Korea has shown the fastest aging trend worldwide. The country moved from an aging to an aged society in only 17 years, a change that took 24 years in Japan, which now has a super-aged society.1,2) Korea is expected to reach super-aged society status, with older people comprising 20% of the population, in 2025, only 8 years after reaching the status of an aged society. The effect of an aging population is intensified by the speed at which aging occurs.3) The change in aging status requires urgent action to avoid social shock, which is led by fast population aging. In 2008, the Korean government launched the Long-Term Care Insurance (LTCI) system to provide daily living assistance for disabled older people. While people welcomed and appreciated LTCI benefits, there have been criticisms of the lack of home and community LTCI care in terms of both quantity and quality. With regard to the current long-term care resources in Korea, many older people live and receive care in residential aged care facilities (RACFs) or long-term hospitals (LTHs) rather than in their own homes. The benefits for RACFs in the LTCI system and LTHs in the National Health Insurance (NHI) system have rapidly increased.4,5) However, there is concern regarding not only financial burden but also the quality of life in the LTCI and NHI systems. Most older people are admitted to RACFs on the basis of decisions made by their family members rather than of their own will.6) Moreover, issues concerning the segmentation and/or overlap of the care services provided by social insurance and welfare systems on the basis of taxes have consistently increased. Policy reforms targeting the LTCI, NHI, and welfare systems have been a recent concern.
The Korean government introduced the notion of Community Care (CC) in 2018.7) CC aims to provide sufficient integrated home and community care services for physically or mentally frail people—mostly older people—to prevent institutionalized long-term care. This marks the realization of “aging in place”.8) The key components of CC are health services, long-term care, supported housing, and welfare services. The delivery system for components of CC is a separate aspect. The central government—the unions of the Ministry of Health and Welfare, Ministry of the Interior and Safety, and Ministry of Land, Infrastructure and Transport—announced the CC road map in 2018 and started a pilot project to develop a customized CC model.9)
In the process of designing the CC road map, the government planned a delivery system centered around the local government by referencing other countries such as Japan, Denmark, and the United Kingdom. The local governments assess the multiple care needs of their people and arrange for care to meet these needs. However, the social context and policy circumferences, including the health and social security system, are unique and different from those mentioned above.
In Korea, the health and long-term care systems are covered by one national insurer, the National Health Insurance Service (NHIS), which is separated from the local government, unlike that in other countries. Most Koreans have universal coverage for health and long-term care—that is, all Korean people can access the health and LTCI service regardless of their addresses and socioeconomic position. However, the welfare service coverage differs slightly according to region and the financial situation of the local government.
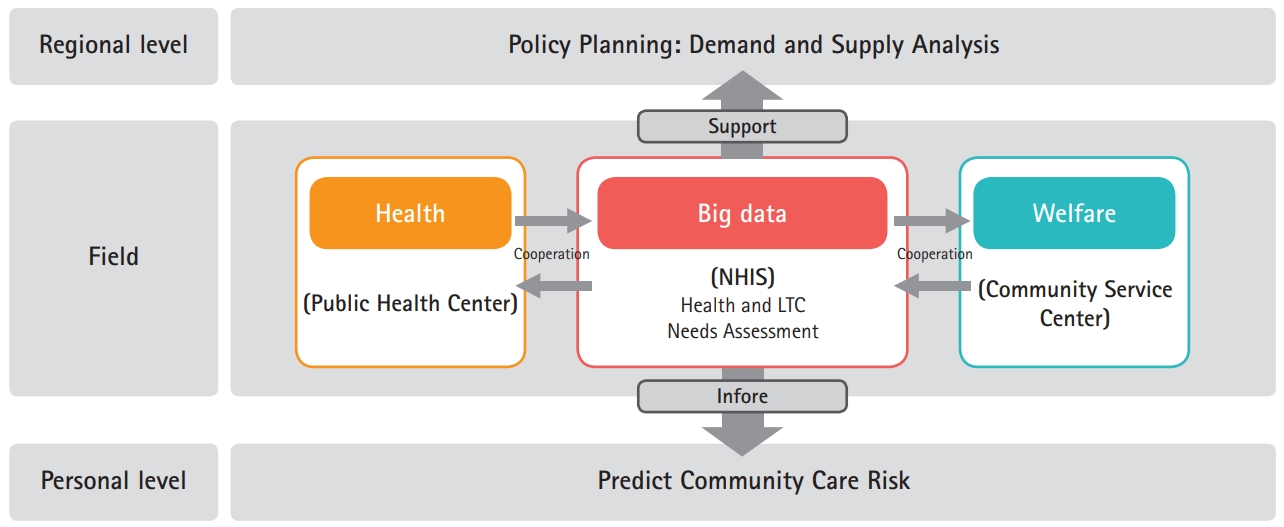
In the regions in which the CC pilot project was implemented, local governments reported difficulties in finding and assessing the care needs of potential care consumers. The NHIS supports the local governments to provide a potential pool of the people who require care, with privacy agreements based on big data analysis. The NHIS has big data on insurance benefits and collecting contributions. Social workers, sometimes along with nurses, at community service centers in the pilot project regions have developed the “Tonghapdolbomchangu” (“a gateway for integrated care”) for CC. They visit senior citizens’ homes and assess their care needs in person. Assessing care needs requires significant time and effort by care coordinators, especially for vulnerable persons with complex health problems and welfare issues in the community. The development of a pre-screening system to identify potential high-risk older populations as targets for CC will help local authorities implement CC.
The coronavirus disease 2019 (COVID-19) outbreak has changed the policy environment. Particularly, given the difficulties of in-person service, contact-free work is required even in the fields of health and long-term care. The primary assessment of service targets on the basis of big data analysis can complement the assessment through home-visits and can also make investigation of complex care needs easier and safer. Criticism from experts and professionals is that the criteria and standards for providing CC services in different pilot regions vary by region and are not validated. These problems might stem from insufficient experience with national and local care services among governmental officials in the community and the lack of guidelines and formal standards of community care from the headquarters.
As a single government insurer of the NHI and LTCI systems, the NHIS now has enormous data sets to identify the economic status, health, and long-term care needs of general citizens. These include data on the insured and contributions, health screening, medical care institutions and treatments, deaths and new-born reports, cancer registration, rare diseases, and long-term care needs assessment. CC assessment using big data in the NHIS can lessen the burden of identifying people who require CC, shorten assessment time, and increase the accuracy of assessment results in a single visit. An NHIS internal analysis confirmed that 19 of 23 items could assess CC needs through NHIS data without in-person contact. This could also be an effective contact-free working method to meet social demands. The NHIS has long-term experience in dealing with data and with standardized assessment and management of the long-term care needs of older people for LTCI beneficiaries. Centering the CC system on NHIS data, which plays a main role in the CC delivery system with the local government could be an effective and realistic model to fit the Korean environment. Citizens can be assessed and can access CC without losing benefit, even if they move to another region. It could also provide a means for easy involvement of various healthcare experts. With regard to the use of NHIS data, there is a negative opinion about the NHIS being centered on the CC data platform, but, it is a waste of time and money to set up a new organization even if there is a pre-existing organization. Additionally, the Health Insurance Research Institute of the NHIS could support local and central governments in developing CC plans through the analysis of accumulated health and long-term care data. Citizens could also be informed and encouraged to participate in healthcare management and practice healthy behaviors to prevent future frailty (Fig. 1).
Most people who require CC are older. They live their lives in long-term care settings with chronic conditions; thus, health and long-term care services must be the major parts of CC provision. The CC delivery system should comply with healthcare and long-term care systems and also be culturally acceptable to most Korean citizens and relevant stakeholders. Moreover, it should be a system for future generations and not just present seniors. A comprehensive design considering the Korean healthcare system’s strengths, weaknesses, and uniqueness is essential to establish the K-Community Care System. The big data accumulated by the NHIS as a single national insurer have significant potential for utilization in connecting CC with selecting service targets, recommending care services, and performing outcome evaluations. A CC model incorporating the NHI big-data system in Korea will be the best example for neighboring countries.