of the heart compressed by chest compressions with a 60-mm depth (i.e., [60 mm (internal chest AP diameter heart AP diameter)]/heart AP diameter├Ś100). The proportion of 50- and 60-mm depths and heart AP diameter to external chest AP diameter were investigated as secondary outcomes.
Data were entered into an Excel spreadsheet (Excel 2016; Microsoft, Redmond, WA, USA) and analyzed using IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA). The categorical data are shown as the frequency and percentage, and the continuous data as the median and inter-quartile range because they were not normally distributed. Kolmogorov-Smirnov tests were performed for all datasets with normal distribution. The Student t-test or Mann-Whitney U-test was used for comparisons of continuous variables, and the chi-square test or Fisher exact test was used to analyze categorical variables. Analysis of covariance (ANCOVA) was performed to adjust the influencing factors and investigate the main factor influencing the outcomes. A value of p<0.05 was considered significant. The partial eta squared (╬Ę2) values were 0.01 (small), 0.06 (medium), and 0.14 (large).
We included 100 records of 1,921 geriatric and 100 of 22,090 nongeriatric people for this study; among these, none of the people was excluded because of chest abnormalities/pathologies (Fig. 1). The baseline characteristics of the individuals are summarized in Table 1. No significant differences in sex and BMI were observed between the 2 groups. However, mean┬▒SD values of height and weight in the nongeriatric group were higher than those in the other group (p<0.001 and p=0.003, respectively).
The values of the chest anatomical parameters measured using CT are summarized in Table 2. There were significant differences in external chest, internal chest, and heart AP diameters between the two groups. The mean┬▒SD values of EFs with 50-mm depth in the geriatric group and nongeriatric group were 37.1%┬▒12.1% and 43.2%┬▒13.8%, respectively (p<0.001) (Table 3). EFs with 60-mm depth were 47.5%┬▒12.8% (geriatric group) and 54.6%┬▒14.8% (nongeriatric group) (p<0.001) (Table 3). The proportion of 50- (21.7%┬▒2.5% vs. 23.1%┬▒3.2%) and 60-mm (26.6%┬▒2.9% vs. 28.2%┬▒3.8%) depths and heart AP to external chest AP diameter (42.5%┬▒3.3% vs. 41.5%┬▒2.9%) were significantly different between the 2 groups (p=0.001, p=0.001, and p=0.03, respectively).
We adjusted for the influencing factors that could affect the results of the chest anatomy parameters and outcomes using ANCOVA. Significant differences were observed in all chest anatomy parameters and outcomes between the two groups (p<0.001), except in the proportion of heart to external chest AP diameter (p=0.07) after adjusting for sex, height, and BMI (Table 4).
Chest compressions generate a small, but critical amount of blood flow to the brain and myocardium and increase the likelihood of a successful defibrillation by increasing intrathoracic pressure and directly compressing the heart.20,21) We measured the chest parameter and outcomes based on the theory of direct heart compression using chest CT. A chest compression depth of one-third of the chest AP diameter for both pediatric and infant CPR has been suggested, but it was not adopted for adult CPR during the preparation of the European Resuscitation Council guidelines.10,21) A chest compression depth of 4ŌĆō5 cm in adults equates to approximately one-fifth of the AP diameter of the adult chest,18) and Nestaas et al.22) reported that compressing the recommended 5 cm corresponded to 20%ŌĆō23% of the external chest diameter. We also found that a chest compression depth of 50 mm comprised about one-fifth of the external chest AP diameter in geriatric and nongeriatric patients, while a chest compression depth of 60 mm comprised about one-fourth of it in both groups. A chest compression depth corresponding to one-third of the chest AP diameter might not be suitable for both groups. In the mathematical model based on neonatal chest CT, Meyer et al.19) assumed that an estimated EF <50% indicates undercompression.
In this study, the mean EFs with a 50-mm depth were 37.1%┬▒12.1% (geriatric group) and 43.2%┬▒13.8% (nongeriatric group), which reflected under-compression. The mean EFs with a 60-mm depth increased in both groups but did not reach 50% in the geriatric group. The EF with a 60-mm depth in the geriatric group (47.5%┬▒12.8%) was not significantly different from the EF with a 50-mm depth in the nongeriatric group after adjusting for sex, height, and BMI (p=0.08). A 5-mm increase in the chest compression depth was found to be associated with a 2-fold increase in shock success in in-hospital and out-of-hospital resuscitations.23) The number of people today aged 60 years or older has doubled since 1980, and the number of people aged 80 years or older almost quadrupled to 395 million between now and 2050.24) The aged population in Korean purportedly accounted for 14.3% of the total population in 2018 and is forecasted to upsurge to 20.0% in 2025, by which time the country will consist of a super-aged society.25) Chest compressions performed in geriatric patients who experience cardiac arrests should be deeper than that performed in other patients to deliver sufficient high-quality chest compressions. However, the increasing rate of complications such as sternum and rib fractures, hematomas associated with rib fractures, pneumothorax, hemothorax, etc. secondary to deeper chest compressions remains a concern. Common complications such spontaneously healing rib fractures or hematomas only have a minor impact on patients who experienced cardiac arrest.26,27)
The differences between sex and body size, including height, weight, and BMI, were not included in the current guidelines. Lee et al.28) noted that the internal and external chest depth increased with increase in BMI. However, the mean age of the patients was 46.1┬▒9.2 years, not including elderly patients. Sex and age were significant explanatory factors for external chest AP depth, whereas only sex was significant for the inner diameters of the intrathoracic blood-filled structures and the ratio of their inner diameters to the external chest AP depth.22) We found that external chest AP and heart AP diameters regarded as the intrathoracic blood-filled structures were different between the 2 groups after adjustment for influencing factors (sex, height, and BMI), whereas the proportion of heart AP to external chest AP diameter was not significantly different between them. Other parameters and the outcomes were still different between the 2 groups after adjusting for influencing factors (sex, height, and BMI). Wang et al.29) reported that patients who experienced in-hospital cardiac arrest with greater BMI and showed external chest depth had worse survival and neurologic outcomes. Hence, we believe that aging, in addition to sex and BMI, could also influence the performance of high-quality chest compressions and thus affect the survival and neurologic outcomes.
This study have several limitations. First, the CT scans were performed in people who had normal anatomical structure of the thorax. We could not address the anatomic variations of patients who had a higher risk of cardiac arrest, such as those with hypertension, diabetes, and hyperlipidemia. Second, the CT scans were obtained while patients were holding their breath deeply during the scanning. The different respiratory phases may affect the precise measurement of the length and the conformational changes in intrathoracic structures. Third, we did not account the changes in intrathoracic pressure during chest compression. There are 2 theories to explain the mechanism of blood flow during CPR: the ŌĆ£Cardiac PumpŌĆØ theory and the ŌĆ£Thoracic PumpŌĆØ theory. We designed our EF calculation formula based only on the ŌĆ£Cardiac PumpŌĆØ theory. However, we were not able to determine how the thoracic cage and pulmonary changes, which happen as the person ages, influence the EF during chest compression. Finally, the CT images were not obtained during real CPR situations. We could not count the possibility that the thoracic structures might relocate during CPR. Hence, further research is required to determine if spontaneous cardiopulmonary circulation recovery rates and survival rates are effective with deeper chest compressions in geriatric individuals in actual cardiac arrest situations.
In this study, we observed that the external and internal chest and heart AP diameters in geriatric patients are longer than those in nongeriatric patients. The chest compression depth in current guidelines is not sufficient in geriatric patients during CPR, and deeper chest compressions would be considered.
ACKNOWLEDGMENTS
This study was supported by the Korean Geriatrics Society (2017). We thank Professor Nam E in the Biostatistical Consulting and Research Lab, Hanyang University, for his assistance with statistical analysis.
Fig.┬Ā2
Chest anatomy measurements on the axial view on the middle point level of the lower half of the sternum using chest computed tomography. (1) External AP diameter (mm), from the skin on the sternum vertically to the skin on the back. (2) Internal AP diameter (mm), from under the surface of the sternum vertically to the anterior longitudinal ligament on the body of the vertebra. (3) Heart AP diameter (mm), AP diameter of heart in line with the external and internal AP diameter. AP, anteriorposterior.
Table┬Ā1
Baseline characteristics of individuals in the geriatric (ageŌēź65 years) and nongeriatric (age<65 years) groups
| Variable | Geriatric group (n=100) | Nongeriatric group (n=100) | p-value |
|---|---|---|---|
| Age (yr) | 74.1┬▒6.1 | 40.5┬▒15.2 | <0.001* |
| Male sex | 51 (51.0) | 51 (51.0) | 1.00 |
| Height (cm) | 160.1┬▒9.1 | 168.4┬▒10.7 | <0.001* |
| Weight (kg) | 61.3┬▒12.0 | 67.2┬▒15.6 | 0.003* |
| Body mass index (kg/m2) | 24.0┬▒4.1 | 23.6┬▒4.7 | 0.62 |
Table┬Ā2
Comparison of chest anatomy parameters based on computed tomography measurement between the geriatric (ageŌēź65 years) and nongeriatric (age<65 years) groups
| Variable | Geriatric group (n=100) | Nongeriatric group (n=100) | p-value |
|---|---|---|---|
| External chest AP diameter (mm) | 228.4┬▒25.5 | 216.6┬▒29.4 | 0.03* |
| Internal chest AP diameter (mm) | 111.7┬▒17.3 | 102.1┬▒18.5 | <0.001* |
| Heart AP diameter (mm) | 96.9┬▒12.8 | 89.8┬▒13.6 | <0.001* |
Table┬Ā3
Comparison of EF by chest compression and the proportion of 50- and 60-mm depths and heart AP to external AP diameter based on computed tomography measurement between the geriatric (ageŌēź65 years) and nongeriatric (age<65 years) groups
| Variable | Geriatric group (n=100) | Nongeriatric group (n=100) | p-value |
|---|---|---|---|
| EF with 50-mm depth (%) | 37.1┬▒12.1 | 43.2┬▒13.8 | 0.001* |
| EF with 60-mm depth (%) | 47.5┬▒12.8 | 54.6┬▒14.8 | <0.001* |
| The proportion of 50 mm to external chest AP diameter (%) | 21.7┬▒2.5 | 23.1┬▒3.2 | 0.001* |
| The proportion of 60 mm to external chest AP diameter (%) | 26.6┬▒2.9 | 28.2┬▒3.8 | 0.001* |
| The proportion of heart AP to external chest AP diameter (%) | 42.5┬▒3.3 | 41.5┬▒2.9 | 0.03* |
Table┬Ā4
Adjustment for influencing factors of chest anatomy parameters and outcomes
| Variable | p-value (ANCOVA) | Partial eta squared (╬Ę2) |
|---|---|---|
| Chest anatomy parameters | ||
| ŌĆāExternal AP diameter | <0.001* | 0.15 |
| ŌĆāInternal AP diameter | <0.001* | 0.10 |
| ŌĆāHeart AP diameter | <0.001* | 0.13 |
| Outcomes | ||
| ŌĆāEF with 50-mm depth | <0.001* | 0.06 |
| ŌĆāEF with 60-mm depth | <0.001* | 0.08 |
| ŌĆāThe proportion of 50 mm to external chest AP diameter (%) | <0.001* | 0.17 |
| ŌĆāThe proportion of 60 mm to external chest AP diameter (%) | <0.001* | 0.17 |
| ŌĆāThe proportion of heart AP to external chest AP diameter (%) | 0.07 | 0.02 |
ANCOVA, analysis of covariance; AP, anteriorposterior; EF, ejection fraction: the proportion of the heart compressed by chest compression.
REFERENCES
1. Ong ME, Shin SD, De Souza NN, Tanaka H, Nishiuchi T, Song KJ, et al. Outcomes for out-of-hospital cardiac arrests across 7 countries in Asia: The Pan Asian Resuscitation Outcomes Study (PAROS). Resuscitation 2015;96:100ŌĆō8.


2. Yoon HD, Kim SW, Kim JS, Lee MH, Lee JT. 2013. Cardiac arrest registry ver 3.0 data analysis report. Seoul (Korea): National Emergency Medical Center; 2014.
3. Beesems SG, Blom MT, van der Pas MH, Hulleman M, van de Glind EM, van Munster BC, et al. Comorbidity and favorable neurologic outcome after out-of-hospital cardiac arrest in patients of 70 years and older. Resuscitation 2015;94:33ŌĆō9.


4. Herlitz J, Eek M, Engdahl J, Holmberg M, Holmberg S. Factors at resuscitation and outcome among patients suffering from out of hospital cardiac arrest in relation to age. Resuscitation 2003;58:309ŌĆō17.


5. Rogove HJ, Safar P, Sutton-Tyrrell K, Abramson NS. Old age does not negate good cerebral outcome after cardiopulmonary resuscitation: analyses from the brain resuscitation clinical trials. The Brain Resuscitation Clinical Trial I and II Study Groups. Crit Care Med 1995;23:18ŌĆō25.


6. Bae J, Oh J, Lee S, Lim TH, Kang H, Lee J. Analysis of the performance for bystanders; cardiopulmonary resuscitation in geriatric and out-of-hospital cardiac arrested patients. Ann Geriatr Med Res 2016;20:118ŌĆō24.

7. American Heart Association in collaboration with International Liaison Committee on Resuscitation. Guidelines 2000 for Cardio-pulmonary Resuscitation and Emergency Cardiovascular Care: Part 12: from science to survival. Circulation 2000;102(Suppl 1):358ŌĆō370.
8. Dumas F, Rea TD, Fahrenbruch C, Rosenqvist M, Fax├®n J, Svensson L, et al. Chest compression alone cardiopulmonary resuscitation is associated with better long-term survival compared with standard cardiopulmonary resuscitation. Circulation 2013;127:435ŌĆō41.


9. Kleinman ME, Brennan EE, Goldberger ZD, Swor RA, Terry M, Bobrow BJ, et al. Part 5: adult basic life support and cardiopulmonary resuscitation quality: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015;132(18 Suppl 2):S414ŌĆō35.


10. Perkins GD, Handley AJ, Koster RW, Castr├®n M, Smyth MA, Olas-veengen T, et al. European resuscitation council guidelines for resuscitation 2015: section 2. Adult basic life support and automated external defibrillation. Resuscitation 2015;95:81ŌĆō99.


11. Paradis NA, Martin GB, Rivers EP, Goetting MG, Appleton TJ, Feingold M, et al. Coronary perfusion pressure and the return of spontaneous circulation in human cardiopulmonary resuscitation. JAMA 1990;263:1106ŌĆō13.


12. Katzman WB, Wanek L, Shepherd JA, Sellmeyer DE. Age-related hyperkyphosis: its causes, consequences, and management. J Orthop Sports Phys Ther 2010;40:352ŌĆō60.



13. Brandsma CA, de Vries M, Costa R4, Woldhuis RR, K├Čnigshoff M, Timens W. Lung ageing and COPD: is there a role for ageing in abnormal tissue repair? Eur Respir Rev 2017 Dec 6 26(146):pii: 170073. https://doi.org/10.1183/16000617.0073-2017.

14. Schr├Čder TH, Storbeck B, Rabe KF, Weber C. The aging lung: clinical and imaging findings and the fringe of physiological state. Rofo 2015;187:430ŌĆō9.



15. In: Minaker Kenneth L, Common clinical sequelae of aging. In: Goldman L, Auseello D, editors. Cecil medicine. 22nd ed. Philadelphia (PA): Elsevier Saunders; 2004. p. 107.

16. In: Lee DW, Park SH, Cho KH, Human aging. In: Cho KH, Michel JP, Bludau J, Dave J, Park SH, Kwak I, , editors. Textbook of geriatric medicine international. 2010 ed. Seoul (Korea): Argos; 2010. p. 21.
17. Lee J, Oh J, Lim TH, Kang H, Park JH, Song SY, et al. Comparison of optimal point on the sternum for chest compression between obese and normal weight individuals with respect to body mass index, using computer tomography: a retrospective study. Resuscitation 2018;128:1ŌĆō5.


18. Pickard A, Darby M, Soar J. Radiological assessment of the adult chest: implications for chest compressions. Resuscitation 2006;71:387ŌĆō90.


19. Meyer A, Nadkarni V, Pollock A, Babbs C, Nishisaki A, Braga M, et al. Evaluation of the Neonatal Resuscitation ProgramŌĆÖs recommended chest compression depth using computerized tomography imaging. Resuscitation 2010;81:544ŌĆō8.


20. Wik L, Hansen TB, Fylling F, Steen T, Vaagenes P, Auestad BH, et al. Delaying defibrillation to give basic cardiopulmonary resuscitation to patients with out-of-hospital ventricular fibrillation: a randomized trial. JAMA 2003;289:1389ŌĆō95.


21. Handley AJ, Koster R, Monsieurs K, Perkins GD, Davies S, Bossaert L, et al. European Resuscitation Council guidelines for resuscitation 2005. Section 2. Adult basic life support and use of automated external defibrillators. Resuscitation 2005;67(Suppl 1):S7ŌĆō23.


22. Nestaas S, Stens├”th KH, Rosseland V, Kramer-Johansen J. Radiological assessment of chest compression point and achievable compression depth in cardiac patients. Scand J Trauma Resusc Emerg Med 2016;24:54



23. Edelson DP, Abella BS, Kramer-Johansen J, Wik L, Myklebust H, Barry AM, et al. Effects of compression depth and pre-shock pauses predict defibrillation failure during cardiac arrest. Resuscitation 2006;71:137ŌĆō45.


24. World Health Organization. Are you ready? What you need to know about ageing [Internet] Geneva (Switzerland): World Health Organization; c2018 [cited 2018 Jul 10]. Available from: http://www.who.int/world-health-day.
25. Statistics Korea. 2017 Elderly statistics [Internet] Daejeon (Korea): Statistics Korea; c2017 [cited 2017 Sep 26]. Available from: http://kostat.go.kr/portal/korea/kor.
26. Beom JH, You JS, Kim MJ, Seung MK, Park YS, Chung HS, et al. Investigation of complications secondary to chest compressions before and after the 2010 cardiopulmonary resuscitation guideline changes by using multi-detector computed tomography: a retrospective study. Scand J Trauma Resusc Emerg Med 2017;25:8




27. Hellevuo H, Sainio M, Nevalainen R, Huhtala H, Olkkola KT, Tenhunen J, et al. Deeper chest compression - more complications for cardiac arrest patients? Resuscitation 2013;84:760ŌĆō5.