INTRODUCTION
Multiple myeloma (MM) is a plasma cell disorder characterized by the proliferation of clonal plasma cells in the bone marrow.
1) Nonsecretory multiple myeloma (NSMM) is a rare variant of MM first described in the 1950s, which accounts for approximately 1% to 5% of myeloma cases.
2) NSMM is a symptomatic myeloma characterized by the absence of detectable monoclonal immunoglobulin (Ig) in the serum or urine on electrophoresis.
3) Therefore, the diagnosis of NSMM can be delayed and nonspecific symptoms, which often present in patients with NSMM, make the diagnosis more difficult. The case described herein misled doctors by presenting as vertebral compression fractures in an older man with osteopenia.
CASE REPORT
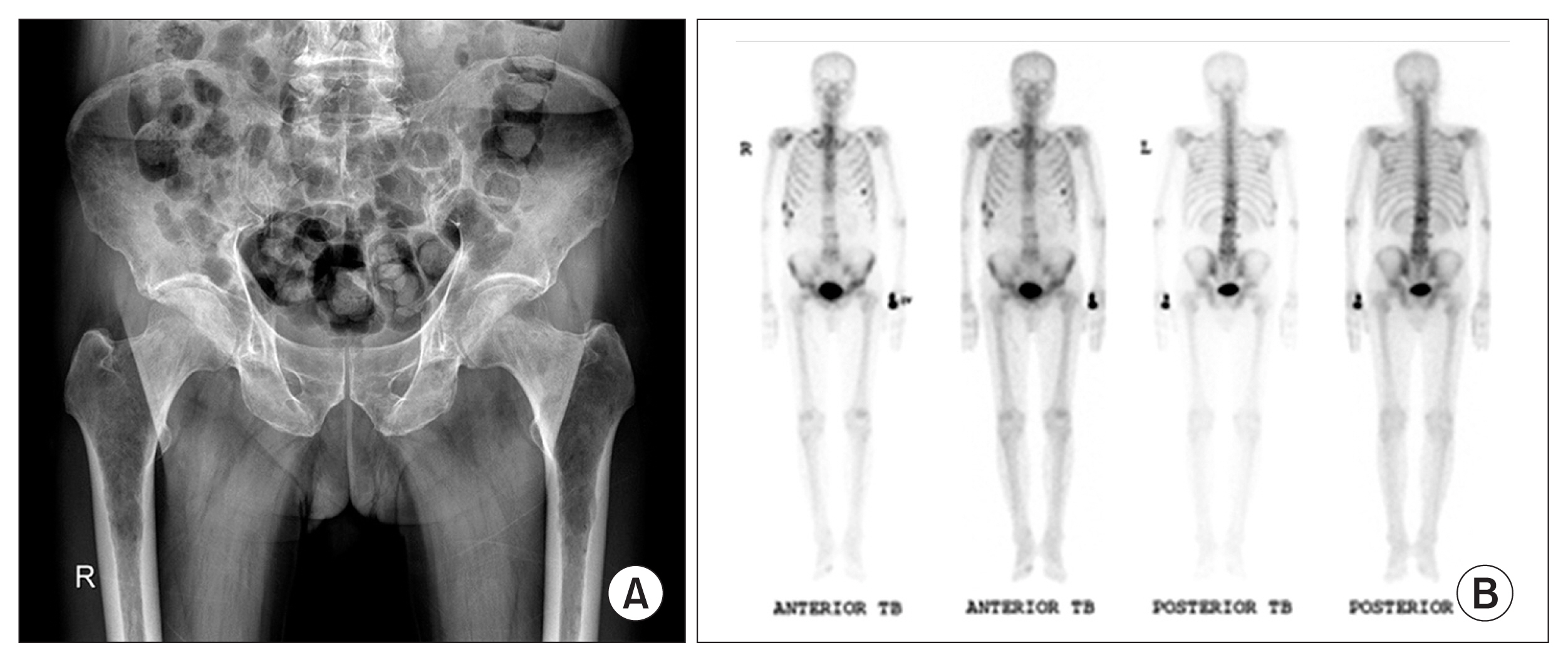
A 70-year-old man with a past medical history of dyslipidemia was referred to Jeju National University Hospital with a 5-month history of recurrent vertebral compression fractures with back pain. He suddenly had back pain while changing his pants and was treated for T11 and L3 vertebral compression fractures 5 months prior. He had slipped down on the stairs, landing on his backside, and was hospitalized for treatment of L2 and L4 vertebral compression fractures 2 months prior. He had felt back pain while sneezing and had difficulty in walking 5 days prior. Eventually, he was referred to our hospital. Bone densitometry of the spine from previous hospital visits revealed osteopenia, and magnetic resonance imaging (MRI) of the lumbar spine from a previous hospital visit showed multiple compression fractures of the vertebral bodies with inconspicuous retropulsion of the cortex into the spinal canal (
Fig. 1A). X-ray images of the T-L spine (
Fig. 1B) revealed degenerative changes with compression fractures at T12, and the L1 to L3 vertebral bodies and the pelvic bones (
Fig. 2A) showed osteopenia. A bone scan (
Fig. 2B) showed a vertebral compression fracture in the L1 spine area; post-traumatic changes in the right first and eighth to tenth ribs and the left sixth rib; and arthritic and degenerative changes in the T9 to L5 spines and both hip joint areas.
Laboratory tests did not reveal specific results. The hemoglobin level was 11.0 g/dL, showing normocytic normochromic anemia on the peripheral blood smear. We also noted the absence of hypercalcemia (8.9 mg/dL), and a normal serum creatinine level of 0.78 mg/dL. Laboratory tests and imaging studies did not provide evidence to suspect that the recurrent compression fractures may have resulted from osteoporosis, metabolic diseases such as hyperparathyroidism, Paget disease and other metabolic processes, or obvious tumors. Therefore, serum and urine protein electrophoresis were conducted for the differential diagnosis of MM. Serum protein electrophoresis did not reveal abnormal Ig levels and the patientŌĆÖs gamma globulin levels were normal. Urine protein electrophoresis showed no monoclonal protein in any significant fraction. Consequently, a presumptive diagnosis of vertebral compression fractures with osteopenia was made, and conservative management was undertaken for 2 weeks.
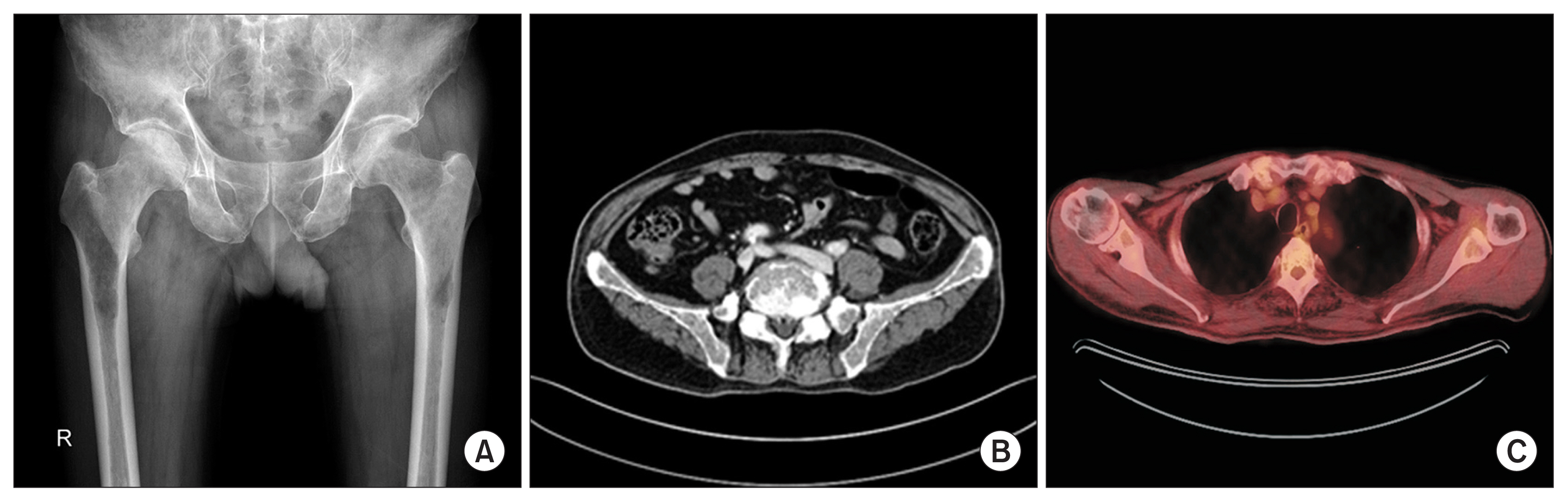
However, the patient complained of right hip pain during his first ambulation after conservative management. Hip X-ray images (
Fig. 3A) suggested several osteolytic lesions, and computed tomography detected multiple inconspicuous osteolytic lesions with greater variegation in opacity than expected in the spine, pelvic bones, both femurs, and ribs, suggesting MM or metastasis (
Fig. 3B). In addition, positron emission tomography revealed a high possibility of bone metastasis or bone-related malignancy based on a significant abnormal 18F-fluorodeoxyglucose uptake in the skull, spine, sternum, ribs, scapula, pelvic bones, and both femurs (
Fig. 3C). Moreover, a serum free light chain (SFLC) assay revealed elevated levels of kappa free light chain (12.667 mg/dL) and abnormal free light chain ratios with free lambda (1.105 mg/dL).
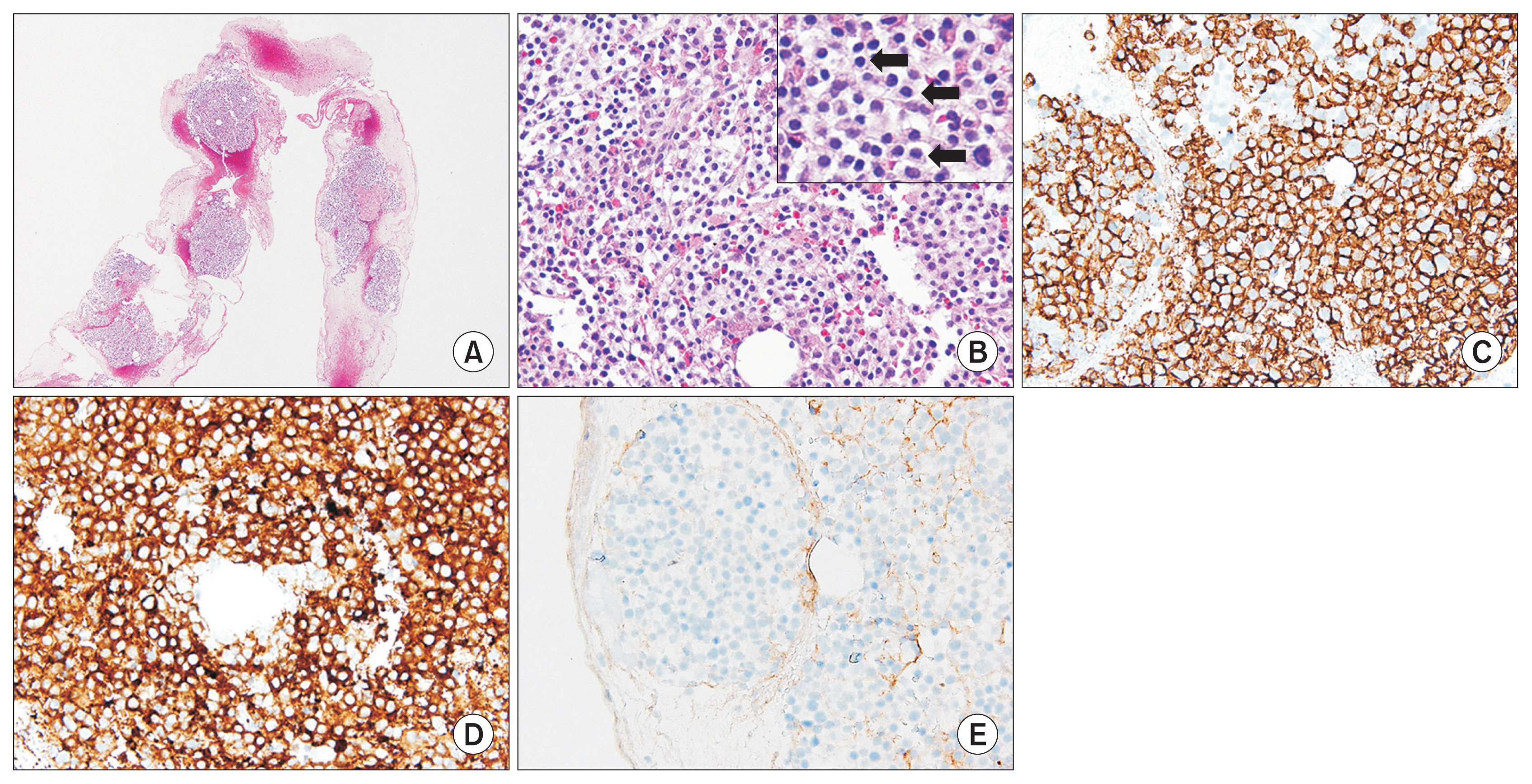
Therefore, we performed a bone marrow biopsy for the definitive diagnosis of NSMM. The marrow was mildly to moderately hypercellular and infiltrated by plasmacytoid cells in clusters with some normal hematopoietic cells (
Fig. 4A, B). The plasmacytoid cells showed reactivity to CD138 (
Fig. 4C) and kappa free light chain on immunohistochemical staining (
Fig. 4D), with no reactivity to lambda light chain (
Fig. 4E), which supports monoclonal plasma cell proliferation and favors the diagnosis of MM. Finally, the patient was diagnosed with NSMM 7 months since the onset of the first symptom and was referred to the oncology center for further management and therapy.
DISCUSSION
MM is a common bone marrow-based hematologic malignancy and multifocal plasma cell neoplasm usually associated with the presence of monoclonal Ig in the serum or urine.
4,5) The definition of MM from the 2014 International Myeloma Working Group includes 10% or more clonal plasma cells in the bone marrow or biopsy-proven bony or extramedullary plasmacytoma and one or more of the seven listed criteria (hypercalcemia, renal insufficiency, anemia, bone lesions, clonal bone marrow plasma cells Ōēź60%, involved/uninvolved SFLC ratio Ōēź100 and involved SFLC concentration Ōēź10 mg/dL, and 2 or more focal lesions based on MRI studies of the skeleton).
6)
The International Myeloma Working Group still defines NSMM as MM lacking monoclonal protein on serum or urine electrophoresis.
7) However, this definition is probably not sufficient since an Ig component is actively secreted in MM.
7) Thus, NSMM patients can more accurately be divided into at least 4 groups with separate molecular mechanisms
6,7):
(1) Oligo secretors/FLC-restricted MMs: this tumor is a subset with impaired secretion among tumors with defects in Ig production, which can produce small amounts of light chains. Their protein secretion may not be as high as that seen in typical myeloma, but it can be measured by the SFLC assay. Oligosecretory MM is often characterized by SFLC values <10 mg/dL. Our case is included in this group.
(2) Nonproducers: in these cases, there is complete and real absence of Ig production, resulting in no secretion and no measurable protein in the blood or urine. True nonsecretory myeloma should only be considered this group.
(3) True nonsecretors: these MM cells produce Ig molecules but are unable to secrete them.
(4) False nonsecretors: these are MM variants or related plasma cell diseases with measurable levels of intra-cellular Ig by immunofluorescence assay but without measurable extracellular components by typical testing, despite clear pathologic evidence that they are secreted, such as Ig deposits found in renal biopsies.
NSMM is a rare variant of MM and the clinical features of NSMM are generally similar to those of secretory MM except for a lower incidence of renal insufficiency and hypercalcemia.
2,5) The clinical course and prognosis of NSMM have not been well studied, since assessment of response and identification of relapse are more difficult given the absence of the monoclonal protein typically used for this purpose in the clinical settings.
8) However, based on current studies, NSMM appears to be less aggressive than secretory MM.
4) Chawla et al.
8) examined the survival and prognosis of 124 NSMM patients in a retrospective study, and the study included SFLC testing where available.
4) They demonstrated that time to progression, progression-free survival, and overall survival prior to 2001 were similar between NSMM patients and secretory MM patients.
4) Between 2001 and 2012, the time frame during which new therapeutics were broadly introduced, there was a marked increase of overall survival in both groups.
4) However, the improvement in overall survival was greater in the NSMM group.
4) In addition, the overall survival was superior in patients with a normal baseline FLC ratio compared to that in patients with an abnormal ratio.
8)
Vertebral collapse with back pain is a common symptom of MM. However, a delayed diagnosis of MM is not uncommon because vertebral compression fractures are relatively prevalent, especially in elderly with osteoporosis; 10% to 25% of patients with MM present with diffuse osteopenia instead of osteolytic lesions, with or without fractures.
9) Furthermore, the diagnosis of NSMM with vertebral compression fractures in the elderly is difficult because these patients have no detectable monoclonal proteins in their serum or urine, as discussed above.
2,5) Therefore, the diagnosis of NSMM depends on a high suspicion of the disease.
Several case reports have described multiple vertebral fractures in NSMM. These cases showed usually myeloma-defining events such as multiple conspicuous osteolytic lesions on MRI or X-ray images, anemia, hypercalcemia, and renal insufficiency. However, our case did not reveal distinct evidence of myeloma on MRI and laboratory tests and also showed vertebral compression fractures with osteopenia on X-ray images of the T-L spine instead of osteolytic lesions. Therefore, we emphasize that recurrent vertebral compression fractures may result from MM if laboratory tests and imaging studies do not provide evidence that the compression fractures have occurred due to osteoporosis, metabolic diseases such as hyperparathyroidism, Paget disease and other metabolic processes, or obvious tumors.
In conclusion, MM can be included in the differential diagnosis of recurrent vertebral compression fractures, despite the lack of detectable monoclonal Ig in the serum or urine by electrophoresis. We recommend bone marrow aspiration, bone marrow biopsy, or biopsy of the osteolytic lesion, SFLC assay and testing for the presence of intracellular Ig by immunofluorescence if NSMM is suspected.